Abstract
Aim
To determine the role of a pharmacy tool, the symptoms-check questionnaire, in supporting pharmacists’ recommendations for treatment with Flomax Relief MR (tamsulosin) and to assess its acceptability to men with lower urinary tract symptoms (LUTS) who present in a pharmacy to purchase tamsulosin.
Design
Two-part cross-sectional study in which pharmacist recommendations for tamsulosin in men with LUTS using the symptoms-check questionnaire were compared with “gold standard” recommendations (GP judgements together with the British Association of Urological Surgeons guidelines for LUTS, summary of product characteristics for Flomax Relief MR, and International Prostate Symptom Scores) to measure agreement and men’s experiences of purchasing tamsulosin, including completion of the symptoms-check questionnaire were assessed.
Subjects and setting
Suitability for tamsulosin was assessed in 181 men with lower urinary tract symptoms by 17 pharmacists and three GPs. Experiences of purchasing tamsulosin were evaluated in 89 men with lower urinary tract symptoms and further in-depth interviews conducted with 43 men.
Outcome measures
The primary outcome for assessing the role of the symptoms-check questionnaire in recommendation for tamsulosin was agreement between pharmacist and gold standard recommendations.
Results
Agreement between pharmacist and gold standard recommendations for tamsulosin in men with lower urinary tract symptoms was 92 per cent (agreement in 166 of 181 cases). Men who had purchased tamsulosin in pharmacy viewed the symptoms-check questionnaire as an indication that they were being thoroughly assessed. This resulted in a perception that pharmacists were professional and knowledgeable about lower urinary tract symptoms.
Conclusion
With the support of the symptoms-check questionnaire, pharmacists made appropriate recommendations for treatment with tamsulosin. Far from being a barrier to purchase in men with lower urinary tract symptoms, the symptoms-check questionnaire reassured them that tamsulosin was the right treatment for them and enhanced their perception of pharmacists’ professionalism and knowledge.
Benign prostatic hyperplasia (BPH) is a common age-related condition often associated with distressing symptoms. Estimates of the prevalence of BPH suggest one in four men over the age of 40 years will experience symptoms.1
Estimates vary between 26 per cent and 46 per cent in men aged 40 to 79 years depending on the way it is defined2–5 and histological changes in the prostate suggestive of BPH have been found in up to 70 per cent of 60- to 70-year-old men.6
Benign prostatic enlargement (BPE) is usually secondary to BPH, occurring in approximately 50 per cent of men with histological BPH.7 BPH and BPE are often associated with lower urinary tract symptoms such as urgency, hesitancy, dribbling, slow, erratic or frequent urination, frequent night time urination, inability to completely empty the bladder and urge incontinence. These symptoms used to be known as prostatism and can have a significant impact on quality of life affecting relationships, mood, emotional well-being and the ability to fulfil roles in men with mild to moderate symptoms and limiting the ability to work or perform daily living tasks in men with more severe symptoms.8
Alpha-1 adrenoceptor antagonists are effective treatments for the symptoms associated with BPH that work on the bladder neck, prostate and bladder and have been shown to increase maximum urinary flow rate by up to 25 per cent and improve symptoms by up to 40 per cent.9,10
To accompany the reclassification of the alpha-1 adrenoceptor antagonist tamsulosin from a prescription only medicine to a medicine available from community pharmacies, a questionnaire was developed for use by pharmacists to guide them in the appropriate use of tamsulosin (Flomax Relief MR). Development of the symptoms-check questionnaire, was a requirement of the licence for reclassification.
The questionnaire is designed to be completed by men who visit a pharmacy requesting help for symptomatic BPH or lower urinary tract symptoms and provides a checklist for pharmacists to structure the clinical assessment they would make of any customer requesting tamsulosin for BPH-related lower urinary tract symptoms as part of their usual clinical practice. An interpretation guide helps pharmacist identify the “red flags” and other contraindications to tamsulosin and to assess the customer’s suitability for treatment with tamsulosin.
The questionnaire was developed in an iterative process incorporating the summary of product characteristics for Flomax Relief MR, the views of specialist clinicians expert in the management of BPH, and couched in the language of men with BPH/lower urinary tract symptoms. It was tested in a pilot study with 58 men with lower urinary tract symptoms, six community pharmacists and three GPs to assess acceptability, comprehensibility and ease of use and to evaluate its ability correctly to identify clinical contraindications to treatment with tamsulosin (validity).
The aim of this study was to determine the role of a pharmacy tool (the symptoms-check questionnaire) in supporting pharmacists’ appropriate recommendations for treatment with tamsulosin. The study was designed to establish whether the tool could help pharmacists in making assessments and recommendations, and whether it was acceptable to and valued by men with lower urinary tract symptoms who presented in a pharmacy intending to buy tamsulosin.
Methods
A two-part study was undertaken. The first part occurred before the launch of Flomax Relief MR to demonstrate that by following a checklist, pharmacists would be assisted in appropriately recommending tamsulosin in a community setting.
The second part ran from the launch of Flomax Relief MR to capture the perceptions and experience of men with lower urinary tract symptoms who purchased tamsulosin in pharmacies, particularly in relation to their perceptions of pharmacists and their experience of purchasing tamsulosin in pharmacy.
Both parts of the study were cross-sectional and observational and were reviewed and approved by an independent research ethics committee, Reading Scientific Laboratories.
Part 1 — pre-switch
Participants
Men with symptomatic BPH or lower urinary tract symptoms were recruited through press and radio advertisements and their suitability for tamsulosin was assessed by pharmacists and GPs.
Eligible men were aged 40 years and over, either had a diagnosis of symptomatic BPH or were experiencing lower urinary tract symptoms, and could be using medicines for their lower urinary tract symptoms or be on no treatment. All the men gave written, informed consent.
Seventeen community pharmacists performed the patient assessments. Participating pharmacists had private consultation facilities within their pharmacies and received face-to-face training for the study. This training covered: the clinical rationale supporting the symptoms-check questionnaire, the contraindications and cautions relating to use of tamsulosin, specific training on the administration and interpretation of the symptoms-check questionnaire, and training in the study process and administration.
Three GPs performed the clinical consultations.
Setting
Pharmacy assessments took place in a naturalistic setting within community pharmacies. Pharmacies were selected from three different geographic locations around England (Birmingham, Hertfordshire and Kent). Where there were geographic barriers to accessing participating pharmacies, pharmacy assessments were conducted by telephone interview. All GP assessments were performed by telephone interview.
Study procedures
There were two stages to the study. In stage 1 participating men attended an assessment with a participating pharmacist or were telephoned by a participating pharmacist at an agreed time. At the assessment/telephone interview, subjects completed the symptoms-check questionnaire and the pharmacists used this, together with their clinical evaluation, as the basis of their assessment as to whether the man would be suitable for tamsulosin.
At stage 2, within 14 days of the pharmacy assessment, participating men were telephoned by a study GP, who performed a clinical assessment by telephone based on the sorts of questions they would usually ask in clinical practice. GPs were blinded to the responses on the symptoms-check questionnaire.
Both pharmacist and GP made independent judgements of suitability of the men for treatment with tamsulosin. GP judgements together with the British Association of Urological Surgeons guidelines for lower urinary tract symptoms,11 SPC for Flomax Relief MR, and international prostate symptom scores (IPSS)12 formed the gold standard of evaluation of suitability for tamsulosin against which pharmacist assessments were compared.
The symptoms-check questionnaire
The symptoms-check questionnaire completed by men in Part 1 is designed to help pharmacists ascertain suitability for treatment with Flomax Relief MR. In the questionnaire, assessment of severity of lower urinary tract symptoms and their impact on quality of life are assessed using the IPSS12 and the IPSS quality of life question.12
These are international, validated scales designed for self-completion by men with BPH and scores are used to determine whether pharmacological interventions are appropriate. The higher the symptom or quality of life score, the more frequent the symptoms and the greater the impact on quality of life.
Symptom scores of 8 or more, or symptom scores of 1 or more plus quality of life scores of 4 or more indicate that patients may benefit from pharmacological intervention. The symptoms-check questionnaire also includes questions about red flag symptoms and contraindications for alpha-1 adrenoceptor antagonists as a checklist or guidance for pharmacists.
Determining sample size
The sample size for Part 1 was based on the assumption that concordance between pharmacist and gold standard assessments of suitability (number of subjects where pharmacist and gold standard assessments of suitability or unsuitability agree/total number of subjects) would be 80 per cent. To estimate this with 95 per cent confidence intervals of width 10 per cent, 180–200 subjects were required.
Statistical analysis
All data were entered in an SPSS database and analysed by one of the authors (AJC). Descriptive statistics were used to describe the demographic and clinical background of men who participated in the study. The primary endpoint was agreement between pharmacist and gold standard assessments of suitability for tamsulosin (number of subjects where pharmacist and gold standard assessments of suitability or unsuitability agreed/total number of subjects). Agreement rates were estimated with 95 per cent confidence intervals. Confidence intervals were calculated using the large sample normal approximation to the binomial distribution.
Data were analysed using SPSS for Windows versions 14.0 and 18.0.
Part 2 — post-switch
Participants
Men with symptomatic BPH or lower urinary tract symptoms who had visited a pharmacy to purchase Flomax Relief MR were recruited via the Flomax Relief website and through telephone and online surveys. All men gave verbal informed consent.
Setting
Interviews with men who had purchased tamsulosin in a pharmacy were conducted by telephone.
Study procedures
Men who had purchased tamsulosin in a pharmacy were interviewed by telephone using a standardised questionnaire that captured feedback on their interaction with the pharmacist when they had visited the pharmacy with the intention of purchasing the medicine.
A convenience sample of around half of these men was subsequently interviewed in depth using open-ended questions to explore their perceptions of the relative roles and responsibilities of pharmacists and GPs in managing lower urinary tract symptoms and their feedback on use of the symptoms-check questionnaire.
All interviews were conducted with men after they had been into a pharmacy with the intention of purchasing tamsulosin.
Analysis
Data from the structured questionnaire were entered in an SPSS database and analysed by one of the authors (AJC). Descriptive statistics were used to describe the demographic and clinical background of men who participated in the study and feedback on their interaction with the pharmacist. The in-depth interviews were transcribed and analysed using content and thematic analysis.
Results
Part 1
Sample
One hundred and eighty-one men were recruited and completed both the pharmacy and GP assessments. The mean age of the sample of 181 men was 57.3 years (standard deviation 9.30, ranging from 40 to 87 years). Ninety-two per cent were white Caucasian. Twenty-four per cent had been previously diagnosed by their doctor as having benign prostatic hyperplasia. Nine men (5 per cent) were currently taking tamsulosin.
The mean IPSS was 17.7 (sd 7.30, range 3–35). Sixty-three per cent of men were dissatisfied, unhappy or thought their life was terrible as a result of lower urinary tract symptoms (IPSS quality of life question12); 27 per cent were ambivalent about the impact of their symptoms and 10 per cent reported a reasonable quality of life despite their symptoms. All except one subject had experienced symptoms for more than three months.
Appropriateness of pharmacist recommendations for treatment with tamsulosin
Concordance between pharmacist designations of suitability for tamsulosin and gold standard designation (a combination of current guidance, SPC for Flomax Relief MR, IPSS and clinical opinion) was 0.92 (95 per cent confidence intervals 0.88–0.96). This means that pharmacists’ recommendations for treatment with tamsulosin would agree with gold standard recommendations in 92 per cent of cases.
The five men whom pharmacists wrongly designated as suitable for tamsulosin (a false positive rate of 6 per cent) comprised:
- One man who reported pain on urination to the GP, but not on the pharmacy questionnaire (symptoms-check questionnaire)
- One man who was believed by the GP to have other conditions that required monitoring, but nothing was detected on the pharmacy questionnaire
- One man who was under urological review and on the pharmacy questionnaire reported cloudy urine and recent heart problems
- One man who was believed by the GP to have urinary symptoms attributable to other causes, but this was not apparent from the pharmacy questionnaire
- One man who was currently taking doxazosin and had reported this on the pharmacy questionnaire
The 10 men who were suitable for Flomax Relief MR, but had been designated unsuitable by the pharmacist (a false negative rate of 11 per cent), comprised:
- Six men who were deemed unsuitable by the pharmacist because their symptoms were too mild but their IPSS and quality of life scores were severe enough to qualify for treatment. These were all men whose symptom severity scores were greater than 7, but who reported little or no impact of symptoms on their quality of life.
- Four men for whom there was no clear reason why the pharmacist had deemed them unsuitable for treatment and who had no contraindications on the pharmacy questionnaire. All were clinically complex, with either diabetes or very severe IPSS symptom scores
Men took an average of 10 minutes to complete the questionnaire, depending on how much discussion was initiated with the pharmacist (sd 5.05, range 2–25min). The mean time taken for pharmacists to review and interpret the questionnaire was 3.79 minutes (sd 3.46, range 0.1–25min). In cases where the responses were straightforward and the pharmacist was familiar with the process, the time for interpretation was a matter of seconds.
The questionnaire had high sensitivity (89 per cent) and specificity (94 per cent).
Part 2
Sample
Eighty-nine men were recruited and interviewed for feedback about their pharmacy interaction and 43 of these participated in subsequent in-depth interviews about the role of pharmacists in managing urinary symptoms. Fifty-seven per cent of the men were aged 45 to 56 years, 43 per cent were aged 60 to 74 years. Ninety-six per cent were white Caucasian.
The mean IPSS score was 16.6 (sd 7.19, range 3–35). Seventy-five per cent of men were dissatisfied, unhappy or thought their life was terrible as a result of lower urinary tract symptoms (IPSS quality of life question12); 18 per cent were ambivalent about the impact of symptoms and 7 per cent reported a reasonable quality of life despite their symptoms.
Men’s experience of buying Flomax Relief MR in pharmacy
Of those men who had been into a pharmacy with the intention of purchasing tamsulosin, 39 (44 per cent) were happy to discuss their urinary symptoms with their pharmacist. Although 50 (56 per cent) said they would prefer to discuss their symptomswithaGP,theirexperienceof buying Flomax Relief MR in a pharmacy was generally positive. Most (n=76, 85 per cent) had found the pharmacist easy to access and had not found the consultation too time-consuming (n=80, 90 per cent) and 67 (75 per cent) thought there had been adequate privacy in which to discuss their symptoms. Most men (n=72, 81 per cent) reported that they believed their symptoms had been thoroughly assessed by the pharmacists who had provided useful information to 75 men (84 per cent) and had been able to answer all the questions of 71 men (80 per cent).
Men’s perceptions of the roles and responsibilities of pharmacists and the function of the symptoms-check questionnaire
When men are unwell, most (n=36, 82 per cent) seek advice about their illness from their GP, particularly where they think the symptoms represent a more serious illness or where symptoms have failed to resolve or have worsened. They see the pharmacist’s role as providing advice about minor ailments such as coughs and colds and dispensing or selling medicines.
Although they would be happy to discuss minor ailments with pharmacists, most would prefer to discuss what they see as more personal health issues with a GP. This preference seems to be as much to do with concerns about privacy as perceptions of professional roles and responsibilities; men said that although they would prefer not to discuss personal issues with a pharmacist, they would do so if there was adequate privacy (such as a separate consulting room). Moreover, despite urinary symptoms being seen as a personal issue, men who had purchased Flomax Relief MR in a pharmacy had specifically gone to the pharmacist rather than their GP for advice about how to manage their symptoms.
Professional competence was important in determining the value men attached to the advice they received and whether it guided their treatment decisions. For men who had purchased Flomax Relief MR in a pharmacy, interaction with the pharmacist had reassured them of the pharmacist’s professional competence and knowledge around urinary symptoms to the extent that their expectations of the roles of pharmacists were modified. In this instance men were happy to receive advice from pharmacists about their urinary symptoms because they seemed knowledgeable and professional and there was a perception that they had been specially trained.
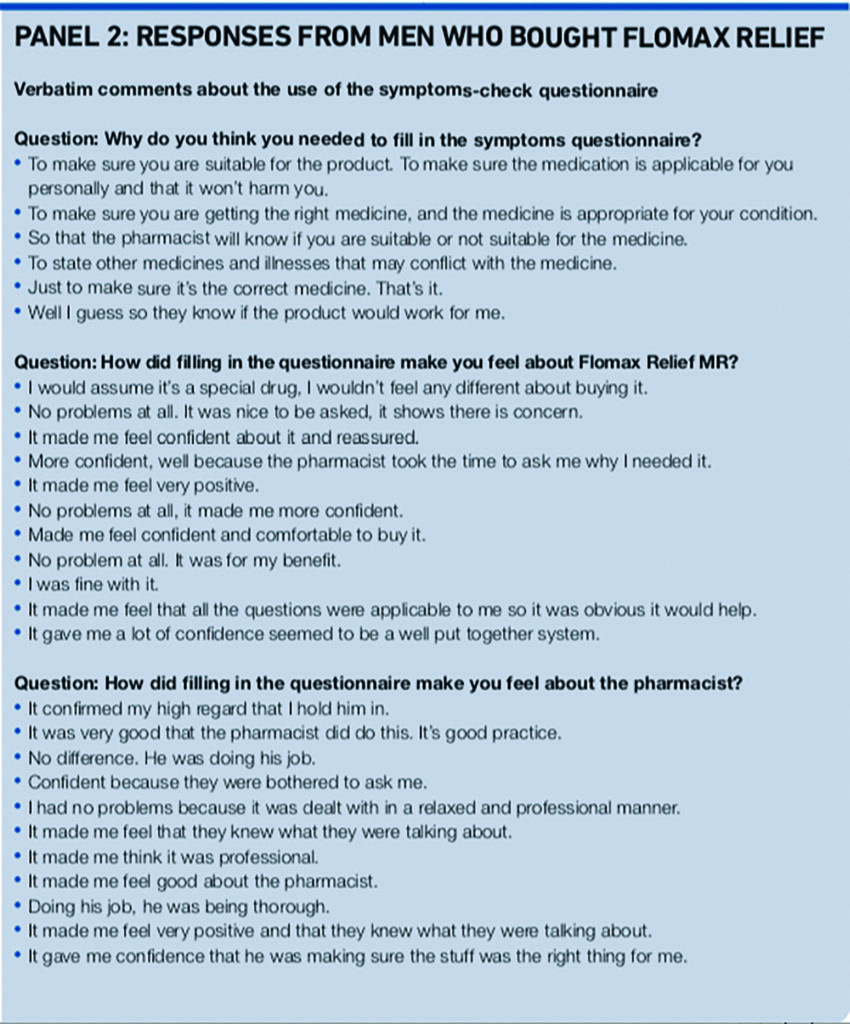
This was reinforced by the use of the symptoms-check questionnaire. Men viewed the questionnaire as a tool to help the pharmacist assess whether tamsulosin was the right treatment for them personally and this either reassured them that the pharmacist’s advice was professional and based on specific, thorough knowledge about them and their symptoms or had no detrimental effect on their feelings about the pharmacist or tamsulosin (Panels 1 and 2). Men did not want to receive information or advice about their urinary symptoms from pharmacy assistants, whom they did not consider to be sufficiently qualified to provide it.

The pharmacy consultation provided most men (n=35, 83 per cent) with all the information they believed they needed to manage their urinary symptoms and they planned to see their GP only because they are required to do so within six weeks of starting to take Flomax Relief MR or because they wanted a prescription.
Discussion
The results of this study demonstrate pharmacists’ professional competence in the appropriate recommendation of a product recently reclassified from a prescription-only medicine to available for purchase in pharmacy. Not only are pharmacists’ recommendations appropriate, but customers also perceive pharmacists as being professionally competent and are reassured by their knowledge and advice.
Both these findings are to some extent the result of the tool that was developed to guide pharmacists’ recommendations for the use of Flomax Relief MR. This tool, the symptoms-check questionnaire, acts as a checklist to enable pharmacists to identify red flag symptoms and contraindications in addition to establishing that symptoms are sufficiently severe to warrant pharmacological treatment.
Using this tool, pharmacists made recommendations for tamsulosin that concurred with gold standard recommendations in 92 per cent of men with lower urinary tract symptoms. Use of this tool in clinical practice in pharmacy reassures men who are considering purchasing tamsulosin that they have been thoroughly assessed and that pharmacists will base their recommendation on what is right for that individual as well as reinforcing the professional role and competence of the pharmacist.
A role for pharmacists in managing a chronic condition such as lower urinary tract symptoms through advice and recommendation of a reclassified medicine, reflects recent changes in the professional boundaries of their role away from dispensing towards a more patient-oriented role that is congruent with current health policy13–16 and includes the provision of health information, advice about self-management and strategies to help patients use their medicines effectively.17
For the evolution of their role to be successful, pharmacists need to feel confident within their new professional boundaries, GPs need to understand and support the expanded role and the services pharmacists can offer, and patients and consumers need to see the pharmacist as someone who has the professional qualifications and skills to support them in self-management or medicine-taking.18–19
The evidence from this study suggests that with training and guidance, pharmacists are professionally competent to advise patients on the self-management of lower urinary tract symptoms and that consumers view them as adequately trained and qualified for this role.
This echoes previous research in which pharmacists were perceived as providing a valuable role in advice and information about healthcare and taking medicine20–23 and contradicts studies in which patients have reported low expectations of pharmacists.24 Pharmacists themselves have reported feeling undervalued. Greater involvement in the management of chronic conditions through reclassification of prescription only medicines can potentially provide an opportunity for pharmacists to use their skills in a more extended, challenging and satisfying role.
Declarations
This study was funded by Boehringer Ingelheim, which holds the marketing licence for Flomax Relief MR. It was carried out independently by Hamell, an independent healthcare research company, which designed and ran the study, wrote the protocol and analysed the results. Hamell received payment from Boehringer Ingelheim for the day-to-day costs incurred in running the study. Professor Kirby and Mr Phillips were reimbursed for the time they gave to the study at British Medical Association agreed rates.
About the authors
Michael Kirby, MBBS, FRCP, is visiting professor at the Faculty of Health & Human Sciences, Centre for Research in Primary & Community Care, University of Hertfordshire
Graham Phillips, DipCommPharm, FRPharmS, is a community pharmacist at Manor Pharmacy (Wheathampstead) Ltd, Wheathampstead
Alison Carr, PhD, is epidemiologist and clinical director at Hamell, London
Correspondence to: Dr Alison Carr, Hamell, Shakespeare House, 168 Lavender Hill, London, SW11 5TG (email alison.carr@hamell.co.uk)
References
- Simpson RJ, Lee RJ, Garroway WM, King D, McIntosh I. Consultation patterns in a community survey of men with benign prostatic hyperplasia. British Journal of General Practice 1994;44:499–502.
- Jacobsen SJ, Germain CJ, Lieber MM. Natural history of benign prostatic hyperplasia. Urology 2001;58(Suppl 6A):5–16.
- Garraway WM, Collins GN, Lee RJ. High prevalence of benign prostatic hypertrophy in the community. Lancet 1991;338:469–71.
- Guess HA. The prevalence of benign prostatic hyperplasia in population surveys. In: Garroway M (editor). Epidemiology of prostate disease. Berlin: Springer–Verlag, 1995; pp121–31.
- Hunter DW, McKee CM, Black N, Sanderson CFB. Urinary symptoms: prevalence and severity in British men aged 55 and over. Journal of Epidemiology and Community Health 1994;48:569–75.
- Lynch TH, Waymount B, Beacock CJ, Dun nJA, Hughes MA, Wallace DM.Follow up after transurethral resection of the prostate: who needs it. BMJ1991;302:27.
- Abrams P. New words for old: lower urinary tract symptoms for“prostatism”. BMJ 1994;69:929–30.
- Welch G, Weinger K, Barry MJ. Quality of life impact of lower urinary tractsymptom severity: results from the health professionals’ follow-up study. Urology 2002;59:245–50.
- Djavan B, Marberger M. A meta-analysis on the efficacy and tolerability ofalpha1-adrenoreceptor antagonists in patients with lower urinary tract symptoms suggestive of benign prostatic obstruction. European Urology 1999;36:1–13.
- Eri LM, Tveter KJ. Alpha-blockade in the treatment of symptomatic benign prostatic hyperplasia. Journal of Urology 1995;154:923–34.
- Speakman MJ, Kirby RS, Joyce A, Abrams P, Pocock R (The British Association of Urological Surgeons). Guideline for the primary care management of male lower urinary tract symptoms. BJU International 2004;29:985–90.
- Barry MJ, Fowler FJ, O’Leary MP, Briskewitz RC, Holtgrewe HL, Mebust WK et al. The American Urological Association Symptom Index for Benign Prostatic Hyperplasia. Journal of Urology 1992;148:1549–57.
- Wong L, Campion P, Coulton S, Cross B, Edmondson H, Farrin A. Pharmaceutical care for elderly patients shared between community pharmacists and general practitioners: a randomised evaluation. RESPECT (Randomised Evaluation of Shared Prescribing for Elderly people in the Community over Time). BMC Health Services Research 2004;4:11.
- Vu T, Harris A, Duncan G, Sussman G. Cost-effectiveness of multidisciplinary wound care in nursing homes: a pseudo-randomized pragmatic cluster trial. Family Practice. 2007;24:372–9.
- Bell JS, Whitehead P, Aslani P, Sacker S, Chen TF. Design and implementation of an educational partnership between community pharmacists and consumer educators in mental health care. American Journal of Pharmaceutical Education 2006;70:28.
- Sorensen L, Stokes JA, Purdie DM, Woodward M, Elliott R, Roberts MS. Medication reviews in the community: results of a randomized, controlled effectiveness trial. British Journal of Clinical Pharmacology 2004;58:648–64.
- Austin Z, Gregory PAM, Martin JC. Negotiation of interprofessional culture shock: the experiences of pharmacists who become physicians. Journal of Interprofessional Care 2007;21:83–93.
- While A, Shah R, Nathan A. Interdisciplinary working between community pharmacists and community nurses: the views of community pharmacists. Journal of Interprofessional Care 2005;19:164–70.
- Muijrers PEM, Knottnerus JA, Sijbrandij J, Janknegt R, Grol R. Changing relationships: attitudes and opinions of general practitioners and pharmacists regarding the role of the community pharmacist. Pharmacy World and Science 2003;25:235–41.
- Bajramovic J, Emmerton L, Tett SE. Perceptions around concordance — focus groups and semi-structured interviews conducted with consumers, pharmacists and general practitioners. Health Expectations 2004;7:221–34.
- Du Pasquier S, Aslani P. Concordance-based adherence support service delivery: consumer perspectives. Pharmacy World and Science 2008;30:846–53.
- Bell JS, Aslani P, McLachlan AJ, Whitehead P, Chen TF. Mental health case conferences in primary care: content and treatment decision making. Research in Social and Administrative Pharmacy 2007;3:86–103.
- Clark AM, McMurray JJV, Morrison CE, Murdoch DL, Capewell S, Reid M. A qualitative study of the contribution of pharmacists to heart failure management in Scotland. Pharmacy World and Science 2005;27:453–8.
- Hassell K, Noyce P, Rogers A, Harris J, Wilkinson J. Advice provided in British community pharmacies: what people want and what they get. Journal of Health Services Research and Policy. 1998;3:219–25.


