This content was published in 2007. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
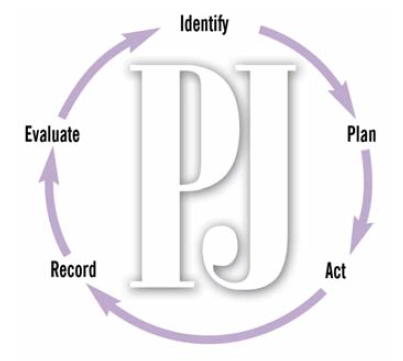
Marginal keratitis
Marginal keratitis (inflammation of the cornea) is a corneal ulcer thought to be caused by a hypersensitivity reaction to staphylococcus species. It is particularly common in patients with blepharitis. The patient presents with a red, uncomfortable eye. If examined with a slit lamp, a white corneal ulcer, usually in the periphery of the cornea, will be seen.
Treatment with a topical steroid is effective. A strong steroid eye drop (eg, Maxidex or Pred Forte) can be prescribed. A treatment regimen of one drop tds for seven days, then one drop bd for seven days, then one drop od for seven days is recommended. As with other strong steroids, the dosage should be reduced gradually. Associated blepharitis should be treated with chloramphenicol eye ointment first line.
Source: Marvyn Elton
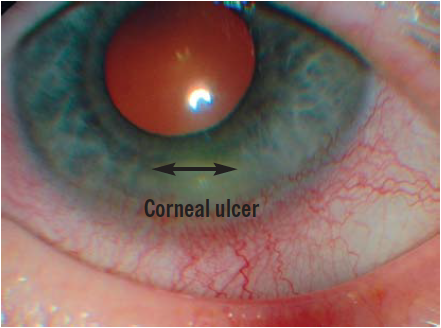
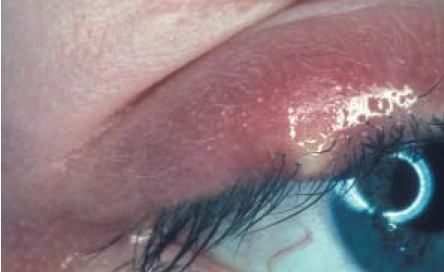
Meibomian cysts
The meibomian glands are modified sebaceous glands that secrete a lipid material onto the tear film which prevents the tears from evaporating. The glands are located in the tarsal plates (thin plates of connective tissue) situated in the middle of each eyelid. The eye lids contain between 50 and 70 meibomian glands and the openings of the meibomian gland ducts are located behind the eyelashes.
Blockage of the passage of the lipid down the gland duct causes a pea-like swelling called a meibomian cyst (see Figure 6 for two examples). This is an inflammatory lesion and not an infection and if this cyst is touched, it will not be painful compared with touching a stye (see below).
Source: Marvyn Elton
Small meibomian cysts often spontaneously resolve. If the meibomian cyst does not resolve, then a warm compress can be held against the cyst for a couple of minutes to warm the oils which are not flowing properly, then the cyst should be massaged for about a minute. This should be done every day to try to resolve the cyst. If this does not work, a hospital visit is necessary, where the eyelid will be everted and the cyst clamped and incised. Larger cysts (1cm) usually need this treatment.
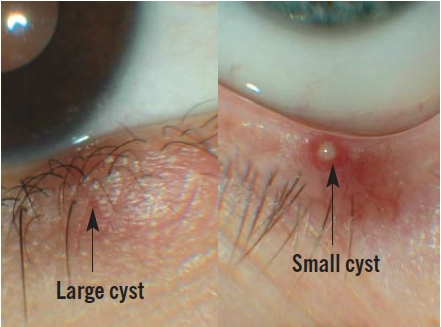
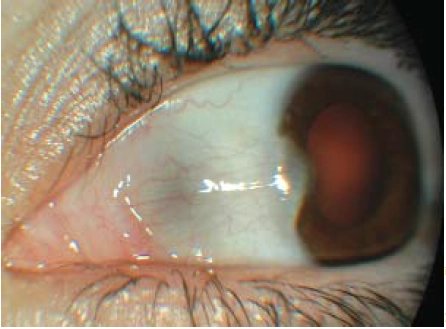
Naevi
A naevus (mole) can appear on the conjunctiva during puberty or early adult life (see Figure 7). A conjunctival naevus can be either flat or slightly elevated and it commonly occurs on the bulbar conjunctiva. It may or may not be pigmented and the degree of pigmentation can change with time.

Source: Marvyn Elton
Iris naevi or freckles can also occur. Like conjunctival naevi, these are commonly benign tumours. They are also flat or slightly elevated. They do not usually distort the surrounding structures, such as the pupil, so if an adjacent structure is distorted, then a malignant iris melanoma would be suspected. The presence of many iris naevi (called Lisch nodules) is a classic sign of neurofibromatosis type 1, an autoimmune disease.
Glossary
Choroid The choroid lies between the retina and sclera. It is made up of blood vessels that supply the back of the eye. The choroid is joined to the ciliary body and to edges of the optic nerve at the back of the eye.
Ciliary body The ciliary body lies just behind the iris. Attached to the ciliary body are tiny fibres that suspend the lens in the eye. The ciliary body produces aqueous humor (clear fluid that fills the front of the eye) and controls accommodation by changing the shape of the crystalline lens through contracting and relaxing.
Iris The iris is the coloured part of the eye. It controls light levels inside the eye.
See Panel 2 below
Pingueculae
A pinguecula is a yellow-white, flat or slightly raised conjunctival lesion that typically appears on the white of the eye (see Figure 8). A pinguecula does not encroach onto the cornea.
Source: Marvyn Elton
Pingueculae are common and are a sign of conjunctival ageing. A histological examination will show degeneration of collagen fibres in the conjunctiva, thinning of the conjunctival epithelium and, occasionally, calcification. Pingueculae are benign lesions and no treatment is usually indicated. However, if a pinguecula becomes inflamed the eye can feel uncomfortable and look red. An inflamed pinguecula can be treated with a mild steroid eye drop (eg, prednisolone 0.5 per cent). The usual dosage regimen is one drop to be instilled three times a day for five days, then one drop twice a day for five days, and finally one drop daily for five days.
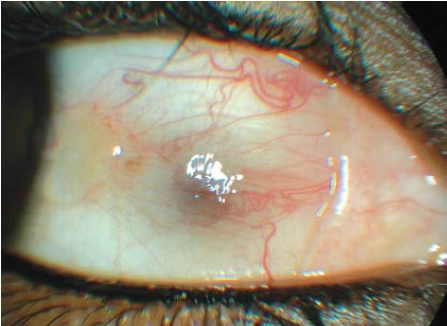
Pterygia
A pterygium is a wing of fibrovascular tissue arising from the nasal corner of the eye and growing over the conjunctiva (see Figure 9). Unlike pingueculae, pterygia can encroach onto the cornea. A pterygium is a benign lesion lesion and is more common in people who live in hot countries. Treatment (by surgical excision) is indicated for cosmetic reasons or if the pterygium is getting so close to the pupil that there is a risk of blurred vision.
Source: Marvyn Elton
Red eyes
Pharmacists are often asked for treatment for red eyes, where the customer’s main concern is the appearance of his or her eyes. Several eye drops containing naphazoline hydrochloride are marketed for red eyes (eg, Optrex Red Eye, Murine). Naphazoline acts on alpha-adrenergic receptors in the walls of blood vessels, causing them to constrict and, therefore, redness is reduced.
I prefer not to recommend such products, but pharmacists wishing to do so should ensure that the redness is not a symptom of a more serious condition, such as episcleritis or uveitis (see below), which requires investigation. The cause must be obviously connected to lifestyle, for example, the customer may say that he or she has been in a smoky environment or has had little sleep. The eyes will not be painful. As with many other eye drops, products for reducing redness are not suitable for contact lens wearers.
Styes
A stye (or external hordeolum) is a staphylococcal (usually Staphylococcus aureus) infection of an eyelash follicle and/or its associated gland of Zeis (a modified sebaceous gland) or gland of Moll (a modified sweat gland). It typically presents as a red swelling at the anterior (outside the eyelashes) eyelid margin (see Figure 10). Because the cause is bacterial, pus can usually be seen and, if touched, a stye can be painful.
Source: Marvyn Elton
Without treatment, a stye will usually resolve within seven to 14 days. Pulling out the eyelash can quicken the recovery and applying a warm compress may be helpful. If the infection spreads the whole eyelid can swell and a systemic antibiotic will be necessary. Subconjunctival haemorrhage A subconjunctival haemorrhage is a bleed from a small blood vessel, resulting in a bright red patch of blood in the eye (see Figure 11). The blood can cover the whole of the white of the eye (sclera) or can be in just one sector, but the eye is not painful.

Source: Marvyn Elton
In many cases, the patient will wake up with the haemorrhage, which is not noticed until he or she looks in a mirror. The condition appears alarming but is usually harmless.
No treatment is indicated and the patient can be reassured that the blood will clear gradually within seven to 14 days. Most subconjunctival haemorrhages are idiopathic. Some can be caused by trauma (eg, by coughing or sneezing). Hypertension is also a possible cause so pharmacists can advise patients to have their blood pressure checked.
Anticoagulant drugs (eg, warfarin, aspirin, clopidogrel) can also cause a haemorrhage so patients should be asked about their medicines and those taking warfarin should have their international normalised ratio measured.
Trichiasis
Trichiasis is the ingrowing of the eyelashes. Ingrowing eyelashes can rub against the cornea (especially as the patient blinks) causing discomfort and possible abrasion. Treatment involves pulling the eyelash or lashes out with a fine tipped medical tweezer, but these can regrow within four to six weeks and may need to be pulled out again. Alternative treatments include electrolysis and cryotherapy of the hair follicles.
Uveitis
The uvea is made up of the iris, the ciliary body and the choroid. There are different types of uveitis and treatment depends on the part of the uvea affected. The most common form of uveitis is iritis (inflammation of the iris). It is associated with inflammatory conditions, such as arthritis and Crohn’s disease, but can also be idiopathic. The patient’s eye will be red. In textbooks, the redness is typically shown around the iris, but this is not always the case.
The patient will usually complain of pain (or at least discomfort) in the eye. Other symptoms can include blurred vision and sensitivity to light. Iritis is diagnosed by finding white blood cells in the aqueous fluid of the eye. This requires a slit lamp, so a person with suspected uveitis should be referred to an optometrist.
Iritis requires treatment with steroid eye drops to alleviate the pain and inflammation, and to prevent complications from developing. A mydriatic drop (usually cyclopentolate 1 per cent) is sometimes used in addition to the steroid.
Watery eyes
Tears are necessary to keep the eye lubricated and clean. Increased tear production accompanies actions, such as yawning and laughing, and is a reflex to irritation (eg, wind, cold weather, dust). However, other causes of watery eyes (epiphora) include: dry eyes (tear production is stimulated by dryness), blepharitis, allergy and infection. Treatment will depend on the cause. Prolonged excessive tear production is undesirable and may also be caused by a blocked tear duct. This can be treated in hospital with syringing.
Xanthelasmata
Xanthelasmata are pale yellow lesions that occur most commonly on or just above the upper eyelids (see Figure 12). They are composed of lipids. About one in three people with a xanthelasma has a raised blood cholesterol level so patients should be advised to have their cholesterol levels checked. Xanthelasmata can be removed by cosmetic surgery, but most patients reject it.
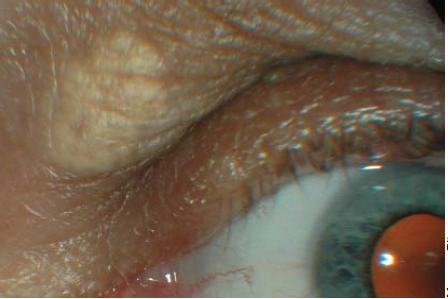
Source: Marvyn Elton
Conclusion
Symptoms such as redness, dryness, discomfort and tearing are signs that are common to many ocular conditions. Giving the correct advice depends on the pharmacist being able to determine the most likely condition(s) and this involves asking the right questions. Panel 3 lists some helpful questions that pharmacists might consider asking patients presenting with an eye problem.
Panel 3: Consultation questions for eye conditions
- When did the problem start?
- Is this the first time it has happened?
- Is there a pattern to the occurrences (eg, all the time or on and off?)
- Are both eyes affected?
- Is the eye painful or uncomfortable?
- Is your vision affected?
- Is there an obvious cause (eg, injury)?
- Do you wear contact lenses?
- Do you have any joint or muscle pains?
- Are you frequently exposed to wind, dust. chemicals, sun, light, air conditioning?
- Do you use a computer for long periods?
As a precaution, pharmacists should always advise patients to whom they supply eye drops over the counter to seek further advice if the symptoms do not improve within two days. If in any doubt, the patient should be referred to an optometrist or to eye casualty.
The following patients should be referred:
- Those with red eyes and pain
- Those with blurred vision
- Those who wear soft contact lenses (This is so that Pseudomonas aeruginosa and acanthamoeba infections can be excluded. Pseudomonas infections can develop rapidly — the eye can fill with pus within 24 hours. Both infections carry a high risk of permanent blindness.) Soft contact lens wearers with a red painful eye should be urgently referred.
Action: practice points
Reading is only one way to undertake CPD and the Society will expect to see various approaches in a pharmacist’s CPD portfolio.
- Make a list of preservative-free artificial tear preparations.
- Who are your local optometrists? Get to know them and find out about their practices. For example, can they perform indirect ophthalmoscopy? Do they take walk in patients? What do they charge for an examination? What are their opening hours? Do they have preferences for how patients are referred to them?
- Some eye conditions are connected to hypertension or hypercholesterolaemia. Consider offering services to look for these conditions in people visiting your pharmacy.
Evaluate
For your work to be presented as CPD, you need to evaluate your reading and any other activities. Answer the following questions: What have you learnt? How has it added value to your practice? (Have you applied this learning or had any feedback?) What will you do now and how will this be achieved?
References
1. Retina and vitreous. In: Basic and clinical science course 1996–1997. American Academy of Ophthalmology.
Resources
- Kanski JJ. Clinical ophthalmology (3rd edition). London: Butterworth-Heinemann Ltd; 1994.
- Cullom JR, Chang JB. The Wills eye manual: office and emergency room diagnosis and treatment of eye disease (2nd edition). Philadelphia: Lippincott Company; 1994.
You might also be interested in…

Identification and management of common eye disorders

Glaucoma: an overview
