This content was published in 2004. We do not recommend that you make any clinical decisions based on this information without first ensuring you have checked the latest guidance.
For more recent content on this topic, please see:
The previous article in this series (PJ, 3 April p419–21), looked at general blood tests requested from haematology departments, such as full blood counts. Blood tests are used to investigate many aspects of health and disease. Some tests are done routinely, for example, tests for blood type and phenylketonuria in new-born babies.
Another example is when a patient has a suspected myocardial infarction. His or her levels of cardiac enzymes, such as creatine kinase (especially the MB isoenzyme) and troponin T, will be determined and this information will be used (in conjunction with electrocardiogram changes) to diagnose underlying disease and choose an appropriate treatment. Blood tests can even be used to assess a person’s risk of a heart attack (eg, tests for c-reactive protein and homocysteine). Venous blood can be taken for microbiological tests (eg, blood cultures in cases of suspected sepsis) and immunological testing (eg, detecting rheumatoid factor when arthritis is suspected). Tests commonly requested from chemical pathology laboratories include those for renal, liver and kidney function as well as tests for cholesterol, triglycerides and glucose and drug assays.
Liver function tests
Liver function tests (LFTs) are a group of biochemical measurements that are used to identify patients who are suffering from liver or biliary tract disease. Substances measured include:
- Albumin
- Bilirubin
- Alanine aminotransferase (ALT)
- Aspartate amino transferase (AST)
- Gamma-glutamyl transferase (GGT)
- Alkaline phosphatase (ALP)
None of the above tests is specific for liver or biliary disease and other diseases can cause abnormal levels of one of more of these substances. Even in cases of liver disease, blood levels of one or more of these sub-stances might be within the reference range. However, it is unlikely that all the results would be within their respective reference ranges. Together, therefore, the combination of tests is more useful than a single test.
Liver enzymes (ALT, AST, etc) leak into the blood when liver cells are damaged so, strictly speaking, these tests indicate liver disease rather than liver function. ALT andAST levels provide an indication of the degree of inflammation as well as the possible causes or hepa to cellular damage. Similarly, ALP and GGT increases can suggest the presence of obstructive liver disease.
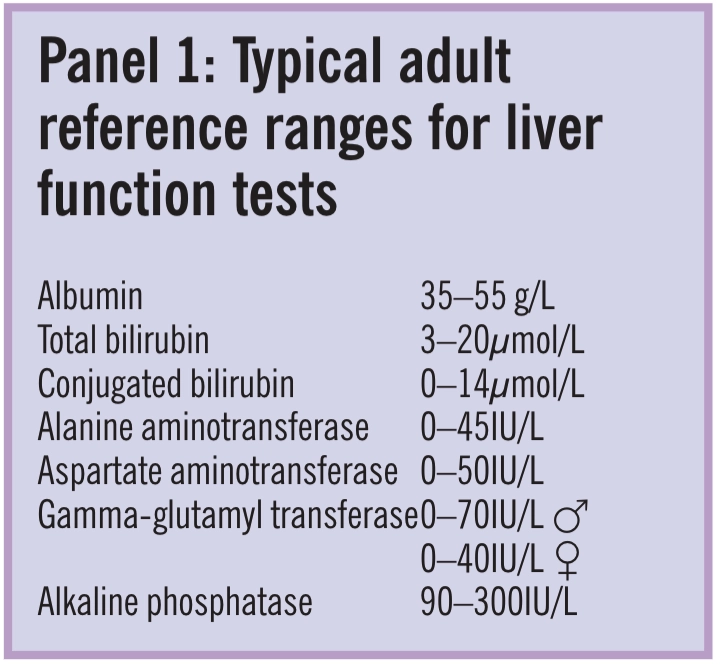
Panel 1 shows typical adult reference ranges for LFTs (ie, values in healthy people).Ranges vary between men and women, at different times of the day and will change with age.This needs to be recognised when tests are performed over time. So, if monitor-ing liver function rather than diagnosing disease, it is recommended that tests are consistently (ie, always in the morning or always in the afternoon).
Patients are usually advised to fast for four to eight hours before blood samples are taken for liver function testing because eating can affect test results. For example, having a meal can stimulate intestinal ALP release.
Patients might also be advised to stop taking drugs that could affect test results.However, many such drugs should not be stopped. For example, the enzyme inducer phenytoin can increase GGT and ALP levels, but stopping it could result in loss of epileptic control. The affect of phenytoin on test results are only usually a concern if enzyme levels exceed those normally considered asymptomatic. In such cases, an alternative test should be used, if possible. For example, some laboratories suggest that the protease leucine amino peptidase is measured instead of GGT. However, testing serum for leucine amino peptidase is generally not as sensitive or as convenient as testing for other liver enzymes and the levels of this enzyme can also be affected by some drugs (eg, oestrogens and progesterones). Unlike other liver enzymes, leucine amino peptidase can be measured in urine.
If you are asked for advice about LFTs, you should remember that as many as 5 percent of healthy, asymptomatic people can have liver enzyme levels outside their reference ranges. To diagnose liver disease reliably, information in addition to LFT results, such as from physical examination, patient history, biopsy or radiologic studies, is needed.
Albumin Albumin levels are low in chronic liver disease. Samples are centrifuged to separate blood cells from serum and the albumin in the serum is measured. Typically, dyes such as bromocresol green or purple are added to the serum. These attach to albumin molecules, changing the light absorbency of the dye in proportion to the amount of albumin present.Albumin is made from amino acids and accounts for around 60 per cent of plasma protein. Serum albumin level indicates how well the liver is making proteins (ie, a test of liver function). Although it might be expected that albumin levels will be low inpatients with liver disease, plasma concentrations change slowly because albumin has along half life. This means that while albumin levels are low in chronic liver disease (eg, cirrhosis), levels can remain within thereference range in cases of acute liver disease(eg, infective hepatitis).
Albumin levels can also be reduced in malnutrition, diseases associated with malabsorption (eg, Crohn’s disease), chronic renal failure, nephrotic syndrome and severe burns.Albumin levels decrease after surgery and are also affected by a patient’s state of hydration— dehydration raises albumin concentration and over hydration lowers it. Similarly, test results can be inaccurate in patients being given large amounts of intravenous fluids.Albumin levels also decrease in pregnancy and with age.Bilirubin Bilirubin is a breakdown product released when red blood cells are destroyed at the end of their 120-day lifespan. In the blood, unconjugated (or “indirect”) bilirubin is carried by albumin to the liver. Here, it is conjugated to make it more water-soluble, before it is excreted in bile. Conjugated bilirubin is also called “direct” bilirubin.
The concentration of bilirubin in serum, therefore, reflects the balance between the amount produced by erythrocyte destruction and that removed by the liver. To measure bilirubin concentration, several chemical reagents are added to the serum sample. Light absorbency (555nm) is measured so that bilirubin levels can be calculated.
Increases in bilirubin levels are particularly suggestive of disease of the bile ducts, but three main types of disease are associated with raised levels in adults:
- Diseases associated with damage to hepatocytes, such as acute or chronic hepatitis, cirrhosis, primary liver cancer, liver metas-tases (these lead to a reduced capacity to conjugate bilirubin for excretion)
- Diseases causing restriction of bile flow and, consequently, reduced bilirubin excretion (eg, cholestasis, gallstones obstructing the bile duct and carcinoma of the pancreas)
- Diseases causing increased red blood cell destruction and, therefore, increased bilirubin production (eg, haemolytic anaemias)
In healthy individuals, almost all serum bilirubin is in the unconjugated form. As lev-els rise above 35mmol/L, the patient becomes visibly jaundiced. In severe jaundice, bilirubin levels can rise to 500mmol/L or higher.Determination of the ratio of conjugated to unconjugated bilirubin can give some indication of the cause of the jaundice. If the proportion of conjugated bilirubin is high, this suggests biliary obstruction. If the proportions are about equal, hepatocellular damage is likely.Total and conjugated bilirubin are usually measured (see Panel 1). Total bilirubin is unconjugated plus conjugated bilirubin.Conjugated (direct) bilirubin can also be measured using urine samples collected over24 hours.
Examples of drugs that increase bilirubin measurements include allopurinol, some diuretics and theophylline. Penicillin can decrease bilirubin measurements.
Alanine aminotransferase The enzymeALT is present in high concentrations in the liver. It is also found in cardiac and skeletal muscle. However, ALT is considered as a specific marker of hepatocellular damage because levels are generally only significantly raised in liver disease. ALT is present in the heart and muscles in much lower concentrations — only marginal elevations occur in acute myocardial infarction.
People with acute liver damage have particularly high ALT levels and those with chronic liver disease and obstructive jaundice have more modestly raised levels.
Low ALT (and AST) levels suggest vitamin B6 deficiency.
Action: practice points
Reading is only one way to undertake CPD and theSociety will expect to see various approaches in a pharmacist’s CPD portfolio.
- Find out about other blood tests, such as those done to investigate menstrual or fertility problems.
- Find out what drugs might affect serum albumin levels and why.
- Pay a visit to your hospital’s haematology or chemical pathology department to gain a wider understanding of what blood tests involve.
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities.Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?
Aspartate aminotransferase AST is more widely distributed than ALT. It is present in the liver, heart, kidneys, skeletal muscle and red blood cells. AST levels are raised in shock. It is less specific for liver disease and is not included in liver function profiles by all laboratories. AST levels are also raised in pregnancy and after exercise.
Gamma-glutamyl transferase The enzyme gamma-glutamyl transferase (GGT)is present in high concentrations in the liver, kidneys, prostate and pancreas. Levels are raised in all types of liver and biliary tract dis-ease (acute and chronic) and also in carcinoma of the pancreas. GGT level can be used to identify those with liver or biliary diseasebut is not useful in establishing the cause.
Measuring GGT is most useful in patients at risk of liver disease due to alcoholism. This is because, unlike the other liver enzymes,GGT is raised by alcohol consumption even in the absence of liver damage. Levels return to normal when drinking is stopped, but if high levels of GGT persist, it is likely that some liver damage has been sustained or that the patient is still drinking. Measurement of GGT is, therefore, useful in managing patients with alcoholic liver disease.
As well as phenytoin, phenobarbital can increase GGT levels. Clofibrate and oral contraceptives can decrease GGT levels.
Alkaline phosphatase AP is produced in the liver, bile ducts, bone and gut and widely distributed in the body. Levels of this enzyme are raised in diseases of the liver and biliary tract, with the highest levels found in obstructive jaundice.
AP is usually raised in cirrhosis and liver cancers, but levels can be within the reference range or only slightly raised in acute hepatitis. In addition, increased levels are found in some diseases of the bone (eg, Paget’s disease, osteomalacia and bone tumours) and further tests will be requested.
Other tests for liver disease Other indicators of liver function include prothrombin time and platelet count (see PJ, 3 April p419–21). Proteins made by the liver are involved in blood clotting so in liver disease (especially in worsening chronic disease), prothrombin time is increased. Liver disease causes the spleen (which traps platelets) to become enlarged so that the platelet count is often reduced.
Thyroid function tests
The concentration of thyroid hormones in the blood can be measured (usually using immunoassay techniques with fluorescence or chemiluminescence as signals) and used to diagnosis and monitor thyroid disorders. The tests used vary between laboratories, but substances measured usually include:
- Total thyroxine (T4); free (biologically active) thyroxine plus protein-bound (bio-logically inactive) thyroxine in serum
- Total triiodothyronine (T3); free (biologically active) tri-iodothyronine and protein-bound tri-iodothyronine in serum
- Thyroid stimulating hormone (TSH)
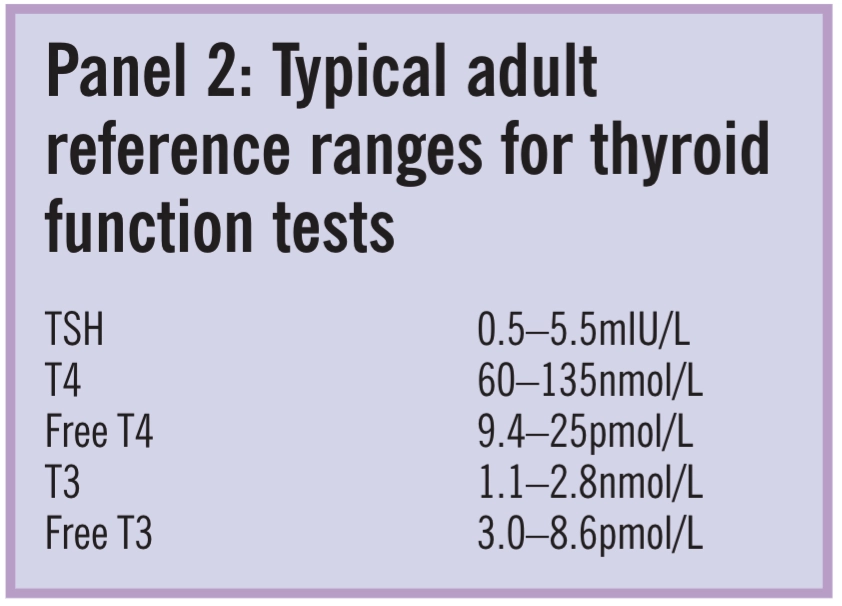
Sometimes, free thyroxine (FT4) and free tri-iodothyronine (FT3) are measured separately. Typical reference ranges are shown inPanel 2. Results outside the reference ranges are found in people with hyperthyroidismand hypothyroidism. In hyperthyroidism there is:
- Increased serum T4, FT4 and T3 concen-trations, although occasionally T4 and FT4are normal and only T3 is raised
- Reduced serum TSH concentration — in severe disease TSH can be undetectable
Results expected in hypothyroidism are:
- Reduced serum T4 and FT4 concentrations (although both may be at the lower end of their reference ranges in the early stages of the disease)
- Increased serum TSH
Some medicines (in addition to anti-thyroid drugs or thyroxine) can affect thyroid function1 and, therefore, the results of thyroid function tests. This must be borne in mind when interpreting test results. Drug interactions can occur at many sites along the thyroid hormone synthesis pathway. For example:
- Dopamine and glucocorticoids decreaseTSH secretion
- Lithium interferes with synthesis and decreases thyroid hormone secretion
- Amiodarone can cause hyperthyroidism because its high iodine content stimulates thyroid hormone production
In addition, some drugs can affect thyroid hormone secretion and transport. For example, oestrogens increase the concentration of serum carrier proteins and the serum concentration of T4 (androgens decrease serumT4 concentrations) and salicylates inhibit the binding of T3 and T4 to carrier proteins.
The metabolism of thyroid hormone as well as the absorption of exogenous thyroxine can also be affected. For example, rifampicin and phenobarbital increase the rate of T4 and T3 metabolism and colestipol binds T4.
However, it should be noted that although many drugs can affect thyroid function, not all will result in values as low or high as those expected in patients with hypo- or hyperthyroidism. In addition, healthy pituitary-thyroid function will compensate for low or high serum thyroid hormone levels.
Thyroid function is sometimes determined by measuring the rate at which the thyroid gland accumulates radioactive iodine.Renal function testsBoth blood and urine tests can be used to investigate kidney function. In terms of blood samples, the substances of interest are creatinine and blood urea nitrogen (BUN).Creatinine is a breakdown product of muscle. It is cleared by the kidneys, but only reabsorbed and secreted in small amounts.
This means that creatinine clearance can be used as a measure of glomerular filtration rate and, therefore, renal function.
The simplest way to find creatinine clearance is to measure the concentration of creatinine in serum and use this figure to find a population-based estimate by applying an appropriate formula. Obtaining a value for creatinine clearance from urine creatinine measurements is less convenient because this requires urine to be collected over 24 hours.
Creatinine levels vary according to a per-son’s size and muscle mass. Aminoglycosideshave been reported to increase creatinine measurements.
A BUN test is also routinely used to evaluate renal function. Urea is a breakdown product of protein.When protein is digested, amino acids are formed and ammonium ions are a by-product. These combine with small molecules to form urea, which enters the blood and is excreted in urine. Most renal diseases affect urea excretion so that BUN levels increase in the blood. Patients who are dehydrated can also have “abnormal” BUN levels and many drugs affect BUN, mainly by competing with it for renal elimination.Drugs that can increase BUN levels include allopurinol, some diuretics, aminoglycosides and indometacin. BUN levels are also affected by high protein diets.
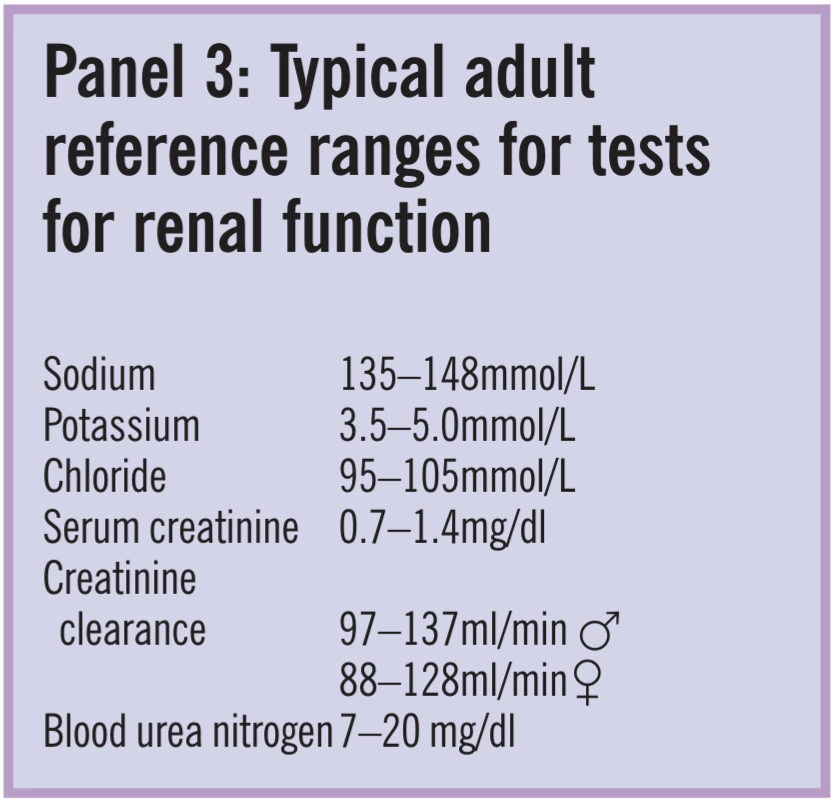
Electrolyte levels are also used to asses renal function. For example a high chloride ion concentration suggests renal failure. Adult reference ranges are shown in Panel 3. There is little difference between the expected levels of electrolytes in different laboratories.
References
- Surks MI, Sievert R, Drugs and thyroid function. New EnglandJournal of Medicine 1995;333:1688–94.


