Biophoto Associates / Science Photo Library
John Manning is a 27-year-old man in good health and is not prescribed any regular medicines. He visits the pharmacy to ask your advice about athlete’s foot. He explains that he has recently started training for a marathon and has developed an itchy area on his left foot.
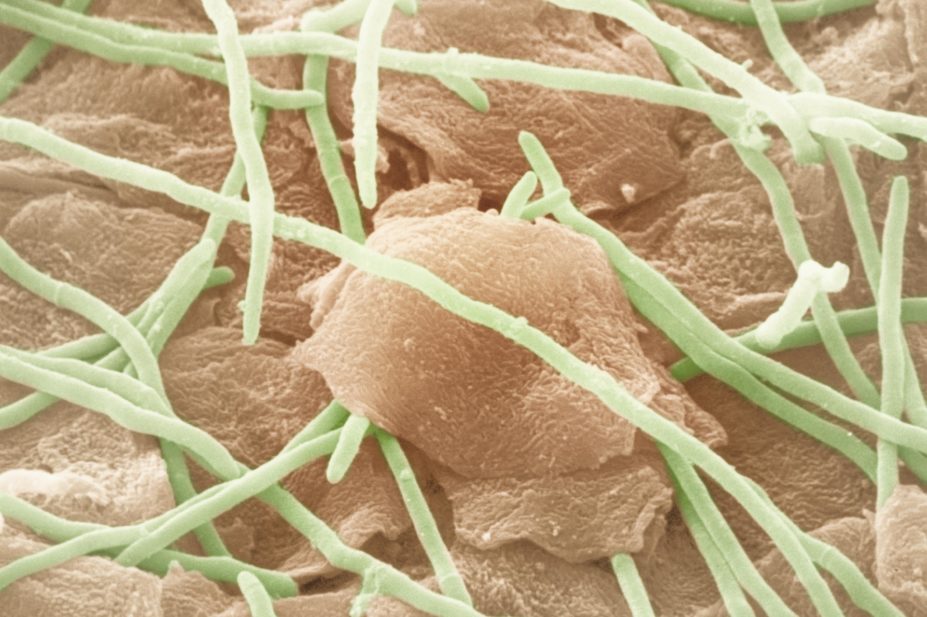
Athlete’s foot, or tinea pedis, is a fungal skin infection estimated to affect more than 15% of the world’s population[1]
. It is predominantly caused by Trichophyton rubrum and T. interdigitale but can also be caused by Epidermophyton floccosum. There is limited data on prevalence, although it is believed to be twice as common in men[2]
. It is more common in adults aged 15–40 years.
Risk factors for developing athlete’s foot include having damp feet (e.g., keeping damp socks on, wearing tight shoes with little ventilation, or wearing shoes and socks for long periods); walking barefoot in communal areas such as locker rooms and showers; sharing bed linen, towels or shoes with someone who is infected; and having a compromised immune system.
The signs and symptoms of athlete’s foot can include:
- Itching
- Redness
- Dry, flaking skin and diffuse scaling
- Maceration (white, soggy skin, especially between the toes)
- Splitting/fissures (especially between the fourth and fifth toes)
- Burning, inflammation and pain
- Unpleasant smell
Athlete’s foot is characterised by a rash which usually first appears between the toes, often in the space between the fourth and fifth toes. This rash can appear similar to psoriasis. The diagnosis can be confirmed by skin microscopy, although this is often only necessary if antifungal treatment fails.
Although it is a relatively superficial condition, athlete’s foot should be treated as soon as possible because the infection can spread to the soles and sides of the foot. It can also result in onychomycosis, or fungal infection of the nail.
Moccasin-type athlete’s foot affects the whole of the sole and sides of the feet. The sole shows silvery, fine scaling and the underlying skin is usually inflamed. Most patients with moccasin-type athlete’s foot will also have onychomycosis. It is often recalcitrant to topical antifungal treatment and patients should be referred to their GP.
Vesicular athlete’s foot is characterised by small blisters on the instep of the foot. It is believed these are caused by an allergic reaction to the fungal infection.
Other body areas can also be affected and athlete’s foot is frequently associated with tinea cruris, or fungal groin infection.
Patients with athlete’s foot may develop secondary bacterial skin infections, including cellulitis, as a result of cracks in the dry skin allowing the entry of bacteria.
Assessment
Most cases of athlete’s foot can be treated with over-the-counter (OTC) products. However, cases with complications are likely to require prescription-only treatment (e.g., oral itraconazole or terbinafine, antibiotics) and further investigation. It is therefore important to check the extent and type of infection before recommending a product.
Patients with extensive fungal infection (e.g., if the infection has spread to the toenails or other parts of the body), or signs of a secondary bacterial infection (e.g., painful inflammation and yellow discharge) should be referred to a GP for further assessment and to rule out underlying disease. Patients with diabetes or a compromised immune system, or those with recurrent infections or an infection resistant to treatment, should also be referred.
You inspect John’s feet visually and ask how long he has had the infection, whether any other areas are affected and if he has tried any other treatments. He appears to have a mild athlete’s foot infection which has not spread to the nails. John says the infection has been bothering him for around a week, does not affect any other area, and he has only tried to ease the itch with non-medicated talcum powder. You decide to recommend an OTC antifungal.
What to consider when assessing suspected athlete’s foot
- How extensive is the infection?
- Are there any signs of bacterial infection?
- What are the symptoms and when did they start?
- Has the infection been treated previously? If so, what was used? Was it continued for the recommended time after the infection appeared to clear? Was it applied to a sufficient area?
- Is the infection anywhere else?
- Is this really a case of athlete’s foot?
- Is the condition recurrent?
- Does the patient have diabetes or a compromised immune system?
- How difficult would the patient find a treatment regimen that is frequent and prolonged?
- Does the patient have sensitive skin?
- Is there marked inflammation?
Treatment options
There is a wide range of products available to treat athlete’s foot. These contain a number of active ingredients and are available in various formulations.
According to a 2007 review, topical terbinafine, imidazoles (e.g., miconazole, clotrimazole), tolnaftate and undecenoates are effective for treating athlete’s foot. The review found the most effective topical agent was terbinafine[3]
.
Terbinafine is a synthetic allylamine. It is fungicidal and acts by interfering with fungal sterol biosynthesis, leading to a deficiency in ergosterol and to an intracellular accumulation of squalene, which results in fungal cell death. Topical allylamines may have fewer instances of treatment failure than topical imidazoles; of six systematic reviews, three showed a statistically significant difference favouring allylamines and three showed no significant difference between the two drug classes[4]
.
Terbinafine is not licensed for use in children, is contraindicated in breastfeeding and should only be used by women who are pregnant when potential benefits outweigh the risks.
Imidazoles, tolnaftate and undecenoates are fungistatic. There is insufficient evidence to demonstrate efficacy of any one imidazole over another. One study of 250 patients found ketonazole 2% applied twice a day is as effective as four weeks’ treatment with clotrimazole 1%[5]
. However, another trial comparing clotrimazole applied once a day with ketoconazole applied twice a day did not find a significant difference in efficacy between the topical preparations3.
Although data suggests clotrimazole does not cause adverse effects in pregnancy, it should only be used under medical supervision. It can be used in children. Topical ketoconazole can be used by both pregnant women and children.
Tea tree oil is often claimed to have antiseptic properties. However, a review found there was no conclusive evidence it was effective in the treatment of athlete’s foot3.
Hydrocortisone may be recommended for patients with particularly sore or inflamed skin. It should not be used alone as it will not treat the infection but will dampen the local immune response, resulting in increased fungal growth.
It should be applied once a day. Combination therapies should not be used because hydrocortisone should not be used for more than seven days, and antifungal treatment usually takes longer.
Patient advice
Formulations for the treatment of athlete’s foot include creams, ointments, gels, sprays, paints and powders.
Patients with busy lifestyles, poor manual dexterity or problems reaching their feet may benefit from a treatment that only requires application once a day. Patients with moist, sweaty feet, including those with a sporty lifestyle, may prefer a spray and powder combination, while those
with sensitive skin should be advised to avoid spray treatments, which may contain alcohol and can dry out the skin.
You consider John’s treatment and lifestyle, and decide to recommend terbinafine 1% spray. You advise John to apply the spray to the affected area and also up to 5cm of the surrounding skin. This is because the fungal infection may be present in areas where there are no lesions.
John should continue the treatment after the symptoms have cleared to ensure complete eradication of the infection. The recommended duration of treatment varies between products. Irregular use or stopping treatment prematurely carries a greater risk of recurrence.
John should also be advised to:
- Wash and dry his feet thoroughly before treatment. It may be best to apply the treatment after a bath or a shower to avoid washing off the treatment soon after application;
- If his skin is not cracked or blistered, skin flakes may be removed with a soft brush before treatment, taking care not to cause any breaks in the skin;
- Wash his hands before and after treatment;
- Visit his GP if the infection does not noticeably improve after one week.
Athlete’s foot is contagious, and John should be advised to avoid skin-to-skin contact with others and not to share towels. He should be advised to avoid scratching the skin and to wash his hands after touching the infected area. He should also be advised there is a risk of re-infection from his trainers and he may want to consider a new pair.
Tips on preventing athlete’s foot
- Wash feet regularly and dry them thoroughly
- Keep feet dry and cool: wearing cotton socks (changed regularly) and applying talcum powder may help
- Do not wear tight fitting, occlusive shoes for long periods
- Avoid going bare foot in communal changing rooms and wear flip-flops in shower areas
- Do not wear the same shoes every day
- Some medicated OTC products (e.g., antifungal powders) can be used regularly to help prevent athlete’s foot
- Keep toenails clean and short
References
[1] Crawford F. Athlete’s foot. Clin Ev Online 2009;2009:1712.
[2] Perea S, Ramos MJ, Garau M et al. Prevalence and Risk Factors of Tinea Unguium and Tinea Pedis in the General Population in Spain. J Clin Microbiol. 2000;38: 3226-3230.
[3] Crawford F, Hollis S. Topical treatments for fungal infections of the skin and nails of the foot. Cochrane Datab Sys Rev 2007 DOI:10.1002/14651858.CD001434.pub2.
[4] BMJ Best practice. Evidence and GRADE interventions on athlete’s foot. [Online]. Available from: www.http://bestpractice.bmj.com
[5] Electronic Medicines Compendium. Summary of product characteristics Daktarin Intensiv. [Online]. Available from: http://www.medicines.org.uk [accessed on 10 July 2014].


