Shutterstock.com
Learning outcomes
At the end of this case, you will be able to:
- Outline the pathophysiology, diagnosis and monitoring of chronic open-angle glaucoma;
- Describe the populations of patients who are at risk of developing glaucoma;
- Describe the optimum use of topical preparations and the rationale for topical therapy in the case of ocular conditions;
- Outline the chemistry and mechanism of action of latanoprost;
- Outline methods for reducing or preventing side effects from ocular products.
Miss NG is 34 years old and African–Caribbean. She regularly comes to your community pharmacy to collect medication for her father, Mr HG, who is 56 years old. During today’s visit, she seems anxious and asks to speak to the pharmacist. She is concerned that her father has developed glaucoma and may go blind. The glaucoma was suspected by her father’s optometrist who performed air puff tonometry as part of routine screening when he went to buy a new pair of glasses. He was then followed up and given latanoprost eyedrops, which she is collecting today.
- What is chronic open-angle glaucoma?
- How is it diagnosed?
- Which people are most likely to develop glaucoma?
- Is the patient likely to go blind?
- What class of drug is latanoprost and what is its mechanism of action?
- How is it related structurally to the naturally occurring biomolecule that it mimics?
Miss NG comes back the next day because her father is having difficulty in using the eyedrops as his eyes seem to run with tears when he administers the drops. She asks if her father could have a tablet instead.
- What are the common formulations used for eyedrops?
- How should eyedrops be correctly administered to the eye?
- Why are topical medications used rather than oral therapy for ocular conditions?
At the end of the week, Miss NG has persuaded her father to come into the pharmacy because she is concerned that he is having a reaction to the latanoprost eyedrops as his eyes look pink.
- What is the side effect that Mr HG is experiencing?
- What can patients do to minimise side effects from ocular products?
Case discussion
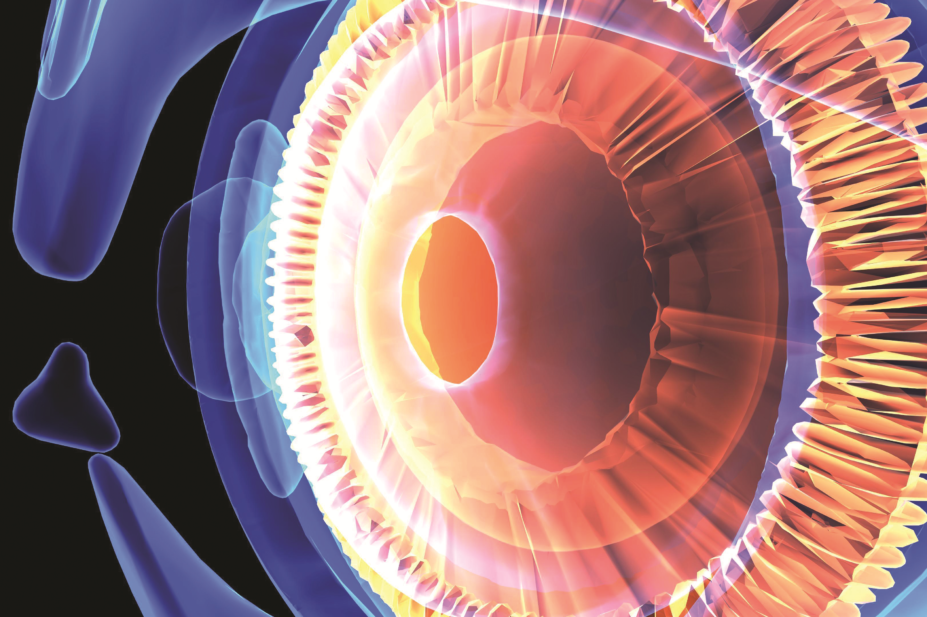
Chronic open-angle glaucoma and its pathophysiology
Glaucoma occurs when the drainage tubules (trabecular meshwork) in the eye are unable to drain the eye effectively of liquid aqueous humour, produced by the ciliary processes. As a result, intraocular pressure builds up, which, if left untreated, can permanently damage the optic nerve and nerve fibres in the retina, leading to visual field loss and eventual blindness. Intraocular pressure is the level of aqueous fluid pressure inside the eye. Normal intraocular pressure usually ranges from 12mmHg to 21mmHg and can be measured by means of a tonometer, nowadays using a non-contact air-puff method to detect small deflections of the cornea. Glaucoma is normally associated with a raised intraocular pressure >21mmHg; however, some individuals with ‘ocular hypertension’ have an abnormally raised intraocular pressure without developing optic nerve damage.
Glaucoma encompasses a group of ocular conditions, typically, but not always, characterised by increased intraocular pressure, optic disc ‘cupping’ (owing to the thinning of the optic nerve head and enlargement of the optic cup observable at the back of the retina) and visual (peripheral) field loss. Chronic open-angle glaucoma is the most common type and develops slowly. In open-angle glaucoma, the drainage angle (Schlemm’s canal) is open so that there is no structural obstruction to the drainage network. There is no visible abnormality of the trabecular meshwork. It is thought that something is wrong with the ability of the cells in the trabecular meshwork to carry out their normal function, or there may be fewer cells present, as a natural result of getting older. Some think that this is because of a structural defect of the eye’s drainage system, others that it is caused by an enzymatic problem (e.g. microsomal CYP1B1 mutations or deletions in the galactosylceramidase gene [GALC]).
Primary angle-closure glaucoma is comparatively rare. Although onset may be insidious or rapid, a sudden painful increase in intraocular pressure occurs as a consequence of blockage to the drainage canals. Immediate medical attention is required.
Glaucoma is one of the leading causes of preventable blindness in the UK, accounting for around 15% of registered cases of blindness.
People most at risk of developing glaucoma
There are several risk factors for the development of glaucoma. Age is a major factor, because the condition becomes much more common as people get older: in the white population, aged <40 years the prevalence is 1 in 50; in those >75 years, prevalence is 1 in 10. Glaucoma is also more likely in people of African or African–Caribbean origin and if there is a family history: people with relatives with the condition may have a four- to nine-fold increased risk of its development. These risk factors may be relevant when targeting screening programmes to those most at risk.
Visual field loss
Vision loss begins with peripheral or side vision. Patients compensate for this unconsciously by turning their head to the side, and may not be aware of a problem until significant vision is lost. If undiagnosed or untreated, the damage will progress and ultimately the whole visual field will be lost. Treatment can halt or slow down the progress of visual field loss, but it cannot regain any of the visual field that has already been lost. Thus, screening (especially in individuals most at risk) to identify disease early on is routinely undertaken by community optometrists.
Rationale for topical treatment of ocular conditions
Glaucoma is most often treated using eyedrops. Systemically (often orally) administered ocular drugs are prevented from reaching therapeutic concentrations within the eye by a variety of physiological mechanisms as well as the characteristics of the drug itself. The blood–aqueous barrier (ciliary epithelium and capillary of the iris) and the blood–retinal barrier (non-fenestrated capillaries of the retinal circulation and tight junctions of retinal epithelium) are responsible for the regulation of drug/molecule transport from the systemic circulation to the anterior and posterior ocular tissues, respectively. In some cases, the vitreal drug level can be <10% of the serum concentration. Although increasing the systemic level would create a corresponding rise in vitreal concentration, this would be at the cost of increasing systemic side effects, and any issues that would normally be associated with the drug metabolism and excretion. It is therefore more clinically effective, cost-effective and safer to use a topical product.
Treatment options
Classes of drug most commonly used are: prostaglandin analogues (e.g. latanoprost) which increase the flow of aqueous humour out of the eye or β-adrenoreceptor blockers (e.g. timolol), thought to reduce intraocular pressure by slowing down production of aqueous humour. Other drugs that may be used are carbonic anhydrase inhibitors (e.g. dorzolamide or brinzolamide), sympathomimetics (α2-adrenoreceptor agonists, e.g. brimonidine or apraclonidine) or miotics (parasympathomimetics, e.g. pilocarpine or anticholinesterases: physostigmine or echothiophate – although these are now less frequently prescribed in practice).
Chemical properties of latanoprost
Latanoprost is a structural analogue of the naturally occurring prostaglandin F2α. As expected, the two molecules are very similar to each other. Latanoprost contains an isopropyl ester in place of the free carboxyl group in prostaglandin F2α. This ester must be hydrolysed by plasma esterases to generate the free carboxyl-containing metabolite, which is biologically active (latanoprost is a prodrug). In addition, on the other side chain, latanoprost lacks the additional alkene group and has an aromatic ring at the end of the alkyl chain. There are five chiral centres and an alkene capable of geometric isomerism in latanoprost. Of the 64 possible stereoisomers of this molecule, only latanoprost has the correct shape for effective interaction (after ester hydrolysis) with its prostanoid F2α receptor target. The alkene in latanoprost has a cis (or Z) configuration.
Formulations for the treatment of eye conditions
Eyedrop preparations may be solutions, suspensions or emulsions. Solution preparations are most common: latanoprost and timolol eyedrops are solution formulations. Solutions are homogeneous, allowing high dose uniformity and rapid onset of action. Poorly water-soluble drugs, such as corticosteroids, may be formulated as suspension eyedrops, e.g. prednisolone eyedrops. Homogeneity and dose uniformity, as with other suspension formulations, may be problematic and require the inclusion of suspending and thickening agents, such that the particles are readily dispersible on shaking, before administration.
Much less frequently, drugs may be formulated in an oil-in-water submicrometre emulsion. An example of such a product is Restasis, an eyedrop formulation of ciclosporin dissolved in an oil phase, stabilised as an emulsion with the non-ionic surfactant Polysorbate 80. In some cases, such as surgery, trauma and infection, it will be necessary to treat the structures surrounding the eye as well as the eye itself. Oral antibiotics, antivirals and anti-inflammatory agents are therefore given alongside topical treatment. During inflammatory states, the blood–ocular barriers are broken down, allowing for greater penetration. These barriers are usually restored once the inflammation has resolved. To increase ocular penetration of systemic therapy, the drugs chosen should have: a small molecular size, high lipid solubility and low protein-binding affinity.
Administration of eyedrops
Regular application of eyedrops is vital to prevent disease progression, even if the patient is not experiencing any symptoms. The need for, and how to use, eyedrops should be carefully explained to the patient.
The use of topical ocular products, as for many other medicines, is associated with problems of adherence. A common problem is that patients may not know exactly where the product should be administered. Patients should avoid administering drops on, or close to, the cornea, which, as the most sensitive tissue in the body, is densely populated with nerves. Therefore, any contact with the cornea will produce an involuntary reflex to rapidly close the eyelid to protect it (blinking). Blinking may cause the bulk of the eyedrop to be removed from the ocular surface. An explanation of how to administer the drops should therefore be provided:
- Use your finger to gently pull down your lower eyelid
- Hold the bottle over your eye and allow a single drop to fall into the pocket you have created in your lower lid, so that the drop touches the sclera and not the cornea
- The pocket can then be gently released, allowing the drop to disperse across the ocular surface, closing your eye and keeping it closed for several minutes
If patients are using two different eyedrops, they should allow at least 5–10 minutes between using the different drops.
Sometimes, dexterity issues are a problem. If so, compliance aids can be helpful, as can different types of packaging, e.g. bottles that are easier to squeeze.
Latanoprost eyedrops are no longer required to be kept in a refrigerator before and after opening, but must not be stored >25°C. In general, eyedrops for domiciliary (home) use should not be used more than 4 weeks after opening the bottle.
Side effects from ocular products for glaucoma
The ingredients in ocular products can produce side effects just like other dosage forms. These may be limited to the local area of administration or systemic effects after passage of the drug into the systemic circulation. Table 1 gives some examples of side effects that may occur locally and systemically after ocular use of glaucoma treatments.
The local effects of topical ocular products are hard to avoid, but for most patients are not troublesome, and in the case of conjunctival hyperaemia can be short-lived. The systemic effects can, however, be minimised by employing the technique known as punctual occlusion. The purpose of this technique is to place a finger close to the corner of the eye for a short period after administration of the product. This will prevent the product escaping through the punctum, which leads to the canaliculus, on to the lacrimal sac, which in turn leads to the nasolacrimal duct and the nasopharyngeal cavity. Drugs that enter this system are more likely to be absorbed, so blocking this route is important for those patients who are likely to find the systemic effects problematic.
Topical side effects
| Table 1: Examples of local and systemic side effects from ocular products | ||
|---|---|---|
Product | Topical side effects | Systemic side effects |
β-adreno-receptor blockers | Redness of the eye, burning, loss of corneal sensation, reduced ocular blood flow | Exacerbation of asthma and COPD, hypotension, bradycardia, nightmares |
Prostaglandin analogues | Conjunctival hyperaemia, darkening and lengthening of eyelashes, increased pigmentation of iris and periocular skin, macular oedema, uveitis | Reactivation of herpes, bitter taste |
Parasympathomimetics (miotics) | Visual blurring (children), darkening of visual field (pupillary constriction), stinging | Headache (initially due to ciliary spasm), sweating |
α2-adreno-receptor agonists | Redness of the eye, eyelid retraction, tearing, discomfort | Fatigue, drowsiness, hypotension, dry mouth, headache, drowsiness |
Carbonic anhydrase inhibitors | Stinging | Headache, unpleasant taste |
Extended learning
Outline the stepwise treatment of open-angle glaucoma.
- What is closed-angle glaucoma?
- What are its symptoms and why is it a medical emergency?
- What are the treatment options for closed-angle glaucoma?
- What surgical options are available for glaucoma?
- What is steroid-induced glaucoma?
- How are eyedrops formulated, manufactured, packaged and sterilised?
- Who are optometrists?
- What is their role in eyehealth?
- How are their services accessed?
- What compliance aids are available for the administration of eyedrops?
- This article was adapted from
Integrated Pharmacy Case Studies
, published by Pharmaceutical Press.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
You might also be interested in…

Wet age-related macular degeneration: case study

Topical drug dosage forms for eye conditions
