
Science Photo Library
This is the second in a series of articles, designed to help pharmacy teams support patients who are experiencing joint pain or patients who have been diagnosed with osteoarthritis and may benefit from recommendations for appropriate management strategies, including the wide range of products available in pharmacies.
More information on joint pain diagnosis and assessment can be found in ‘Pharmacy guide to joint pain: diagnosis and assessment‘.
Read more about our joint pain partnership and find related content on our Pharmacy Learning Centre.
Management options
For patients aged 45 years or over who present to the pharmacy with joint pain and no symptoms that suggest an alternative diagnosis, their mechanical or activity-related joint pain can be managed in community pharmacy[1].
Take note
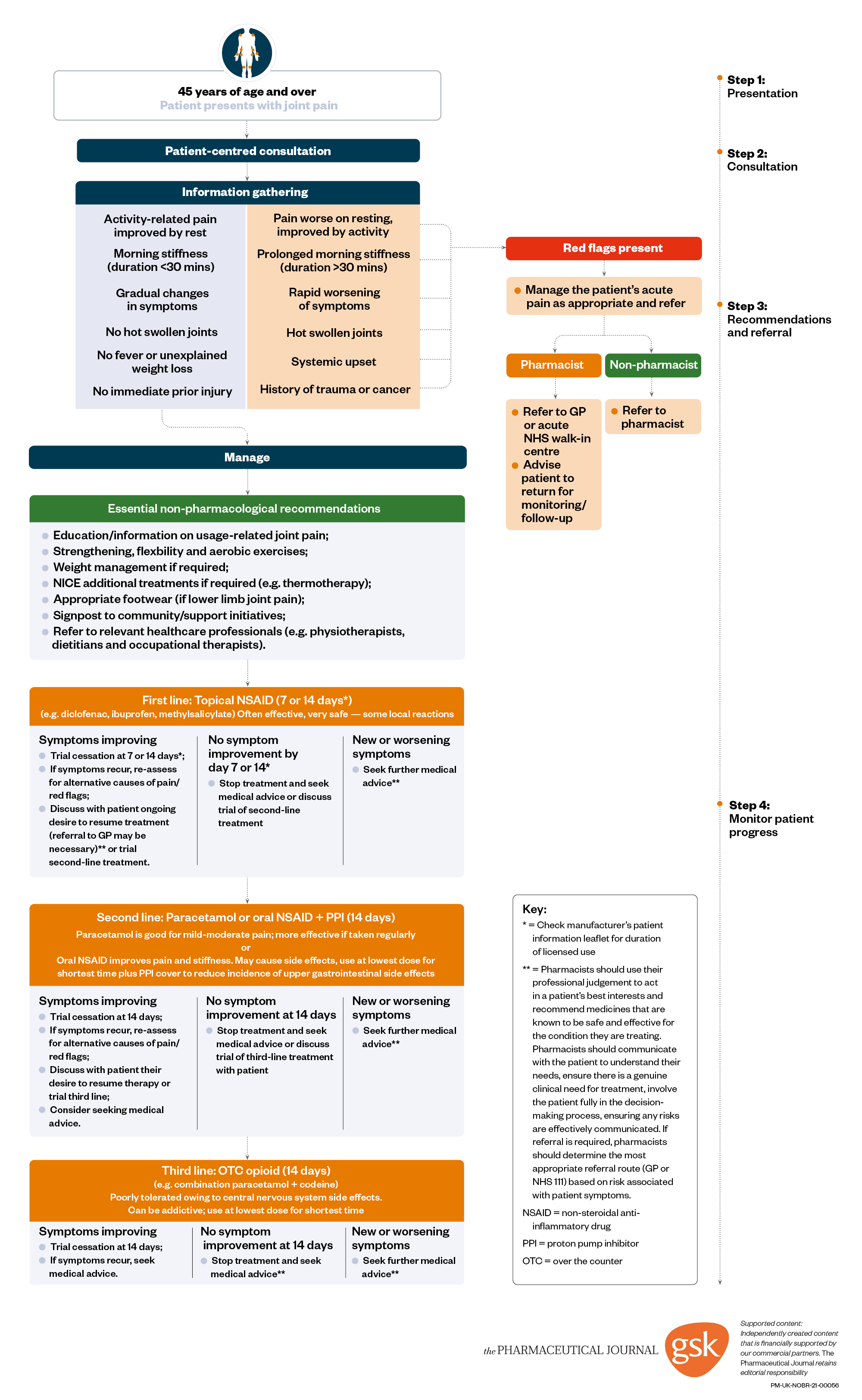
The patient pathway algorithm provides a useful guide on the treatment recommendations for patients after first, second and third presentations. It can be used by pharmacy teams in practice, providing the patient has no contraindications to the recommended treatments and they do not interact with current medicines.
Core treatments
Pharmacy teams should be able to provide information, advice and education to patients, as well as support healthy living by promoting behavioural changes as outlined below. The osteoarthritis (OA) guideline from the National Institute for Health and Care Excellence (NICE) recommends core non-pharmacological treatments that can be provided at the point of care in the pharmacy. These recommendations can be applied to patients of any age[2].
Patient information
- Provide patients with clear and concise verbal/written information.
This can help patients better understand their condition, its possible consequences and the treatment options.
- Consider patient preferences, priorities and past experiences when advising patients on how to manage their condition.
For example, what will help the patient have the best quality of life and carry on with their normal activities?
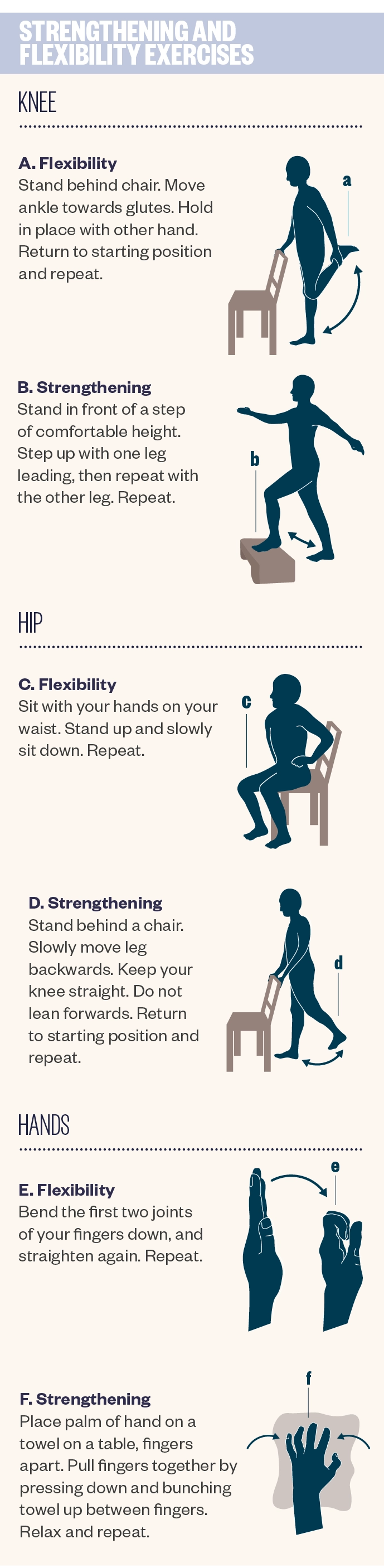
Exercise
Pharmacy teams can provide advice on exercises to improve outcomes and enhance self-management of the condition. Exercising helps to stop the joint capsule from tightening and strengthens the supporting muscles, therefore reducing pain and improving function. By encouraging exercise, patients will also be supported in maintaining a healthy body weight[3].
- Advise patients to maintain, rather than avoid, movement through sensible ‘pacing’ of activities. Encourage patients to carry out both aerobic, stretching and strengthening exercises.
Aerobic exercise can reduce pain and improve function, wellbeing and sleep quality. It is also beneficial for comorbidities that commonly accompany OA. Stretching, strengthening and aerobic exercises should be undertaken regularly. Local strengthening exercises can help to improve pain and function, as well as reverse some of the negative impacts of joint pain[3].
Take note
Not all patients may be able to do the recommended exercises (see ‘Contraindications to exercise‘).
- Encourage patients to incorporate exercise into everyday activities to help build it into their daily routine.
By encouraging patients to find an exercise they enjoy, it may make it easier to incorporate it into their daily routine. For example, walking instead of taking public transport when travelling short distances, or doing some strengthening exercises while waiting for the kettle to boil, may be easy ways to incorporate regular exercise into everyday life[3].
The following exercises should be recommended:
- Undertaking regular exercise may also reduce the need for pain relief medication.
Contraindications to exercise
Not all patients may be able to do the recommended exercises, particularly if they have:
- Acute fever or infection;
- Certain cardiac conditions (e.g. obstructive cardiomyopathy or severe valve disease, myocarditis or arrhythmias [particularly if uncontrolled or induced by exercise]);
- Other unstable conditions (e.g. angina, diabetes or hypertension).
If there is uncertainty about the safety, or the approach, to advising exercise in the presence of another health problem, the patient should be referred to a GP, physiotherapist or specialist for advice[3].
- Signpost patients to local walking groups and provide details of useful information and resources to support them with exercise.
The UK charity Versus Arthritis (previously known as Arthritis Research UK) has produced a booklet entitled ‘Keep moving’, which contains a range of exercises for different joints in the body[4]. It has also produced a leaflet called ‘Protecting your joints’, which provides advice on the best way to approach tasks and movements to protect joints, reduce pain and improve function[5].
Weight management
Weight loss has shown to be beneficial in patients with chronic joint pain and advice should be given on weight management if patients are overweight or obese[3]. Simple tips can be effective in encouraging weight loss, such as recommending:
- Eating a balanced healthy diet (see ‘Food groups in our diet‘);
- Eating breakfast every day;
- Being mindful of calories contained within drinks;
- Eating slowly to enable the body to recognise when it is full;
- Monitoring weight once per week.
Encourage patients to swap sugary fizzy drinks for diet versions with low or no calories, or swap soft drinks for sparkling water with a slice of lemon.
Food groups in our diet
The NHS Eat Well guide explains how to have a healthy, balanced diet. People should try to:
- Eat five servings of fruit and vegetables per day;
- Base meals on starchy foods, such as potatoes, bread, rice or pasta;
- Have some dairy or dairy alternatives, such as soya drinks;
- Eat some beans, pulses, fish, eggs, meat and other protein;
- Choose unsaturated oils and spreads, eaten in small amounts;
- Drink plenty of fluids.
Food and drinks that are high in fat, salt and sugar should be consumed less often and in small amounts.
A variety of different foods should be chosen from the five main food groups[6].
A combination of a healthy diet with an appropriate exercise routine may help people to maintain their weight loss.
Alongside advice on diet and exercise, signposting patients to local pools or parks within the community, or weight-loss groups or initiatives, as well as dietitians, could be helpful in promoting a healthier lifestyle. If patients are having problems managing their weight with diet and exercise, they could be referred to a GP for review to rule out any underlying issues or to discuss medical interventions for weight loss[3].
Footwear
Patients can be given advice on appropriate footwear if their lower limbs are affected by OA. Footwear should have thick but soft soles, no raised heel, broad forefoot and deep soft uppers. Patients can also be referred to a podiatrist for assistance with lower limb joint pain problems[3].
Over-the-counter treatments
Some of the additional treatments recommended by NICE, which have a positive impact on pain and/or function, are available over the counter (OTC) within community pharmacies and include non-pharmacological and pharmacological options. Many people self-manage their pain by buying OTC medicines. Pharmacy teams are ideally placed to question and guide these patients towards the correct treatment options for their condition.
Take note
Before recommending any medication, it is important to be aware of the patient’s current medication (including all prescribed and OTC medicines), other medical conditions (e.g. kidney disease or asthma if considering oral non-steroidal anti-inflammatory drugs [NSAIDs]) and important lifestyle factors (e.g. occupation and driving status if considering opioids) that may affect their individual risk profile to ensure the treatment recommended is appropriate. If in doubt, refer to a pharmacist.
Non-pharmacological treatment options
Supports or braces and use of heat (such as heat packs) or ice (such as ice packs or frozen peas wrapped in a damp towel) may be effective management options for OA symptoms. These measures may help ease pain if used after exercise or if there appears to be any joint swelling[7].
• Reassure patients that they may have to try a few practical solutions before they find what works most effectively for them.
Pharmacological treatment options
OTC pharmacological treatments should be used in combination with supports, braces, heat or ice and are purely for pain relief.
NSAIDs are the first-line pharmacological treatments for most joints (except deep joints, such as shoulders or hips). Topical formulations are applied locally in proximity to the affected area and provide effective concentrations at the local target tissues without producing the systemic levels that are associated with common adverse effects. For mechanical joint pain in the hands or knees, topical NSAIDs may be equally as effective as oral NSAIDs. Topical NSAIDs are safe and cause few side effects — the most common side effects are occasional local skin reactions.
Topical capsaicin can be used as an alternative topical treatment for hand and knee pain. It can take up to one to two weeks before an effect is seen. Capsaicin is very safe but may cause an initial transient burning sensation with use.
Advice on applying topical treatments
It is important to explain to patients that topical joint pain treatments do not take full effect on first application; they can take up to two weeks to provide their maximum effect. Pharmacy teams should ensure that patients are given the following advice:
- The topical treatment should be gently massaged into the skin around the affected joint, using the amount specified on the product information leaflet. The action of massaging can also provide some therapeutic benefit;
- Apply the topical treatment regularly and as specified in the product information leaflet;
- If using capsaicin creams, it is normal to experience a burning sensation on the first application but, with regular application, the analgesic action takes effect after a few days;
- Do not touch sensitive areas (e.g. eyes and genitals) after applying capsaicin;
- If a topical treatment is disliked, an alternative should be tried because each one is different in terms of stickiness and odour;
- Stop using any topical treatment immediately if any side effects (e.g. rash) are experienced and seek advice from a pharmacist[3].
What if topical treatments are ineffective?
Paracetamol, oral NSAIDs or combination codeine + paracetamol (8mg/500mg) may be recommended in this instance. These should only be considered if topical treatments are not appropriate or are ineffective, and if the potential benefit outweighs the risks to the patient[3].
- Advise patients that a gastro-protective agent, such as a proton pump inhibitor (e.g. omeprazole, pantoprazole or rabeprazole) may also need to be taken with oral NSAIDs.
All patients who are taking oral NSAIDs should also be recommended a gastro-protective agent, such as a proton pump inhibitor (e.g. omeprazole, pantoprazole or rabeprazole) to reduce the risk of gastrointestinal bleeding[3].
- Do not recommend glucosamine, rubefacients, acupuncture or herbal remedies because these are not recommended for the treatment of joint pain owing to lack of evidence.
Take note
A rubefacient is a substance for topical application that produces redness of the skin (e.g. by causing dilation of the capillaries and an increase in blood circulation).
However, if a patient wants to use such treatments and it will not cause them any harm, rather than advising against treatments they have faith in, it may be more appropriate to encourage them to add exercises into their daily routine in combination with these methods to help with pain[3].
Take note
Patients who present regularly at the pharmacy with flares of gout to purchase anti-inflammatories, or with joint pain that has not responded to treatment, should be referred to a GP to discuss starting alternative treatments.
Treating more severe cases of joint pain
If topical and oral OTC treatment options are ineffective, referral to a GP is required. Joint surgery should be considered for people with OA who experience joint symptoms that have a substantial impact on their quality of life and have not responded to non-surgical treatment.
The patient journey: the referral pathway
When a patient visits a pharmacy, they may not be visiting to specifically seek help for their joint pain. Regular prescriptions of analgesia may be indicative of chronic joint pain. Asking specific questions about symptoms and conditions can help to appropriately identify mechanical joint pain and rule out any other conditions. Some patients may seek help directly about a previously diagnosed chronic joint pain or consult the pharmacist directly. In either case, it is important not to exclude any red flags and not to assume that the patient has already received evidence-based recommendations. The flowchart (see below) provides a useful overview for community pharmacy teams to support patients with joint pain through their journey in community pharmacy and can help decide the best course of action at each stage.
- Advise patients to use OTC products for the duration specified in the product leaflet.
Products will need to be used daily, rather than just when symptoms occur, to help to maintain relief and prevent symptoms from recurring[3].
- If patients are anxious or frustrated, reassure them that there are other available treatment options that could be tried.
It is important to follow up with patients and encourage them to return after one to two weeks to find out whether their treatment has been effective or whether their symptoms are persistent or have worsened[3].
Figure: Supporting patients with joint pain in community pharmacy
Useful resources
There are many charities and healthcare resources for patients looking for advice and support with joint pain. These can be easily and freely accessed online and include:
- Versus Arthritis (previously known as Arthritis Research UK)
A charity for people with arthritis, formed in 2018 following a merger of Arthritis Care and Arthritis Research UK.
An accessible guidebook written by patients for patients, which includes experiences of patients and solutions for pain and problems related to their joint pain.
A UK charity for people with rheumatoid arthritis.
Interactive tools for assessing weight and links to healthy eating and living advice.
- 1Community pharmacy teams can provide greater support to patients presenting with joint pain, regardless of diagnosis. The Pharmaceutical Journal Published Online First: 2019. doi:10.1211/pj.2019.20205664
- 2Clinical guideline – Osteoarthritis: care and management. National Institute for Health and Care Excellence. https://www.nice.org.uk/guidance/cg177/chapter/1-Recommendations#diagnosis-2 (accessed Feb 2019).
- 3Appropriate community pharmacy management and referral of patients with chronic peripheral joint pain. The Pharmaceutical Journal Published Online First: 2019. doi:10.1211/pj.2019.20205710
- 4‘Keep Moving’ leaflet. Versus Arthritis. https://www.arthritisresearchuk.org/shop/products/publications/patient-information/living-with-arthritis/keep-moving.aspx (accessed Feb 2019).
- 5‘Protecting your joints’ leaflet. Versus Arthritis. https://www.arthritisresearchuk.org/shop/products/publications/patient-information/living-with-arthritis/looking-after-your-joints.aspx (accessed Feb 2019).
- 6NHS Eat Well Guide. NHS. https://www.nhs.uk/live-well/eat-well (accessed Feb 2019).
- 7Osteoarthritis in general practice. Versus Arthritis. http://www.arthritisresearchuk.org/arthritis-information/data-and-statistics/~/media/EFAEFCE432734F3AA5FB1C64329E02D1.ashx (accessed Feb 2019).



