In 2004, the National Institute for Health and Clinical Excellence (NICE) published practice guidance relating to the treatment and management of eating disorders.1 It emphasises that care should involve integrating appropriate psychological, nutritional and medical (including pharmacological) approaches. The goals of treatment should be to restore healthy weight and eating behaviour, to reduce psychosocial factors that maintain these disorders and to support recovery of social and occupational roles. The evidence base is limited, particularly for anorexia nervosa (AN), and much of the NICE guidance is based on expert clinical experience rather than robust randomised controlled trials.
Because eating disorders are syndromes with a spectrum of severity, it is suggested that treatment can be delivered using a stepped-care model. Guided self help in primary care may be effective for those with a mild disorder,2 whereas specialist outpatient treatment is more appropriate for those with more severe disorders. Inpatient and day-patient care are reserved for those with the most severe disorders.
There is substantial stigma associated with eating disorders among both the general public and healthcare professionals. Some common misconceptions include: that people with eating disorders are unpredictable, hard to talk to, have only themselves to blame and should “pull themselves together”.1 These beliefs adversely affect the treatment experience for individuals and their carers. This stigma, combined with ambivalence to change (which is characteristic of patients with eating disorders) represents a considerable barrier to engaging in, and developing, a helpful therapeutic relationship.
Since there is a lack of evidence to guide the management of atypical eating disorders, it is recommended that the guidance for either AN or bulimia nervosa (BN) is adopted, depending on what an individual’s eating disorder most resembles.1 This article summarises psychological, nutritional, medical and pharmacological components of the management of eating disorders.
Medical management and monitoring
The severity of symptoms and results of baseline investigations will determine how a patient with an eating disorder is managed. Monitoring can include: monitoring blood pressure, pulse, temperature and weight; electrocardiography; and blood tests, eg, to measure electrolytes, glucose and liver function.
Electrolyte disturbances
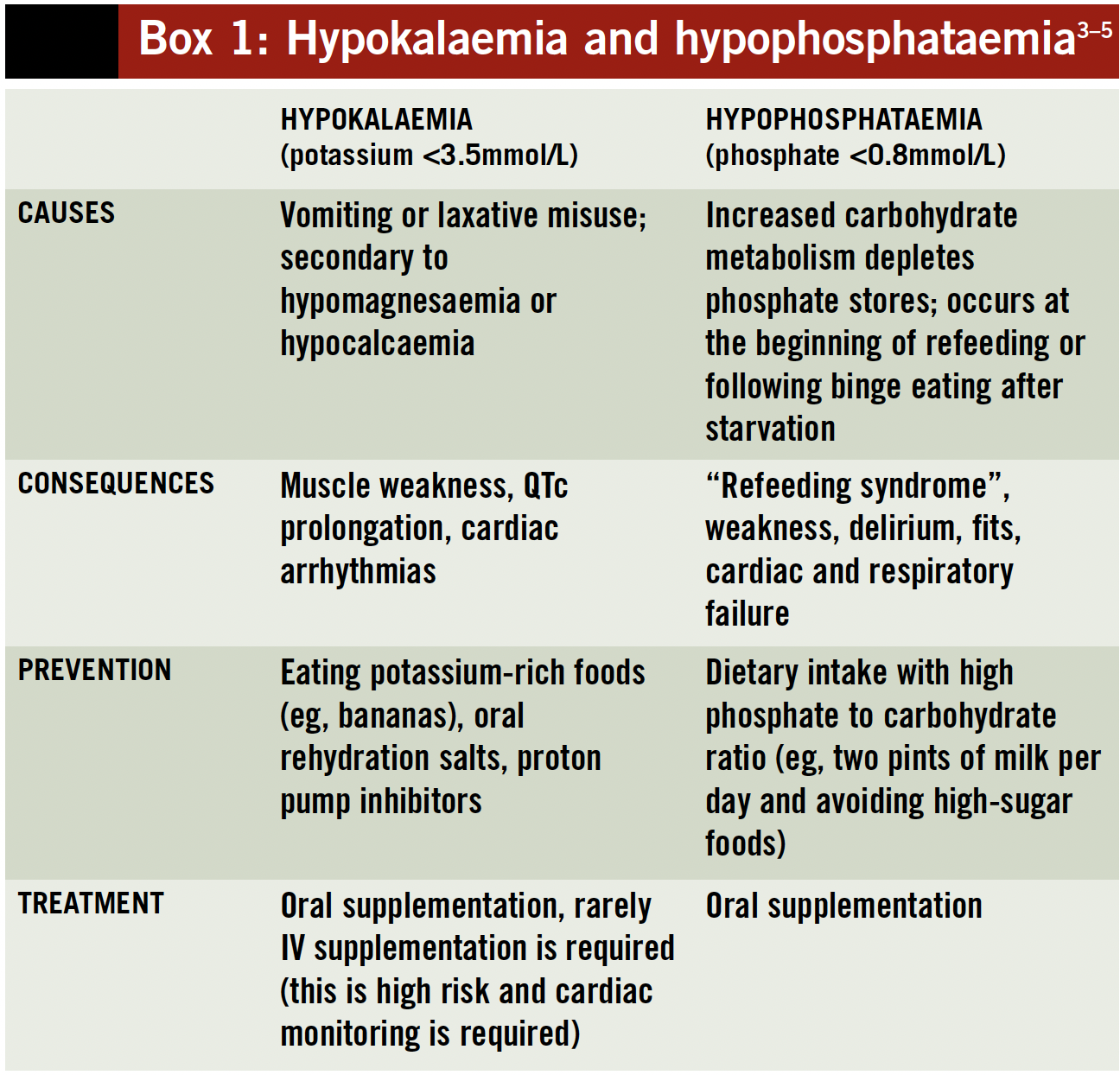
Blood test results can be affected by severe starvation or purging, or when starting to restore weight. Hypophosphataemia and hypokalaemia are common — the causes and treatments are outlined in Box 1 (p331). Correction of biochemical abnormalities should be done cautiously because changes are often chronic and therefore some physiological adaptation may have occurred.
Micronutrient deficiencies
Several deficiencies in micronutrients have been identified in patients with eating disorders, particularly those with AN, but the clinical significance of many of these mineral and vitamin deficiencies is unclear.
Thiamine (vitamin B1) deficiency can be exacerbated when reintroducing food (refeeding). Therefore, prophylactic supplementation with at least 25mg daily (higher doses [eg, 100mg twice daily] are often used in practice) is recommended when weight gain begins. Thiamine supplementation prevents precipitation of Wernicke-Korsakoff syndrome, a severe and irreversible neurological condition.
Zinc deficiency can result in altered taste and a range of neuropsychiatric symptoms, including cognitive impairment. Despite this, routine use of zinc supplementation is not recommended.
AN is associated with osteoporosis; however, the underlying causes differ from those of postmenopausal osteoporosis and there have been few robust studies regarding treatment. Specialist advice is recommended when considering the available treatment options.6
Other deficiencies that can occur and may require specific supplementation include folic acid, vitamin B12, iron and vitamin C. A combination oral multivitamin and multimineral preparation, such as Forceval or Sanatogen Gold, is recommended routinely.1,3
Fluid balance
Peripheral oedema can occur when refeeding, particularly in those who have a history of laxative misuse or vomiting. Initially, fluid retention may result in several kilograms of weight gain and cause considerable distress. It is important that cardiac failure secondary to overly rapid feeding is excluded as a possible cause.
Oedema should be managed conservatively with reassurance, avoidance of excessive fluid intake and advice to elevate the feet during the day and the head at night.
Diuretics are likely to exacerbate the underlying cause of oedema and should be avoided. Oedema usually resolves within two weeks, but can take considerably longer.
Pharmacological treatments
Anorexia nervosa
Few robust trials have evaluated pharmacological treatments for AN and, despite a lifetime prevalence comparable to that of schizophrenia, the condition has received little attention from the pharmaceutical industry.
A Cochrane review of antidepressants for the treatment of AN found no evidence for improving symptoms (including weight gain) from four placebo-controlled trials.7
There is insufficient evidence to support the routine use of typical antipsychotics or antihistamines to promote weight gain, according to current NICE guidance.1 However, evidence for the use of olanzapine (2.5–15mg daily) has been emerging in the literature: recently several small, short-term, randomised controlled trials have demonstrated benefits in terms of improving weight gain, treatment adherence and other psychological symptoms such as agitation, pre-meal anxiety and obsessional or abnormal beliefs.8
High levels of anxiety (especially before meals) are common and, where possible, psychological approaches should be used to manage anxiety: in practice, treatment may include the short-term use of antipsychotics (eg, olanzapine) or antihistamines (eg, promethazine).
Pharmacological treatment alone is insufficient to manage AN effectively and is not recommended.1
Bulimia nervosa
High-dose selective serotonin reuptake inhibitor (SSRI) antidepressants (eg, fluoxetine 60mg daily) have been shown to be superior to placebo for the treatment of BN and can reduce the frequency of binge eating and purging by as much as a third. However, the long-term efficacy of SSRIs is unknown and they are less effective and acceptable (with greater patient drop-out rates in trials) than cognitive behavioural therapy (CBT).9
Therefore, the most appropriate indication for SSRIs is as a short-term alternative, or adjunct, to an evidence-based self-help programme (while waiting for psychological treatment to become available), or for those also requiring treatment for depression. Current evidence does not support combined pharmacotherapy and CBT.10 No other pharmacological treatments are recommended for BN.
Psychological therapies
Addressing an individual’s ambivalence to treatment and developing and maintaining their engagement in the process of change is essential for the treatment of eating disorders. Motivational interviewing is a useful technique in this respect (EDITOR—see Clinical Pharmacist 2010;2:28). Key tenets include:11
Adopting a collaborative rather than authoritarian approach
Respecting an individual’s autonomy
Facilitating and strengthening an individual’s own motivation to change
Providing information to individuals, and their families where appropriate, is an important component of the early stages of treatment. “Psycho-education” — educating people with eating disorders to deal with unhelpful beliefs, (eg, that taking laxatives can bring about weight loss) — can be facilitated by self-help books and other resources. Some of these are provided by the charity Beating Eating Disorders (Beat).
Anorexia nervosa
Family therapy for the treatment of adolescents with AN has moderate supporting evidence and is the first-line treatment recommended by NICE. At five-year follow-up, a recovery rate of 75% has been reported with relapse rates of only 8% after weight restoration.12
For adults, treatment outcomes are poorer and this emphasises the need for early intervention. Specialist therapies have been shown to be more effective than nonspecialist treatment or dietary advice alone (with approximately a third achieving remission)13,14. Specialist therapies include:
- Focal psychodynamic psychotherapy
- Family therapy
- Cognitive analytic therapy
- Specialist supportive clinical management
- CBT
There is currently, however, no robust evidence to support the use of any of these therapies, including CBT.
Bulimia nervosa
CBT for BN has been widely studied and is more effective than other psychological therapies2 — it is therefore considered to be the most appropriate first-line treatment. CBT can be adapted for children and adolescents (involving the patient’s family where appropriate) although there has been little systematic evaluation of this approach. Interpersonal psychotherapy is as effective as CBT at one year’s follow-up, but the effect is slower.15
Nutritional management
Nutritional management should be a core component of treatment for eating disorders. The aim is to establish a structured eating pattern that includes three meals and three snacks per day. This approach reduces hunger and thus helps allay anxiety about loss of control of eating and reduces the risk of binge eating.
Reintroduction of food should start slowly with a low fibre, energy-dense, phosphate-rich diet including milk, eggs and chicken. This reduces the risk of gastric dilation (which can result in perforation and death) and refeeding syndrome (which can occur a few days after the introduction of food and is characterised by metabolic disturbances such as hypophosphataemia, hypokalaemia and hypoglycaemia). Consequences of refeeding syndrome include confusion, convulsions, heart failure and death.
Standardised meal plans are often used in specialist inpatient and day-patient settings and are designed to increase food intake and weight safely. Close physical health monitoring is required, especially in the first two weeks of refeeding.
A broader range of foods is gradually introduced and the quantity is slowly increased to reach a target weight gain of 0.5kg per week for outpatients and 0.5–1kg for inpatients.1 Agreeing on a healthy target weight at the start of treatment is helpful and the patient’s premorbid, healthy adult weight is a useful guide. For those patients who have never achieved this, a BMI of 20 is an appropriate initial goal for those who are underweight. Weight stabilisation is a suitable goal for those in the normal or overweight range.
Food diaries
Food diaries can be a useful strategy to help outpatients (and inpatients during periods of leave) monitor their food intake and behaviours such as binge eating, purging and excessive exercise.
Additionally, recording day-to-day difficulties and emotional experiences in the diary helps individuals to begin to recognise the patterns of thinking, feeling and behaviour that maintain the eating disorder, for example, “…exam today, felt fat and stupid…ate four chocolate muffins, felt guilty. Vomited.” The aim of therapy is then to help individuals develop healthier strategies that they can use to cope with difficult thoughts, feelings and relationships.
Supportive treatments
Constipation can be a problem for people with an eating disorder, especially in those with low weight or a history of laxative misuse. Dietary advice, such as increasing fibre and fluid intake, is usually sufficient. However, the addition of a bulk-forming laxative or stool softener may be required. Stimulant laxatives are not recommended, since long-term use can lead to reduced colon motility and exacerbate constipation. In addition, they are liable to misuse by the patient.
Feelings of bloating, fullness or early satiety can occur because of delayed gastric emptying. Bowel motility can be encouraged by giving metoclopramide (a prokinetic) 5–10mg three times daily before meals. However, the efficacy of metoclopramide is limited and it can cause extrapyramidal side effects.
For some, antispasmodics such as mebeverine can alleviate colicky abdominal pain, although this is often unsuccessful and the issue might be managed best through reassurance and smaller, more frequent food portions.
Enteral feeding
In a small number of cases of severe AN enteral feeding will be necessary. This occurs when individuals are medically unstable and unable to feed themselves despite expert nursing care. The decision to use compulsory enteral feeding should only be taken following specialist advice and should be within the legal framework of the Mental Health Act (1983) or Children Act (2004).
There are a variety of enteral feeding regimens (eg, 20 hours’ continuous administration with a four-hour rest period) and different feeds available. Many specialist services use bolus enteral feeds to support oral feeding by replacing missed meals.
The nasogastric route is preferred but the nasojejunal route is sometimes used if persistent vomiting prevents weight gain. Close monitoring for electrolyte disturbances and hyperglycaemia is required. Before starting an enteral feed, phosphate supplements and intravenous vitamin B and C (Pabrinex) is recommended to prevent refeeding syndrome and Wernicke-Korsakoff syndrome and should be continued for at least three days.3
Enteral feeding should be used as a short-term measure since it does not actively involve the individual in the recovery process. Patients should be encouraged to eat while receiving enteral feeds, if they are able to tolerate it. NICE recommends that total parenteral nutrition is not used for the treatment of AN unless there is substantial gastrointestinal impairment.1
Role of pharmacy staff
Signposting
Pharmacy staff must be aware of over-thecounter products that are liable to misuse by those with eating disorders, such as laxatives and orlistat. If there are reasonable grounds for suspecting misuse, then sale must be refused.16 A person being underweight should not be the sole trigger for suspecting misuse since most individuals with BN are of normal weight or are overweight. Consideration should be given to the frequency, quantity and reasons for purchase in addition to being vigilant for the signs and symptoms of eating disorders.
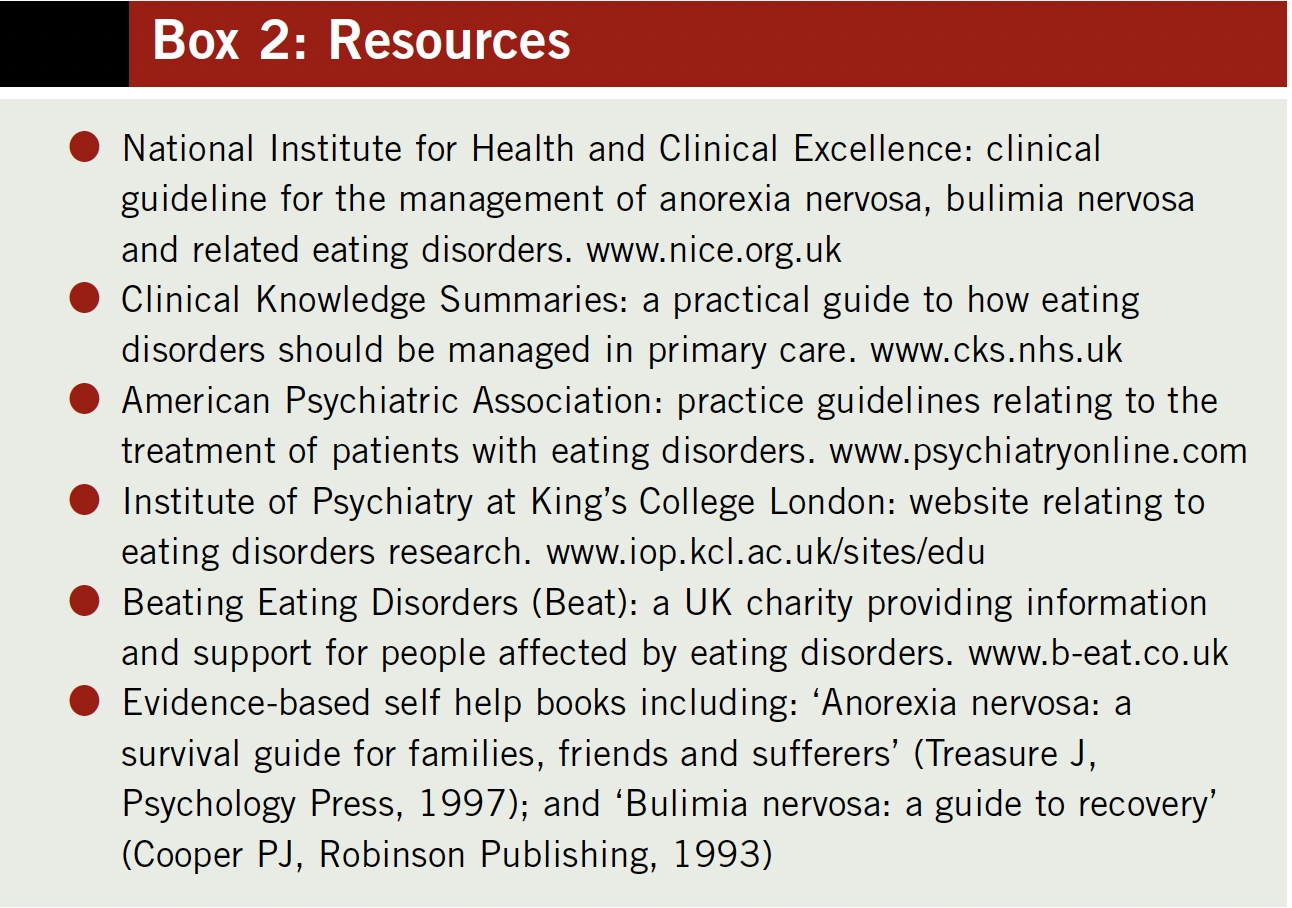
However, restricting sales of these products is unlikely to prevent eating disorders in the long term. Therefore, inappropriate requests should be seen as an opportunity for early intervention.17 Pharmacy staff should be able to help those with a suspected eating disorder by providing basic information about the risks associated with laxative misuse. Individuals should be encouraged to discuss these issues with their GP and also be directed to local support services for further information (see Box 2).
Pharmaceutical care
Pharmacists should be aware of the potential for altered pharmacokinetics in people with eating disorders (due to starvation, vomiting, dehydration or over-hydration). Changes can include reduced absorption or an increased sensitivity to intended or unwanted effects of medicines. It is therefore advisable to use lower doses of medicines initially (such as those used in the elderly), then assess response and alter doses accordingly.
Caution should be exercised with medicines that increase the QTc interval (such as macrolide antibiotics and antipsychotics) and those that exacerbate electrolyte disturbances, especially hypokalaemia. It is recommended that individuals with AN should have an alert placed on their prescribing record to highlight these risks.1
Pharmacists can also have a role in ensuring appropriate monitoring of electrolytes, especially during the initial stages of refeeding and when supplementation is being used. Pharmacist input may also be required when considering pharmacological treatments for comorbidities.
Summary
The National Institute for Health and Clinical Excellence recommends that the management of eating disorders should be based on integrated psychological, nutritional and medical care (including medicines in some instances).
Psychological therapies are considered to be the most effective treatment for anorexia nervosa, along with establishing a healthy diet and weight restoration. Achieving this safely requires prior correction of any biochemical abnormalities and close monitoring, especially for those with an especially low body mass index. Pharmacological treatments are not recommended as a sole intervention for the treatment of anorexia nervosa.
Cognitive behavioural therapy is the first-line treatment for bulimia nervosa. Antidepressants such as selective serotonin reuptake inhibitors can also be used.
Jonathan Cavan is advanced specialist pharmacist at St Charles Hospital and Frances Connan is consultant psychiatrist for eating disorders at Vincent Square Clinic, both part of Central and North West London NHS Foundation Trust. E: jonathancavan@nhs.net
References
1 National Collaborating Centre for Mental Health. Eating disorders: core interventions in the treatment and management of anorexia nervosa, bulimia nervosa and related eating disorders 2004. www.nice.org.uk/CG9 (accessed 1 May 2010).
2 Hay PP, Balaltchuk J, Stefano S, et al. Psychological treatments for bulimia nervosa and binging. Cochrane Database of Systematic Review 2009; issue 4.
3 Royal College of Psychiatrists. Guidelines for the nutritional management of anorexia nervosa 2005. www.rcpsych.ac.uk/files/pdfversion/cr130.pdf (accessed 14 May 2010).
4 Treasure, J. A guide to the medical risk assessment for eating disorders 2009. www.iop.kcl.ac.uk/sites/edu (accessed 14 May 2010).
5 Eiro M, Katoh T, Watanabe T. Use of a proton-pump inhibitor for metabolic disturbances associated with anorexia nervosa. New England Journal of Medicine 2002;324:140.
6 Mehler PS, MacKenzie TD. Treatment of osteopenia and osteoporosis in anorexia nervosa: a systematic review of the literature. International Journal of Eating Disorders 2009;42:195–201.
7 Claudino AM, Silva de Lima M, Hay PPJ, et al. Antidepressants for anorexia nervosa. Cochrane Database of Systematic Reviews 2006; issue 1.
8 Dunican KC, DelDotto D. The role of olanzapine in the treatment of anorexia nervosa. Annals of Pharmacotherapy 2007;41:111–5.
9 Capasso A, Petrella C, Milano W. Pharmacological profile of SSRIs and SNRIs in the treatment of eating disorders. Current Clinical Pharmacology 2009;4:78–83.
10 Goldbloom DS, Olmsted M, Davis R, et al. A randomized controlled trial of fluoxetine and cognitive behavioural therapy for bulimia nervosa: shortterm outcome. Behaviour Research and Therapy 1997;35:803–11.
11 Miller WR, Rose GS. Toward a theory of motivational interviewing. American Psychologist 2009;64:527–37.
12 Eisler I, Simic M, Russell GF, et al. A randomised controlled treatment trial of two forms of family therapy in adolescent anorexia nervosa: a fiveyear follow-up. Journal of Child Psychology and Psychiatry 2007;48:552–60.
13 Dare C, Eisler I, Russell G, et al. Psychological therapies for adults with anorexia nervosa: randomised controlled trial of out-patient treatments. British Journal of Psychiatry 2001;178:216–21.
14 McIntosh VV, Jordan J, Carter FA, et al. Three psychotherapies for anorexia nervosa: a randomized, controlled trial. American Journal of Psychiatry 2005;162:741–7.
15 Agras WS, Walsh T, Fairburn CG, et al. A multicenter comparison of cognitive-behavioural therapy and interpersonal psychotherapy for bulimia nervosa. Archives of General Psychiatry 2000;57:459–66.
16 Royal Pharmaceutical Society. Professional standards and guidance for the sale and supply of medicines 2009. www.rpsgb.org/pdfs/coepsgssmeds.pdf (accessed 6 June 2010).
17 Bryant-Waugh R, Turner H, East P. Over-the-counter laxatives and eating disorders — a survey of pharmacists’ and other retailers’ views and practice. Pharmaceutical Journal 2005;275:87–91.
