This content was published in 2007. We do not recommend that you take any clinical decisions based on this information without first ensuring you hvave checked the latest guidance.
Identify knowledge gaps
- What is blepharitis and how is it treated?
- What factors should you consider when recommending a product over the counter for dry eyes?
- Look at the picture below. What is this condition and how should it be treated?
Before reading on, think about how this article may help you to do your job better. The Royal Pharmaceutical Society’s areas of competence for pharmacists are listed in “Plan and record”, (available at: www.rpsgb.org/education). This article relates to “common disease states” (see appendix 4 of “Plan and record”).
Pharmacies are now often the first port of call for treatment of bacterial or allergic conjunctivitis, but pharmacists can also encounter many other eye conditions. This article outlines eye conditions with visible signs. Asymptomatic diseases, such as glaucoma, are not covered.
Arcus senilis
Arcus senilis is caused by lipid deposition in the cornea. This appears as a white ring in the periphery of the cornea (see Figure 1). The white ring usually appears first at a 12 o’clock position and at a six o’clock position, then extends round the corneal periphery. Vision is not affected.
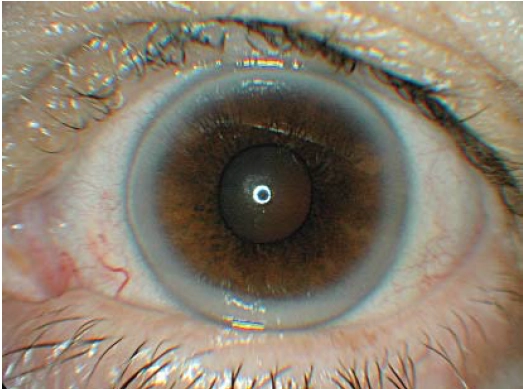
Source: Marvyn Elton
Arcus senilis is common in the elderly. If it appears in people under 40 years of age, a lipid profile should be recommended to rule out hyperlipidaemia, hypercholesterolaemia and hyperlipoproteinaemia.
Blepharitis
Blepharitis simply means inflammation of the eyelid margin. The patient will usually complain of an itchy, gritty, uncomfortable eye, and will want to rub it. The eye may or may not be red. Blepharitis usually affects the lower eyelid. The eyelashes can be waxed together (to a point) and there may be dandruff-like scales in the eyelashes (see Figure 2) or at the base of the eyelashes.

Source: Marvyn Elton
In heavy blepharitis the scales are situated throughout the eyelashes and at the base of the eyelashes. Blepharitis can be classified as seborrhoeic or bacterial. Bacterial blepharitis can lead to bacterial conjunctivitis. Seborrhoeic blepharitis tends to occur more often in people with oily skin.
“Lid toilet” is the first-line treatment. This involves mixing two parts of baby shampoo with 10 parts of warm water. The lower eyelid is pulled down and the solution is applied with a cotton-wool ball or bud, wiping it along the base of the eyelashes. This should be done twice a day for several weeks. People with blepharitis should be told it is a chronic condition.
If lid toilet does not work (an improvement would be expected after four weeks), an antibiotic eye ointment can be used to eradicate any bacteria present — Staphylococcus aureus is usually the main culprit. Chloramphenicol eye ointment can be rubbed into the eyelashes and at the base of the lashes two or three times a day for seven days. An alternative is to use fusidic acid viscous drops. Fusidic acid is active against Gram positive bacteria, for example, Staphylococcus aureus and Staphylococcus epidermidis. It should be used twice a day for seven days.
Glossary
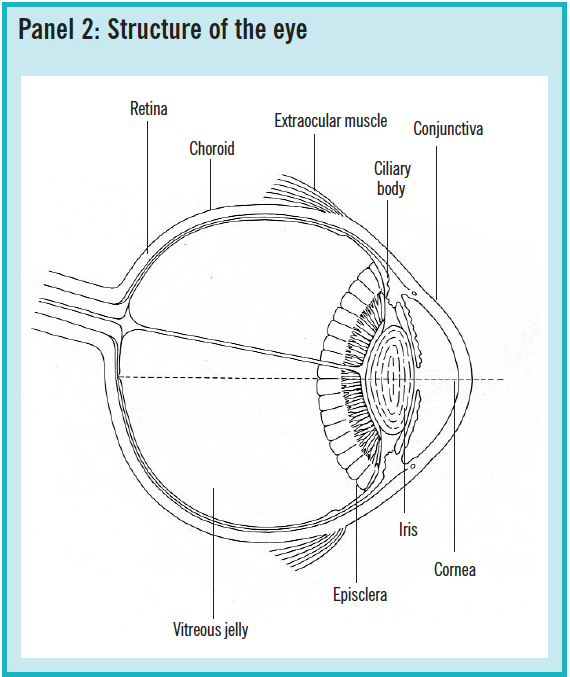
Conjunctiva The conjunctiva is the membrane covering the white of the eye (bulbar conjunctiva) and lining the inside of the eyelids (palpebral conjunctiva)
Cornea The cornea is the clear dome-shaped surface at the front part of the eye, covering the iris, pupil, and anterior chamber
Episclera The episclera is the layer of connective tissue between the sclera (white of the eye) and the conjunctiva. See Panel 2 below.
Conjunctivitis
The four main types of conjunctivitis (bacterial, adenoviral, allergic and chlamydial) were discussed in a previous CPD article (PJ, 11 June 2005, pp725–8).
Dry eye syndrome
Dry eye syndrome is usually due to a deficiency of the aqueous component of tears (see Panel 1).
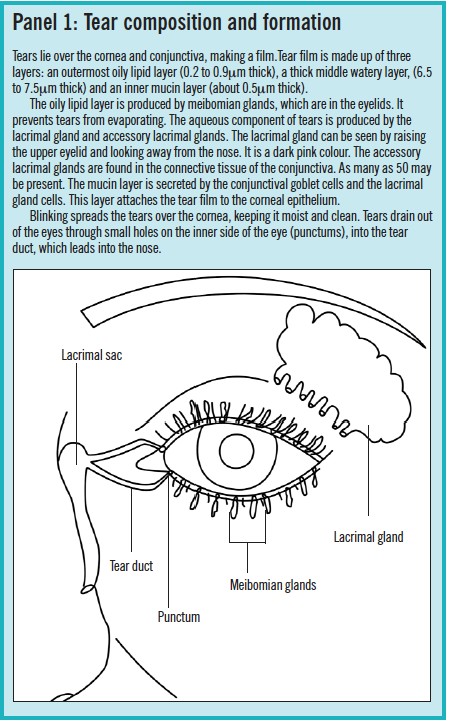
Patients with dry eyes will commonly complain of discomfort and soreness. They may also feel as if something is in the eyes and their vision can sometimes become blurred. Dry eyes are more common in the elderly (tear production decreases with age) and menopausal or postmenopausal women. With increasing age, the lower eyelid may also turn outward (known as ectropion) due to a weakening of the eyelid muscles. This causes the conjunctiva to become dry because, on blinking, the lower eyelid does not cover the lower conjunctiva and cornea. In addition to ageing, causes of dry eyes include:
- Medicines (eg, oral contraceptives, firstgeneration antihistamines, beta-blockers, anticholinergics)
- Diseases (eg, Sjögren’s syndrome [an immunological disorder involving reduced secretion from a number of glands], rheumatoid arthritis, sarcoidosis)
- Damage to the eye (eg, conjunctival scarring can occur as a result of Stevens-Johnson syndrome)
- Blinking problems (eg, after injury or stroke)
- Environmental factors (eg, working in an air-conditioned office)
The main treatment for dry eyes is to instil “artificial tears”. However, dry eye syndrome is probably over-diagnosed and, often, the underlying cause of a sore, uncomfortable eye is blepharitis. The difference between the two can be subtle. My personal preference is, therefore, to first look for blepharitis and treat this if necessary. Only if the blepharitis treatment were unsuccessful would I recommend artificial tears to treat dry eyes.
There are many artificial tear preparations to choose from. First, there is a basic choice between drops and ointments. Ointments are less convenient to use during the day because they can blur vision. The traditional remedy for dry eyes is hypromellose drops, instilled as often as required. These are available in concentrations from 0.1 per cent and 1 per cent. I usually recommend the 0.3 per cent strength. In my opinion, there is no difference between the strengths available and their effects. According to Alcon, which manufactures hypromellose at 0.5 per cent (Isopto Plain) and 1 per cent (Isopto Alkaline), the 1 per cent drop has more lubricating power because of the higher hypromellose content.
Drops can be divided into those which contain a preservative and those which do not. The preservative is nearly always benzalkonium chloride, usually present at 0.01 per cent. Preservatives can destabilise the lipid layer of the tear film and affect its surface tension. This can damage the corneal epithelium. If a patient is likely to be using artificial tears for a long time, a preservative-free preparation should be considered although these can be more expensive. Preservative-free eyeointments include Lacri-Lube and Simple Eye Ointment.
Some eye drops, particularly those containing carbomers, have a thicker consistency than others. For example, GelTears, Viscotears are carbomer-based and Tears Naturale contains the thickening agent dextran 70. It is claimed that, because these products are more viscous, the drop stays in contact with the surface of the eye for longer and the product needs to be instilled less frequently. However, if the product contains a preservative, this may not be so desirable. For patients requiring a viscose, preservative-free eye drop, Viscotears is available in single dose units.
In the British National Formulary, some artificial tears products are indicated for “dry eye conditions” and others are indicated for “tear deficiency”. In my opinion, however, products indicated for tear deficiency are interchangeable with those indicated for dry eye conditions — they do the same thing, regardless of whether dryness is caused by decreased tear production or something like ectropion.
In severe cases of dry eyes, a specialist may offer to insert punctum plugs to prevent tears draining into the tear duct. For dry eyes in Sjögren’s syndrome, pilocarpine tablets (5mg four times a day) are prescribed.
Pharmacists can advise patients with dry eyes to avoid smoky or low humidity environments, to avoid looking at a monitor or watching television for long periods and to try to blink more often. Pharmacists should also ensure that patients who use eye drops to treat other conditions, such as glaucoma, leave at least five minutes between instilling their eye drops and their artificial tears, to allow the drug to be absorbed. The lower conjunctival sac is not big enough to hold two drops and using two products one after another can result in the second drop flushing out the first.
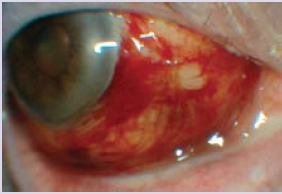
Episcleritis
Episcleritis is inflammation of the episclera, which covers the white of the eye (sclera) and lies underneath the conjunctiva. This presents as redness. Sectoral episcleritis, where only one part of the episclera is affected (see Figure 3), is more common than diffuse episcleritis where most of the white of the eye is red. The redness is due to dilation of the episcleral blood vessels, large vessels that run radially underneath the conjunctiva.
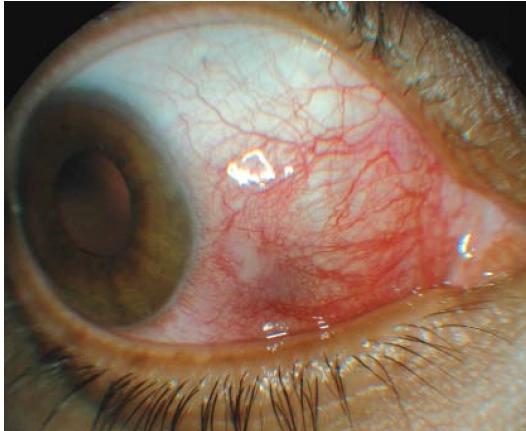
Source: Marvyn Elton
Patients usually present with an “uncomfortable eye”. If pain is present, it is usually mild. Episcleritis has been associated with rheumatoid arthritis but most cases are idiopathic. A mild topical steroid (eg, prednisolone 0.5 per cent drops) can be prescribed. Doses vary, but one example is one drop three times a day for five days, then one drop twice a day for five days, then one drop daily for a further five days.
See also the section on “red eyes”.
Floaters
“Floaters” are dark objects that travel across the field of vision. They are shadows of material suspended in the vitreous jelly that fills the back of the eye. The patient will typically complain of a “moving dot” in front of one eye or a “spiders web” or “mist”. Patients also commonly report that these move across the field of vision as the eye moves.
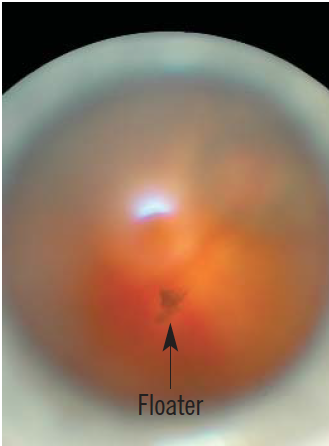
Source: Marvyn Elton
The most likely cause of this symptom is a posterior vitreous detachment (PVD). In a young eye, the vitreous jelly is attached to the retina, which is the layer of neural cells lining the back of the eye. With increasing age, there is liquefaction of the vitreous jelly, which becomes more likely to detach from the retina. This condition is common; in a study of autopsies, PVDs were observed in 63 per cent of those over 70 years of age.1
In most cases, the vitreous jelly detaches from the retina and leaves the retina flat. Most PVDs are not treated and a patient with a floater will get used to its presence. However, the eye should be examined because if the jelly detaches and pulls on the retina, this can cause a retinal tear. When the jelly pulls on the retina, the patient may experience “flashing lights”. These can be differentiated from the flashing lights that some migraine sufferers experience because they are not zig-zag shaped. When the jelly detaches from the retina, it may also pull on a retinal blood vessel causing a bleed at the back of the eye.
Retinal tears are nearly always in the retinal periphery so are difficult to see on examination. Retinal tears can be sealed with laser treatment, which is a relatively easy procedure. If, however, a retinal tear is missed or the patient does not bother to have an examination the tear could progress to a retinal detachment. A retinal detachment means the retina falls off the back of the eye and a major eye operation is required to try to save the patient’s sight. The problem should, therefore, be stopped at the retinal tear stage. Seeing a black shadow or black curtain is more likely to be a sign of a retinal detachment.
Pharmacists should refer patients complaining about a new floater, with or without flashing lights and with or without a black shadow, to an optometrist or GP as soon as possible. The optometrist should, as a minimum, carry out indirect ophthalmoscopy: eye drops (eg, tropicamide 1 per cent) are used to dilate the pupil so that the retina can be examined using a slit lamp and lens.
Herpes simplex
Infection with herpes simplex is extremely common — about 90 per cent of the population carry herpes simplex antibodies. Primary infections with herpes simplex usually occur between the ages of six months and five years. This may involve typical symptoms of a viral illness (eg, swollen lymph glands, malaise, sore throat) or the infection may be subclinical.
There are two types of herpes simplex: HSV-1 (which infects the face, lips and eyes) and HSV-2 (which causes genital infections). When the primary infection occurs, the herpes virus travels up the sensory nerve (the trigeminal nerve in the case of HSV-1) to its ganglion, where it lies dormant. On reactivation, the virus travels down the sensory nerve to the target tissue where it causes active disease.
The patient will usually present with an uncomfortable eye and, perhaps, blurred vision. Other signs include pain (usually mild), redness, tearing and light sensitivity. There may be accompanying herpetic vesicles on the eyelid or periocular skin (see Figure 4). The patient may have had a herpes simplex infection in the eye before.

Source: Marvyn Elton
HSV-1 typically affects the eyelids, conjunctiva, and cornea. If the cornea is infected, the active disease is called herpes keratitis. At the optometrist, the infection typically presents as a dendritic ulcer (a branching tree-like lesion), which can be seen on examination with a slit lamp. The dendritic ulcer affects the corneal epithelium, which is the outermost layer of the cornea.
For a corneal dendritic ulcer, aciclovir 3 per cent eye ointment applied five times a day to the affected eye is usually effective. A 1cm line of ointment should be placed inside the lower conjunctival sac and the eye kept closed for 30 seconds after application. Two weeks’ treatment should be sufficient. In some cases, oral treatment may be required. Patients who suffer severe or recurrent infections are at higher risk of corneal scarring.
For periocular herpetic vesicles, aciclovir cream is used.
This article will continue on 3 March. Conditions covered will include styes and subconjunctival haemorrhage.
You might also be interested in…

Identification and management of common eye disorders

Glaucoma: an overview
