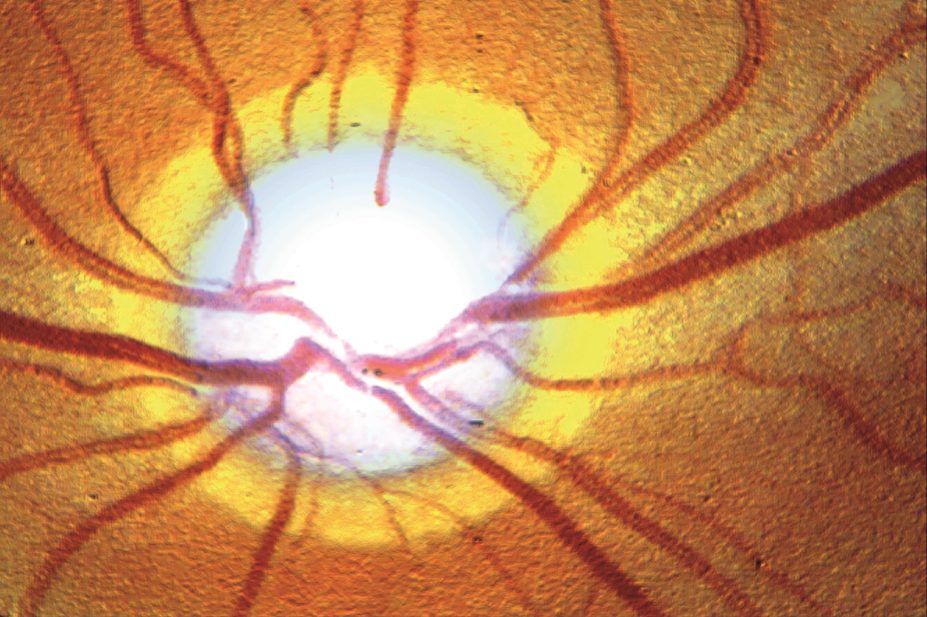
BSIP SA / Alamy
Summary
Reducing intra-ocular pressure (IOP) is the only treatment strategy with good evidence of clinical effectiveness in open angle glaucoma. There is no specific target for lowering IOP; the target and monitoring interval varies according to the severity of the disease and risk of progression.
Prostaglandin analogues include latanoprost, tafluprost and travoprost. These, in addition to bimatoprost (a prostamide), are usually used as first-line treatment because they are the most effective IOP-lowering agents, do not cause systemic side effects, are well tolerated and are used once a day.
The treatment of choice in children is surgery, as long-term pharmacological treatment is not practical. Ocular antihypertensive drugs are not generally used in children.
The European Glaucoma Society (EGS) states the aim of treatment in glaucoma is to “maintain the patient’s visual function and related quality of life, at a sustainable cost”. Cost is defined as inconvenience and adverse effects, as well as financial considerations[1]
.
It is important that patients have individualised treatment targets[2]
. Patients with chronic open angle glaucoma (OAG), suspected OAG and ocular hypertension (OH) should have a personalised management plan and need to be monitored at intervals according to their risk of progressive loss of vision. The National Institute for Health and Care Excellence (NICE) recommends monthly to two-monthly check-ups for patients with high risk of progression and poor intra-ocular pressure (IOP) control, and up to 12 months for patients at low risk of progression with IOP at target level[2]
. It is also important to treat patients holistically. For example, regular monitoring with no active treatment may be the best option for elderly patients with mild glaucoma, low risk of progression and significant co-morbidities[3]
.
Reducing IOP is the only treatment strategy with good evidence of clinical effectiveness. Research into drugs influencing ocular blood flow or neuroprotective agents has so far not shown any evidence of benefit[1]
.
There is no specific target for lowering IOP; the target and monitoring interval varies according to the severity of the disease and risk of progression. For example, a patient who has shown disease progression and with an IOP greater than the established target requires a change in treatment plan and monitoring every one to two months, whereas a patient with no progression with an IOP within the set target requires no change in plan and monitoring can be extended to every 6–12 months[4]
.
When choosing a target IOP the following factors should be considered: life expectancy; initial glaucoma damage; rate of progression; likelihood of vision loss; status of the other eye; patient preference; any additional risk factors; and adverse effects of treatment[1]
.
Currently, pharmacological treatment is used first-line unless the patient presents with sight-threatening IOP. Glaucoma in children is usually treated by surgery[1],[3]
.
It is important that all patients with glaucoma attend regular follow-up clinics. In the UK in 2009, the then-National Patient Safety Agency (NPSA) issued a rapid response alert that cited 44 cases of patients who experienced deterioration in vision, including 13 reports of total vision loss, attributed to delayed follow-up appointments. The NPSA required NHS organisations to review their processes to minimise the risk of avoidable sight loss by ensuring robust booking systems are in place, which respond to clinical priorities and can flag up high-risk patients, especially those not attending follow-up clinics[5]
.
Pharmacological treatment
Ocular hypotensives (e.g. prostaglandin analogues, beta-blockers, alpha-adrenergic agonists and carbonic anhydrase inhibitors) act either to reduce the production of intra-ocular fluid, increase the outflow, or a combination of both.
Two trials established the role of IOP-lowering drugs in the treatment of primary OAG. The Collaborative Normal Tension Glaucoma Study (CNTGS) treated patients with normal tension glaucoma and found that progression occurred in 17% of eyes treated with IOP-lowering drugs compared with 35% treated with placebo (after correction for increased incidence of cataracts in the treatment group)[6]
. In the Early Manifest Glaucoma Trial (EMGT), which involved patients with previously untreated glaucoma, a 25% decrease in IOP from baseline showed a 10% reduced risk of progression for every 1mmHg lowered, compared with the placebo group.
A trial published in The Lancet comparing latanoprost with placebo over two years showed a statistically significant visual field preservation in the treatment group[7]
.
A meta-analysis of randomized controlled trials found the greatest reduction of IOP was achieved by the prostaglandin analogues, followed by non-selective beta-blockers, alpha-adrenergic agonists, selective beta-blockers and finally topical carbonic anhydrase inhibitors[1]
.
The least amount of medicines to achieve the desired result should be used. Both the EGS and NICE guidelines recommend monotherapy. If the first medicine tried does not bring the IOP to the required target, or the patient does not tolerate the treatment, then the EGS guidelines suggest change to another monotherapy. This can even include swapping to another prostaglandin analogue, as there are reports that patients who do not respond to one prostaglandin analogue may respond to another.
If the target is not reached with monotherapy but the patient is tolerating the drug and there has been some decrease in IOP, a second drug is added[1],[4]
. Combination drops are generally used to improve adherence and decrease the amount of preservatives to which the patient is exposed (see ‘Ocular surface disease’).
Ocular surface disease
Benzalkonium chloride is often used as a preservative in eye drops. It is a highly effective antimicrobial but it can damage the ocular surface of the eye, producing conjunctival inflammation, tear film instability, and corneal cytotoxicity. This is called ocular surface disease.
Intermittent use of preserved drops in healthy eyes is unlikely to be a problem, but glaucoma patients tend to have a higher prevalence of ocular surface disease than the normal population, but it is not clear if this is linked to glaucoma or exacerbated by the chronic use of preserved eye drops[8]
. Therefore, reducing the preservative load is important for patients receiving long-term therapy. This can be done by the use of combination products (reducing the number of drops used) or using a mixture of preserved and preservative-free products to reduce the preservative load. Preservative-free products are not used in all patients because of cost, storage, and as some unit doses are more difficult to instil.
Newer, less toxic preservatives (e.g. Purite) are available but they tend to be found in medical devices, have no monographs and are linked to specific manufacturers by patents. The Alcon brand uses polyquad in Travatan and Duo-Trav, which appears to be less irritating than benzalkonium chloride[9]
.
Multi-dose devices for preservative-free drops are available. At the moment these products tend to be limited to lubricants and are classified as medical devices. However, these devices may be adopted in the future for licensed ophthalmic medicines[10]
.
Prostaglandin analogues include latanoprost, tafluprost and travoprost. These, in addition to bimatoprost (a prostamide), are usually used as first-line treatment as they are the most effective IOP-lowering agents, do not cause systemic side effects, are well tolerated and are used once a day[1],[3]
.
Prostaglandin analogues act by increasing uveoscleral outflow. Reduction in IOP starts two to four hours after first administration, with the effect reaching its peak after 8–12 hours. The circadian rhythm of IOP pressure increases during the night and peaks in the morning; therefore the drops should be instilled at night to produce a maximum effect the following morning. Prostaglandin analogues also reduce the IOP fluctuation during the 24-hour period, with a maximum effect achieved three to five weeks after starting therapy[11]
.
Bimatoprost is thought to have a dual action, increasing outflow through both the trabecular meshwork and the uveoscleral route. Several trials suggest bimatoprost is more effective in lowering IOP than the other prostaglandin analogues, although other trials show no difference[12],[13],[14]
.
The main side effects of prostaglandin analogues and prostamides are eye redness, which usually subsides with continual treatment (the highest incidence is reported with bimatoprost 300μg/ml)[14]
; increased pigmentation of the iris (more noticeable in patients with hazel-coloured eyes); and peri-orbital tissue fat atrophy and pigmentation[15]
. They also cause eyelash growth, and cases of cystoid macular oedema and uveitis have been reported.
Prostaglandin analogues and prostamides are contraindicated in uveitis as they may make the inflammation worse by enhancing the breakdown of the blood-aqueous humour barrier; however, they are sometimes used in patients with stable, well controlled uveitis. They are also contraindicated in patients with prior history of significant ocular viral infection (e.g. herpes simplex) because they may cause reactivation of the infection[1],[3],[11]
.
Prostaglandin analogues and prostamides are available as combination products with timolol as they have additive effects with beta-blockers; these combination products are used as second-line therapy providing the patient has no contraindications.
Latanoprost, bimatoprost and tafluprost are available as preservative-free formulations. A preservative-free tafluprost/timolol combination treatment is also due to be launched in 2015.
Formulations of bimatoprost 300µg/ml have a lower concentration of benzalkonium chloride than the 100µg/ml (0.05mg/ml compared with 0.2mg/ml), as the lower strength bimatoprost needs the addition of benzalkonium chloride to allow adequate drug penetration. A trial comparing bimatoprost 100µg/ml and 300µg/ml showed equivalence in decreasing IOP and improved tolerability[16]
.
Topical beta-blockers
(e.g.
timolol, betaxolol, carteolol, levobunolol) were, until recently, the treatment of choice for glaucoma. NICE recommends them as first-line therapy for OH in patients aged under 60 years with a medium central corneal thickness
[2]
. However, this guidance was issued before the availability of generic latanoprost, which may change future guidelines.
Beta-blockers, generally used twice daily, reduce the production of aqueous humour and tend to be more effective during the day than at night[1],[11]
. They decrease IOP by around 25%, but there have been reports of patients developing tolerance.
Timolol is found in many combination products, including prostaglandin analogues (see above), brimonidine, brinzolamide and dorzolamide. It is also available as a once daily formulation. Timolol, betaxolol and levobunolol are available in preservative free products.
The main disadvantage of beta-blockers is that they can cause systemic side effects, including wheezing, dysponea, bronchospasm, bradycardia and hypotension. They are contraindicated in patients with bronchial asthma, severe chronic obstructive pulmonary disease, bradycardia, severe heart block or overt cardiac failure. Ocular side effects include blepharoconjunctivitis and dry eyes. Contact dermatitis can arise from overflow of the drops on to the skin[11]
.
Betaxolol exhibits relative specificity for B1 receptors and produces less effect on pulmonary function. However, it is less effective in reducing IOP than timolol, and some respiratory physicians caution against the use of any beta-blocker in patients with pulmonary disease[11]
.
Alpha-adrenergic agonists used in glaucoma include brimonidine and apraclonidine.
Brimonidine is a selective alpha2-adrenoceptor agonist. It has a dual action, reducing aqueous production and increasing outflow via the uveoscleral pathways. It is less effective than latanoprost, but comparable in efficacy to timolol. It is licensed as monotherapy for patients in whom beta-blockers are contraindicated, or as an add-on therapy for patients whose IOP target has not been met.
Brimonidine was found to cause an allergic reaction (including blepharitis, blepharoconjunctivitis and conjunctival follicles)[11] in up to 12.7% of patients in clinical trials (causing withdrawal in 11.5% of subjects), with an onset after three to nine months in the majority of patients. It is contraindicated in patients taking monoamine oxidase inhibitors, and close monitoring is required in patients with depression, cerebral or coronary vascular insufficiency, Raynaud’s phenomenon, orthostatic hypotension or thromboangiitis obliterans. A combination of brimonidine and brinzolamide is also available.
Apraclonidine 0.5% is licensed in the UK for short-term use as an add-on therapy for glaucoma, as evidence suggests it is only effective on a long-term basis in around a third of patients[11]
. The 1% strength is licensed in the UK for the control or prevention of post-surgical elevations in IOP after anterior segment laser surgery.
Carbonic anhydrase inhibitors (CAIs) prevent catalysation of water and carbon dioxide to form bicarbonate, an essential component of aqueous humour production.
There are two commercially available topical CAIs in the UK: dorzolamide and brinzolamide. The CAI acetazolamide is taken orally or by intravenous injection. Topical CAIs are less effective at lowering IOP than acetazolamide (20% compared with 40% reduction in IOP), but have far fewer side effects[1],[11]
. They suppress the production of aqueous humour both during the day and at night. Dorzolamide is more irritating to the eye than brinzolamide, which may be a result of its lower pH.
Acetazolamide is now mainly used for short-term treatment (e.g. peri-operatively to prevent IOP spikes or for acute angle closure) on account of its risk of side effects and the availability of topical CAIs.
All commercially available CAIs are sulphonamides. There is significant structural difference between the antibacterial sulphonamide drugs and those used to treat glaucoma, and little evidence to suggest sensitivity overlapping; nevertheless, they are still contraindicated in patients with known hypersensitivity to sulphonamides[11]
.
Pilocarpine facilitates the outflow of aqueous humour by contraction of the ciliary muscles and traction on the trabecular meshwork. It is rarely used for chronic OAG because of the frequency of application required (four times a day) and its side effects, which includes accommodation spasm (prolonged contraction of the ciliary muscles keeping the eye in a state of myopia). Pilocarpine also causes miosis (closure of the eye) and is contraindicated in patients with uveitis[11]
.
Drugs in development include rho kinase (ROCK) inhibitors. ROCK plays a role in regulating the contractile tone of smooth muscle tissue; inhibiting this kinase causes cells in the trabecular meshwork and adjacent to the inner wall of Schlemm’s canal to shrink, creating space for aqueous humour drainage.
Rhopressa is a ROCK and norepinephrine inhibitor that targets the trabecular meshwork. It is currently undergoing phase III clinical trials in Canada. AMA0076 is a ROCK inhibitor also undergoing clinical trials[17]
.
Latanoprostene bunod is a nitric oxide-donating prostaglandin analogue currently in development, which appears to be more effective than latanoprost.
Surgery
NICE recommends that surgery is indicated in individuals with chronic OAG who[4]
:
- Are at risk of progressing to sight loss despite treatment;
- Do not respond to therapy;
- Are non-compliant with pharmacological treatment, or have a significant chance of not complying with treatment.
Trabeculectomy or filtration surgery is the most commonly performed incisional surgical procedure to lower IOP. A “guarded fistula” is produced between the anterior chamber and sub-conjunctival space, which provides an alternative path for the escape of aqueous humour. As fluid flows through the channel, the tissue over the opening rises up to form a bleb (blister).
Success rates of up to 90% have been reported, although some patients may require further therapy or another operation[1],[3]
. Long-term side effects of trabeculectomy include accelerated progression to senile cataracts and a slightly increased risk of bleb associated endophthalmitis (0.45–1.3%), which can be sight threatening[18]
.
The main complication of trabeculectomy is fibrosis of the episcleral tissue leading to closure of the new drainage pathway. This is more common in young people, those of African or Hispanic ethnicity, patients with inflammatory eye conditions and patients who have had previous intraocular surgery.
Fibrosis is reduced if surgery is supported with mitomycin C 0.2mg/ml or 0.4mg/ml or 5-fluorouracil 5mg/0.2ml. Both are unlicensed preparations but their use is standard practice in glaucoma. They are administered on either filter paper or a sponge (for one to five minutes with mitomycin C, and at least five minutes for 5-fluorouracil) to the ocular wound bed, then rinsed off with 20ml of balanced salt solution. They can be administered adjacent to the bleb via a small calibre needle post-operatively.
It is important neither mitomycin C nor 5-flurouracil enters the eye as they can cause irreversible endothelial damage[1]
. They are both cytotoxic agents and their disposal should follow normal cytotoxic protocols.
Long tube drainage devices are reserved for patients at increased risk of poor outcomes following surgery[1]
.
Laser trabeculoplasy is used in OAG. It involves laser burns to the trabecular meshwork, and has been found to facilitate aqueous outflow. It can achieve substantial IOP reductions but the effect gradually decreases over time with an absolute failure rate of 10% each year[3]
. It can be used to avoid or delay surgery[1]
.
Treatment for special groups
The treatment of choice in children is surgery, as long-term pharmacological treatment is not practical[1]
. Ocular antihypertensive drugs are not generally used in children. Prostaglandin analogues are less effective in children (although latanoprost and travoprost now have a paediatric licence in the UK), and alpha-adrenergic agonists are contraindicated in young children. This leaves carbonic anhydrase inhibitors or beta-blockers as treatment options, subject to licence restrictions.
There is little safety evidence regarding the use of ocular antihypertensives in pregnancy. However, so far there appear to be few reports of anti-glaucoma medicines causing harm. The EGS guidelines suggest timolol 0.1% gel (the lowest concentration available), used once a day, may be an option to treat glaucoma in pregnant women. Prostaglandin analogues can theoretically increase uterine contractibility in pregnancy, and should be discontinued if the patient shows any signs of premature labour. Laser trabeculoplasty may be an alternative to drug treatment[1]
.
Hormonal changes caused by pregnancy can lower IOP, especially during the third trimester and for several months after delivery. Therefore, it may be possible to discontinue medicines during pregnancy with careful monitoring. If medicines are continued, the lowest effective dose should be used and systemic absorption should be reduced by punctal occlusion (gently pressing on the tear duct next to the nose through which tears drain) and blotting away excess drops.
The American Academy of Paediatrics recommends that beta-blockers and carbonic anhydrase inhibitors are safe to use in breastfeeding[1]
.
Support for patients
A 2014 survey by the International Glaucoma Association found[19]
:
- 45% of patients had not been instructed on how to use their eye drops;
- 91% of patients were not assessed on their ability to use eye drops;
- 50% of patients were not aware they should practice punctal occlusion;
- 9% of patients had been given any information on compliance aids to help use their eye drops;
- 45% of patients had been given no information on the Driver and Vehicle Licensing Agency’s driving regulations regarding glaucoma;
- 32% had not been told glaucoma can be hereditary and first-degree relatives aged over 40 years are entitled to a free eye test;
- On diagnosis, 31% of people said they were not given sufficient information to understand their condition.
Patient found ophthalmologists, optometrists and ophthalmic nurses a very good source of information. However there was a distinct lack of support from GPs and pharmacists.
Advice for patients
Only around 5% of an eye drop will enter the eye; the rest will run down the cheek or be drained through the nasolacrimal duct (or lacrimal punctum). Once in the eye, spontaneous tear flow will wash out a drop after five minutes. Addition of a second drop 30 seconds later will result in almost 50% of the first drop being washed out. It is important that there is a minimum of five minutes between different drops.
This loss of dose can be reduced by punctal occlusion (gently pressing on the tear duct next to the nose). Patients should also be advised to shake eye drop bottles before use to ensure adequate mixing, as microparticles can settle towards the bottom[1]
.
Glaucoma is a chronic disease and there has always been a problem with adherence with treatment. Non-adherence has remained constant over the past 25 years, with rates estimated at 30–70%. Factors that affect adherence include sex (men are less compliant), stage of disease (those with early disease are less adherent), understanding of the disease, side effect of drugs, and lifestyle[1]
.
Suggestions to improve compliance include the use of simple regimens (no more than two bottles and no more than twice-daily administration) and advice on how to incorporate eye drop administration into daily routines.
It is important that patients are given instructions on how to administer the eye drops, and that their technique is evaluated. Joining an organisation such as the International Glaucoma Association can provide support and education.
Patients with glaucoma may be able to continue driving, provided they have no other problems (e.g. cataracts) and loss to the visual field is not advanced. However, patients with glaucoma in both eyes in the UK must inform the Driver and Vehicle Licensing Agency (DVLA) and complete an online form, or they could be fined up to £1,000. If necessary, the DVLA may request visual acuity and field tests to assess whether a patient is safe to drive.
Elaine Mann is an ophthalmic, ENT, maxillofacial and dental pharmacist at Leeds Teaching Hospitals NHS Trust.
References
[1] European Glaucoma Society. Terminology and Guidelines for Glaucoma 4th Edition.
[2] National Institute for Health and Care Excellence. Glaucoma quality standard QS7.
[3] Weinreb RN. The Pathophysiology and treatment of glaucoma: a review. JAMA 2014;311(18):1901–1911.
[4] National Institute for Health and Care Excellence. Glaucoma: Diagnosis and management of chronic open angle glaucoma and ocular hypertension. London: NICE 2009.
[5] National Patient Safety Alert. Preventing delay to follow up for patients with glaucoma. 2009.
[6] Heijl A, Leske MC, Bengtsson B et al. Reduction of intraocular pressure and glaucoma progression: results from the Early Manifest Glaucoma Trial. Arch Ophthalmol 2002;120(10):1268–1279.
[7] Garway-Heath D, Crabb DP, Bunce C et al. Latanoprost for open angle glaucoma (UKGTS): a randomised, multicentre, placebo-controlled trial. The Lancet 2015;385(9975):1295–1304.
[8] Rosin L & Bell N. Preservative toxicity in glaucoma medication: clinical evaluation of benzalkinium chloride free timolol eye drops. Clinical Ophthalmology 2013;2013(7):2131–2135.
[9] Freeman PD & Kahook MY. Preservatives in topical ophthalmic medications: historical and clinical perspectives. Expert Rev Opthalmol 2009;41(1):59–64.
[10] Pisella PJ, Pouliquen P & Baudouin C. Prevalence of ocular symptoms and signs with preserved and preservative free glaucoma medication. Br J Ophthal 2002;86:418–423.
[11] Bartlett JD & Jaanus SD. Clinical ocular pharmacology 5th edition. Chicester: Elsevier 2008.
[12] Eyawo O, Nachega J, Lefebvre P et al. Efficacy and safety of prostaglandin analogues in patients with predominantly primary open-angle glaucoma or ocular hypertension: a meta-analysis. Clin Ophthalmol 2009;3:447–456.
[13] Cheng JW, Cai JP, Li Y et al. A meta-analysis of topical prostaglandin analogs in the treatment of chronic angle-closure glaucoma. J Glaucoma 2009;18:652–657.
[14] Honrubia F, Garcia-Sanchez J, Polo V et al. Conjunctival hyperaemia with the use of latanoprost versus other prostaglandin analogues in patients with ocular hypertension or glaucoma: a meta-analysis of randomised clinical trials. Br J Ophthal 2009;93(3):316–321.
[15] American Academy of Ophthalmology. Clinical Update: Glaucoma. What clinicians need to know about prostaglandin-associated Periorbitopathy.
[16] Katz LJ, Cohen JS, Batoosingh AL et al. Twelve-month, randomized controlled trial of bimatoprost 0.01%, 0.0125%, and 0.03% in patients with glaucoma or ocular hypertension. Am J Ophthalmol 2010;149:661–671.
[17] Karmel M. Glaucoma pipeline drugs: targeting the trabecular meshwork. American Academy of Ophthalmology. 2013
[18] Vaziri K, Kishor K, Schwartz SG et al. Incidence of bleb associated endophthalmitis in the United States. Clinical Ophthalmol 2015;9:317–322.
[19] International Glaucoma Association. IGA News Autumn 2014.


