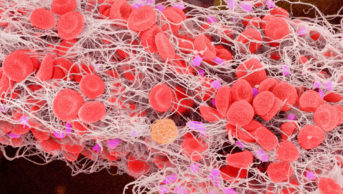
Dr P Marazzi / Science Photo Library
Warfarin has been widely used as an anticoagulant for over 70 years, since its discovery and initial use as a rodenticide in the early 20th century. It has been estimated that 1.25 million people take warfarin in the UK — 1.9% of the population[1]
.
Warfarin is a vitamin K antagonist and exerts its anticoagulant effect by interfering with the production of vitamin K-dependent coagulation factors (factors II, VII, IX and X)[2]
. Two other vitamin K antagonists (acenocoumarol and phenindione) are licensed for use as oral anticoagulants in the UK; however, warfarin is the most commonly prescribed[3]
,[4]
.
Warfarin is indicated for, among other things:
- Treatment of acute venous thromboembolism (VTE), (e.g. deep vein thrombosis [DVT] or pulmonary embolism [PE]);
- Atrial fibrillation (AF) to prevent stroke where there is a risk of embolisation;
- Mechanical prosthetic heart valves (to prevent thrombi forming on the valves).
Treatment with warfarin necessitates regular monitoring of the international normalised ratio (INR), with the aim of ensuring it remains within the designated target range, and as close to the actual target INR as possible. A target INR is determined by the indication for anticoagulation and associated bleeding risk for the patient. When setting target INRs, pharmacists and healthcare professionals will usually use a local protocol, which is most often based on current guidelines from the British Committee for Standards in Haematology (BCSH)[5]
. Example target INRs are provided in Table 1. While BCSH guidelines provide a target INR, a range of +/-0.5 above and below the target is generally used in practice.
| Table 1: Examples of typical target international normalised ratio (INR) values. | |
|---|---|
| Data taken from British Committee for Standards in Haematology (BCSH) Guidelines for oral anticoagulation with warfarin – fourth edition[5] | |
| Indication | Target INR |
| Initial treatment of first episode venous thromboembolism (VTE) | 2.5 (range 2–3) |
| Antiphospholipid syndrome | 2.5 (range 2–3) |
| Atrial fibrillation | 2.5 (range 2–3) |
| Mechanical heart valve | Dependent upon prosthesis thrombogenicity and patient-related risk factors (see Table 2) |
| Table 2: Target international normalised ratio (INR) for mechanical prostheses | ||
|---|---|---|
Prosthesis Thrombogenicity* | INR target No patient risk factors | INR target Patient-related risk factors†|
| Low | 2.5 | 3.0 |
| Medium | 3.0 | 3.5 |
| High | 3.5 | 3.5‡ |
| *Prosthesis thrombogenicity: Low: Carbomedics (aortic position), Medtronic Hall, St Jude Medical (without silzone); Medium: Bjork-Shiley, other bileaflet valves; High: Starr-Edwards, Omniscience, Lillehei-Kaster | ||
| †Patient-related risk factors for thrombosis: Mitral, tricuspid or pulmonary position; Previous arterial thromboembolism; Atrial fibrillation; Left atrium diameter >50 mm; Mitral stenosis of any degree; Left ventricular ejection fraction <35%; Left atrial dense spontaneous echo contrast | ||
| ‡Was 4·0[22] | ||
| Source: Adapted with permission from[22] | ||
INR is a standardised measure of the patient’s prothrombin time. It is obtained by comparing the measured prothrombin time to a reference value, which allows results measured in different laboratories to be compared reliably.
The potential consequences of a subtherapeutic INR depend on: the initial indication for anticoagulation; how far below the target the INR has fallen; how long the INR has been subtherapeutic; and, in the case of VTE, the time since the VTE occurred. For example, BCSH guidelines recommend that bridging therapy is considered if an INR becomes significantly subtherapeutic within the first month following a VTE, owing to the risk of recurrence and mortality[5]
.
Causes of a subtherapeutic INR
Pharmacists and healthcare professionals are often involved in the management of both inpatients and outpatients with subtherapeutic INRs. They may be responsible for managing the patient themselves, or may be asked to provide advice to guide the medical team’s treatment of a patient. Consideration of what has caused a subtherapeutic INR is an important factor in the subsequent management decision. Causative factors include the potential for any omitted doses; any recent diarrhoea and/or vomiting or other illness; changes to concomitant medication; and diet or lifestyle changes. Some of these factors are further discussed below and summarised in ‘Box 1: Possible causes of a low subtherapeutic INR.’
Box 1: Possible causes of a low subtherapeutic international normalised ratio (INR)
- Interruptions owing to procedures that necessitate warfarin discontinuation;
- Recent administration of vitamin K;
- Non-adherence to treatment (intentional or non-intentional);
- Diarrhoea and/or vomiting;
- Recent dose reductions (e.g. to correct a previously high INR);
- Changes in concomitant drug therapy (including herbal medication);
- Dietary and lifestyle effects:
- Increase in dietary vitamin K intake;
- Use of vitamin supplements;
- Use of soya protein;
- Changes in smoking status;
- Increased levels of physical activity;
- Changes in disease status of comorbidities.
Interruptions owing to procedures
Treatment with warfarin therapy may be interrupted owing to certain procedures, such as surgery, which may have an associated bleeding risk. In such cases, the patient’s risk of thrombosis if warfarin is stopped versus bleeding will be evaluated in a pre-assessment clinic, usually following a local protocol. For some invasive procedures (e.g. joint injections, cataracts surgery or some endoscopic procedures), the risk of bleeding is low, therefore, warfarin will usually be continued[5],[6]
. However, for some surgical procedures (e.g. joint arthroplasty, nephrectomy or spinal surgery), the bleeding risk requires temporary discontinuation of warfarin[7]
.
Depending on the risk of thrombosis, bridging therapy may be given in the peri-operative period, using either low-molecular-weight heparin (LMWH) or unfractionated heparin (UFH)[6]
.
Following surgery, warfarin therapy can usually be restarted, using the patient’s usual maintenance dose 12–24 hours post-operatively and when there is adequate haemostasis[7]
. If bridging therapy has been required, this will be continued until stable anticoagulation is re-established with warfarin.
In the case of emergency surgery, it may be necessary to intravenously administer vitamin K (in the form of phytomenadione) in order to reverse the effect of warfarin. As this can take 6–12 hours, it is only suitable if surgery can be delayed for this period of time. For surgery that cannot be delayed, the INR can be reversed using prothrombin complex concentrate (PCC) and intravenous vitamin K[5]
.
Use of vitamin K
Vitamin K is administered either orally or intravenously to reverse the effects of warfarin. Owing to the risk of intramuscular haematoma, the intramuscular route is avoided, and it is not given subcutaneously owing to inconsistent correction. Intravenous administration produces a more rapid correction of the INR than oral administration, with significant correction observed within six to eight hours, and is used to treat high INR associated with non-major bleeding. Oral vitamin K at a dose of 1–5mg is administered to correct high INR (>8) in non-bleeding patients. Resistance to anticoagulation does not occur when oral vitamin K is given at these doses[5]
.
The use of vitamin K can interfere with warfarin treatment for up to a further two to three weeks following administration of a dose; this should be considered when treatment is re-initiated[8]
. If the patient is discharged back to their usual warfarin clinic provider, it is important that information regarding administration of vitamin K is communicated so that this can be taken into account when reviewing INR results.
Non-adherence to treatment
Patients may be intentionally or unintentionally non-adherent with warfarin treatment, and this is an important factor to consider when elucidating the reason for a subtherapeutic INR.
Examples of unintentional non-adherence to warfarin treatment include patients misunderstanding the dosage instructions or forgetting to take doses.
Where non-adherence results from difficulty remembering to take doses (e.g. owing to busy lifestyles or shift work), strategies for remembering can be discussed. Examples include, linking medication administration to a regular activity (e.g. teeth brushing) or setting an alert on a mobile phone. Patients are usually advised to take warfarin in the evening; however, if this is difficult to remember, then switching to morning administration may help (as long as following doses continue to be taken at this same time of the day).
A patient’s beliefs and preferences will influence adherence to warfarin treatment, and intentional non-adherence can occur when perceptions about the necessity for treatment do not outweigh concerns about various adverse effects[9]
. Research suggests that the likelihood of subtherapeutic INR is dependent on the indication for anticoagulation and associated perceived risk, with the highest likelihood found among patients taking anticoagulation for prophylaxis of VTE following surgery or in other high-risk situations, and the lowest likelihood in those with mechanical heart valves[10]
.
It is useful to check patients’ understanding of the reasons for taking warfarin therapy and the risks associated with non-adherence. For example, in patients with AF, it may be useful to discuss the annual stroke risk (extrapolated to a five- or ten-year stroke risk).
It is important that upon initiation of therapy, patients are counselled so that they understand the importance of taking warfarin treatment as advised and of maintaining a stable, therapeutic INR. Patients should be encouraged to inform their healthcare professional of any missed doses.
Diarrhoea and/or vomiting
Acute diarrhoea and/or vomiting can result in a low INR owing to reduced or incomplete absorption of warfarin from the gastrointestinal tract[11]
. Patients should be asked whether they have experienced any such symptoms (e.g. those associated with travel abroad) in the time prior to their INR being tested to ascertain whether this could have caused or contributed to a subtherapeutic INR. In a patient reporting recent diarrhoea or vomiting, it should also be considered that a reduced vitamin K intake as a result of this can lead to the reverse effect (i.e. a high INR).
Recent dose reductions
Consideration should be made to any recent alterations in dosage when assessing reasons for a low INR. A potential cause could be a prior dose reduction to correct a transiently high INR, which has resulted in lowering it to below the therapeutic range. For example, a patient may have previously had a high INR caused by taking another medication, which enhances the anticoagulant effect of warfarin (e.g. erythromycin), and their warfarin dose may have been reduced as a result[3]
. Upon discontinuation of the interacting drug (e.g. when the erythromycin course was completed), the INR may then fall to below the therapeutic range and it will be necessary to increase the warfarin dose back to the usual maintenance dose.
It has been argued that because of the obvious dangers of a high INR, there is a tendency towards under-anticoagulation in AF patients[12]
. Assessment of recent doses taken, including any recent dose reductions, is necessary to determine if a subtherapeutic INR is owing to insufficient warfarin intake, in which case an increase in dosage will be required to return the INR into the prescribed range.
Drug interactions
Upon initiation of warfarin therapy, patients should be counselled around the potential for drug interactions, as they can frequently be the cause of both sub and supratherapeutic INRs. It is necessary to ask patients at each INR check regarding any changes, or planned changes, to medication.
When considering changes in concomitant medication, it is necessary to consider the pharmacokinetic parameters involved and how this may affect the timeline of any effects on anticoagulation. For example, drugs that have a long half-life may continue to impact on INR control for a prolonged period following discontinuation. Rifampicin, which causes a reduction in INR, is an important example of this phenomenon — it can continue to have an effect for 2–5 weeks following discontinuation[13]
. Similarly, amiodarone tends to increase the INR and this effect is observed for several weeks owing to its long half-life. Therefore, if continuing the same dose of warfarin without adequate monitoring and appropriate warfarin dose adjustment, a subtherapeutic INR may be observed several weeks after stopping amiodarone.
Some drugs that have been shown to reduce the INR include rifamycins, spironolactone, sucralfate, trazodone, clozapine, atorvastatin, carbamazepine, phenobarbital and primidone[13]
,[14]
. Phenytoin causes an increased metabolism of warfarin and, therefore, decreased anticoagulant effect. However, it should be noted that increased INR with phenytoin has also been reported[3]
.
A consideration in patients who take analgesia is any changes in frequency or dose of painkillers (e.g. paracetamol or tramadol, both of which can affect INR). Pharmacists and healthcare professionals should ask patients about this in the post-operative period, where analgesia use is likely to decline over time.
Alcohol can have a variable effect on INR. Chronic heavy drinking can induce hepatic enzymes, leading to increased metabolism of warfarin, and these patients may require higher-than-average warfarin doses. Some evidence suggests that binge drinking in those with liver impairment may cause marked fluctuations in prothrombin time. This is thought to result from the excess alcohol disrupting general hepatic function[13]
.
Herbal medication can affect INR and it is recommended that such substances are avoided while taking warfarin. St John’s Wort, for example, has been shown to both decrease plasma concentrations and reduce the clinical effects of warfarin[15]
. Other herbal medications that may reduce response to warfarin include agrimony, goldenseal, mistletoe, yarrow, ginseng and coenzyme Q10[14]
.
Dietary and lifestyle effects
Intake of vitamin K can affect INR, as this will also affect production of the vitamin K-dependent clotting factors. One study found that vitamin K intake ≥250µg/day was associated with reduced warfarin sensitivity in patients on normal diets[16]
.
It is important to question a patient or carer regarding any recent changes to diet (see ‘Box 2: Examples of food rich in vitamin K’), including the use of any vitamin supplements. If a patient takes any purchased or prescribed dietary supplements or feeds, any changes should also be communicated to the pharmacist or healthcare professional monitoring INR because vitamin K content may vary between products. When counselling a patient who is to be started on warfarin therapy, it is important to ensure that they are aware of the potential for vitamin K to affect their INR, and that they know to inform their anticoagulant clinic should they decide to start any new supplements, or make any significant changes in their diet[4]
. However, the importance of maintaining a healthy, balanced diet should be discussed because over-emphasising the effect of dietary vitamin K can lead to some patients restricting their diet to an excessive and unnecessary extent.
Box 2: Examples of foods rich in vitamin K
- Green leafy vegetables;
- Chickpeas;
- Liver;
- Egg yolks;
- Cereals containing wheat bran and oats;
- Mature cheese;
- Blue cheese;
- Avocado;
- Olive oil.
Source: National Patient Safety Agency, Oral Anticoagulant Therapy: Important information for patients – also known as the “Yellow Book”
A change in INR may be observed when a patient moves between home and the hospital, resulting from changes in diet that can sometimes occur. Significant dose adjustments may be are required when moving between these settings.
Soya protein may modestly reduce the effects of warfarin, therefore, patients wishing to use soya protein, especially if in complete substitution for animal protein, should be advised that it may lower INR and that a timely review may be necessary[13]
.
Limited evidence suggests that smoking may decrease response to warfarin by causing a small increase in its clearance, therefore, it is pertinent to check a patient’s smoking status[13]
.
In addition, it is not unusual for a patient’s INR to be altered upon return from a holiday. This could be owing to a combination of factors, including a change in diet and alcohol consumption.
INR can also be influenced by varying levels of physical activity. One study found that patients with regular levels of physical activity (defined as ≥ 30min ≥ 3 times/week) had higher warfarin dose requirements compared with patients with lower levels of physical activity[17]
.
The effect of comorbidities on INR control
A subtherapeutic INR could be caused by a change in general medical condition. This can cause problems when a patient is acutely unwell, thus, close monitoring of INR may be necessary.
Disease states that are known to decrease INR include hypothyroidism, diabetes mellitus, oedema, hyperlipidaemia and visceral carcinoma[14]
.
Disease states that are known to increase response to warfarin include congestive heart failure, hepatic dysfunction, moderate-to-severe renal impairment, hyperthyroidism, infectious disease, menstrual disorders, malnutrition and cachexia[14]
. Improvements in disease status in these instances may cause a reduction in INR and necessitate an increase in warfarin dose.
For example, careful monitoring of INR is recommended in patients with thyroid disease, as dose requirements may change depending upon changes in thyroid status – higher doses are required in hypothyroid states and lower doses in hyperthyroidism. Likewise, careful monitoring of INR is required in congestive heart failure, as warfarin requirements can be increased or decreased depending on disease severity. Warfarin requirements have been found to change in the period following heart valve replacement surgery. In the immediate postoperative period, sensitivity to warfarin has been found to be increased. However, this effect is not sustained and careful monitoring of response, with an increase in dose, may be necessary to avoid a subtherapeutic INR[18]
.
Pharmacogenomics
Warfarin dosage requirements can be affected by variations in the genes responsible for its metabolism or pharmacodynamic response. While genetic variations are not commonly tested for, they may be if a patient is particularly warfarin resistant.
Cytochrome P-450 (CYP) isoenzyme 2C9 (CYP2C9) is the enzyme that is primarily responsible for metabolism of S -warfarin. Reduced clearance of warfarin is associated with variant alleles of CYP2C9, and patients expressing this phenotype require lower doses[14]
.
Warfarin exerts its anticoagulant effect by inhibiting vitamin K epoxide reductase, which controls the regeneration of reduced vitamin K from vitamin K epoxide. Reduced vitamin K is required for production of the vitamin K-dependent clotting factors. Variations in the gene that encodes this, vitamin K epoxide reductase complex subunit 1 (VKORC1), has been associated with variations in warfarin dose requirements[14]
.
Taking action when an INR is subtherapeutic
The action required depends on the risk of thrombosis and the cause of the low INR and this will vary depending on individual circumstances. As previously mentioned, BCSH guidelines advise that the use of bridging therapy should be considered if the INR becomes significantly subtherapeutic within the first month following an acute VTE. There is no clear consensus on what constitutes a ‘significant’ subtherapeutic INR in this instance, with some healthcare professionals classing <1.7 as significant, while others consider <1.5 as significant[5]
.
The risk of thromboembolism is high in patients with prosthetic heart valves; however, this varies depending on the type of valve, position of valve and individual patient factors (e.g. presence of AF or cardiac chamber dilatation)[19]
. Bridging therapy may be required if an INR becomes subtherapeutic and it is necessary to follow local protocols, which may include referral to a cardiologist. The decision to cover with LMWH may be influenced by the type of valve, how subtherapeutic and how long the INR has been subtherapeutic for (e.g. LMWH may be instituted sooner for an older style mitral valve than a newer style aortic valve). The daily thrombosis risk of a non-anticoagulated heart valve is around 0.01%, although the risk is greater with older thrombogenic valves and mitral valves rather than aortic valves[20]
.
Any adjustments in warfarin dosage will be dependent on the reason(s) for the subtherapeutic INR. A long-term cause (e.g. a permanent change in concomitant drug therapy or increased physical activity) will necessitate an increase in the weekly warfarin dose. However, it may not be appropriate to change the weekly warfarin dosage in the case of short-term causes (e.g. a missed dose or a short course of an interacting drug). If it is necessary to adjust the warfarin dosage, this can be done by altering the total weekly dose by 10–20%, taking into account the strength of available warfarin tablets[21]
.
A boost dose may occasionally be given if the patient is felt to be at higher thromboembolic risk. This boost dose consists of one or two doses that are given at a higher dose (usually around 50% greater than the patient’s regular dose). If the INR is low resulting from a long-term cause, then a boost dose may be given as well as increasing the total weekly dose.
Owing to warfarin’s mechanism of action, with the resulting slow and prolonged effect on INR, it is important to avoid over-responding to high or low results as this can lead to unnecessary INR instability. Time must be given to allow the INR to change in response to a dose adjustment and although in hospitalised patients several INRs may be taken each week, it is important to take an overall weekly view of the warfarin dose and INR. This will avoid “yo-yo” dosing and INR instability.
Financial and conflicts of interest disclosure:
The author has no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in the manuscript apart from those disclosed. No writing assistance was utilised in the production of this manuscript.
Reading this article counts towards your CPD
You can use the following forms to record your learning and action points from this article from Pharmaceutical Journal Publications.
Your CPD module results are stored against your account here at The Pharmaceutical Journal. You must be registered and logged into the site to do this. To review your module results, go to the ‘My Account’ tab and then ‘My CPD’.
Any training, learning or development activities that you undertake for CPD can also be recorded as evidence as part of your RPS Faculty practice-based portfolio when preparing for Faculty membership. To start your RPS Faculty journey today, access the portfolio and tools at www.rpharms.com/Faculty
If your learning was planned in advance, please click:
If your learning was spontaneous, please click:
References
[1] Support for commissioning: anticoagulation therapy: National Institute for Health and Care Excellence; 2013.
[2] Hirsh J, Dalen JE, Anderson DR et al. Oral anticoagulants: mechanism of action, clinical effectiveness, and optimal therapeutic range. Chest. 2001;119(1):8S–21S. doi: 10.1378/chest.119.1_suppl.8S
[3] Joint Formulary Committee. British National Formulary (online) London: BMJ Group and Pharmaceutical Press. Available at: http://www.medicinescomplete.com (accessed June 2016)
[4] The National Patient Safety Agency. Oral anticoagulant therapy: important information for patients. 2007. London. Available at: http://www.nrls.npsa.nhs.uk/resources/?EntryId45=61777 (accessed June 2016)
[5] Keeling D, Baglin T, Tait C et al. Guidelines on oral anticoagulation with warfarin - fourth edition. British Journal of Haematology 2011;154:311–324. doi: 10.1111/j.1365-2141.2011.08753.x
[6] Hammond R. Bridging anticoagulation: perioperative management of patients on anticoagulants.Clinical Pharmacist 2016;8:4. doi: 10.1211/CP.2016.20200956
[7] Douketis JD, Spyropoulos AC, Spencer FA et al. Perioperative management of antithrombotic therapy: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest 2012;141:e326S–350S. doi: 10.1378/chest.11-2298
[8] Konakion MM. 10mg/ml - summary of product characteristics (SPC) - (eMC). Available at: https://www.medicines.org.uk/emc/medicine/1698 (accessed April 2016)
[9] Horne R, Chapman SCE, Parham R et al. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the necessity-concerns framework. PLoS ONE. 2013;8(12): e80633. doi: 10.1371/journal.pone.0080633
[10] Rombouts EK, Rosendaal FR & van der Meer FJM. Subtherapeutic oral anticoagulant therapy: frequency and risk factors. Thrombosis and Haemostasis. 2009;101:552–556. doi: 10.1160/TH08-09-0626
[11] Nathan A. Treating acute diarrhoea in adults. The Pharmaceutical Journal. 2008;281:217 Available at: URI: 10027800
[12] Hylek EM & Rose AJ. Understanding low INR in clinical practice. Thrombosis and Haemostasis. 2009;101:417–418. doi: 10.1160/TH09-01-0067
[13] Baxter K (ed), Stockley’s Drug Interactions. [online] London: Pharmaceutical Press. Available at: http://www.medicinescomplete.com/ (accessed June 2016)
[14] AHFS: AHFS Drug information, Bethesda: American Society of Health-System Pharmacists. 2012. Available at: http://www.medicinescomplete.com/mc/ahfs/current/ (accessed June 2016)
[15] Marevan 5mg tablets - Summary of Product Characteristics (SPC) - (eMC). Available at: http://www.medicines.org.uk/emc/medicine/21596/SPC/Marevan+5mg+tablets (accessed April 2016)
[16] Lubetsky A, Dekel-Stern E, Chetrit et al. Vitamin K intake and sensitivity to warfarin in patients consuming regular diets. Thrombosis and Haemostasis. 1999;81(3):396–399. PMID: 10102468
[17] Shendre A, Beasley TM, Brown TM et al. Influence of regular physical activity on warfarin dose and risk of hemorrhagic complications: physical activity and warfarin response. Pharmacotherapy 2014;34(6):545–554. doi: 10.1002/phar.1401
[18] Rahman M, BinEsmael TM, Payne N et al. Increased sensitivity to warfarin after heart valve replacement. Ann Pharmacother.2006;40: 97–401. doi: 10.1345/aph.1G407
[19] Scottish Intercollegiate Guidelines Network. SIGN 129: Antithrombotics: indications and management. A national clinical guideline. 2013. Available at: http://www.sign.ac.uk/guidelines/fulltext/129/index.html (accessed June 2016)
[20] Cannegieter SC, Rosendaal FR & Briet E. Thromboembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation 1994;89(2):635–641. doi: 10.1161/01.CIR.89.2.635 9
[21] Kim YK, Nieuwlaat R, Connolly SJ et al. Effect of a simple two-step warfarin dosing algorithm on anticoagulant control as measured by time in therapeutic range: a pilot study. Journal of Thrombosis and Haemostasis. 2010;8(1):101–106. doi: 10.1111/j.1538-7836.2009.03652.x
[22] Vahanian A, Baumgartner H, Bax H et al. Guidelines on the management of valvular heart disease. European Heart Journal. 2007;28(2):230–268. doi: 10.1093/eurheartj/ehl428