Zephyr / Science Photo Library

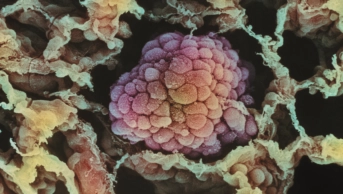
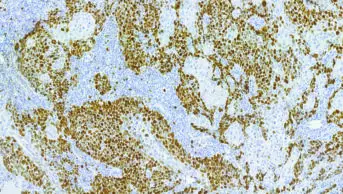
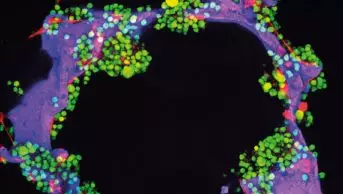
Cancer learning ‘hub’
Pharmacists are playing an increasingly important role in supporting patients with cancer, working within multidisciplinary teams and improving outcomes. However, in a rapidly evolving field with numbers of new cancer medicines is increasing and the potential for adverse effects, it is now more important than ever for pharmacists to have a solid understanding of the principles of cancer biology, its diagnosis and approaches to treatment and prevention. This new collection of cancer content, brought to you in partnership with BeOne Medicines, provides access to educational resources that support professional development for improved patientSurveillance
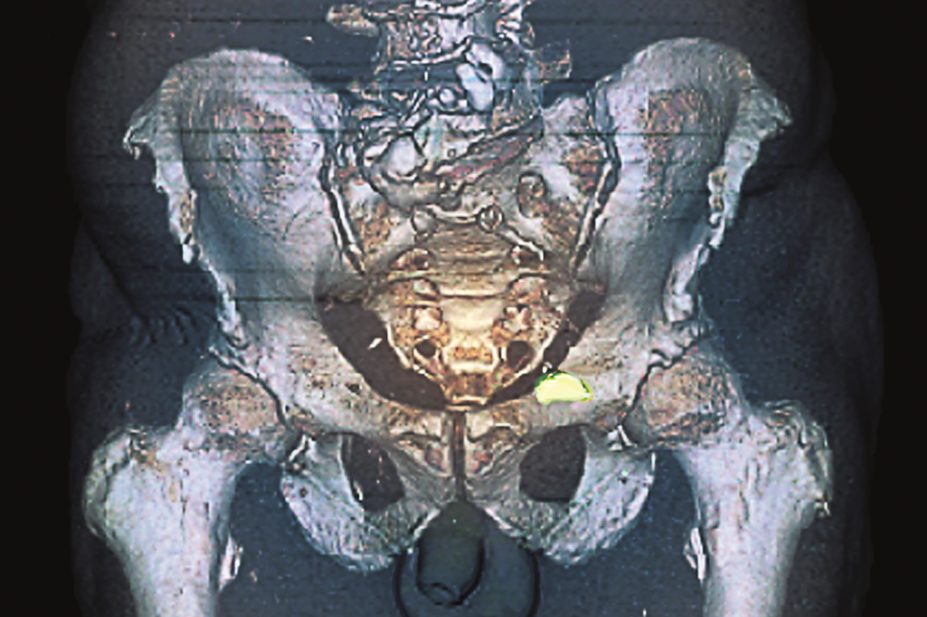
Watchful waiting is sometimes used to monitor the disease with no planned intervention, as it is likely the patient will die from other comorbidities (e.g. cardiovascular disease) before they die of prostate cancer. Active surveillance is used for low-risk patients who have a limited life expectancy (<10–15 years) on account of age at diagnosis or comorbidities. It is an important treatment option as it is more likely that these patients will die of a condition other than prostate cancer. Around 25–30% of these patients will require definitive therapy as their prostate cancer progresses. It is currently unknown whether deferred active therapy results in worse outcomes for men compared with immediate therapy; however, as definitive therapy has associated complications, active surveillance remains a valid choice. The National Institute for Health and Care Excellence (NICE) has produced a protocol for active surveillance (see ‘NICE protocol for active surveillance’)[1] .Radical treatment
NICE recommends radical prostatectomy or radical radiotherapy for men with intermediate-risk localised prostate cancer and men with high-risk localised prostate cancer when there is a realistic prospect of long-term disease control[1] . There is a variety of surgical options, including open surgery or robotic-assisted laparoscopic prostatectomy (RALP) to treat localised prostate cancer. Prostatectomy is associated with complications such as urinary incontinence or sexual dysfunction. Where possible, nerve-sparing radical pr ostatectomy is performed, as it offers a greater chance of sexual recovery. However, patient suitability for this treatment depends on the size and position of the tumour. Radiotherapy can be administered using radical external beam radiotherapy (EBRT) for localised prostate cancer, given as daily fractions over a number of weeks. NICE recommends a minimum dose of 74 Gy to the prostate, at no more than 2 Gy per daily fraction[1] . An alternative to radical radiotherapy is to use high-dose rate brachytherapy in combination with EBRT. Brachytherapy is the implantation of radioactive material directly into the tumour. Two radioactive seed isotopes have been used: iodine (I-125), with a half-life of 60 days, and palladium (Pd-103), with a shorter half-life (17 days) and higher dose rate. The advantage of brachytherapy is that a substantial dose can be delivered to the prostate with minimal effect on the surrounding tissue. One of the main concerns of men undergoing surgery and radiotherapy is the potential loss of sexual function; it is estimated that as many as 50% of patients may not recover erections sufficient for intercourse[1] . In those who do undergo surgery and radiotherapy, the quality (rigidity and duration) of erections is poorer compared with preoperative erections. Potency may return anywhere from two to 24 months following surgery. Sensation of the penis is not changed after nerve sparing radical prostatectomy, and men still experience orgasm. ADT can result in a reduction in libido and loss of sexual function. Early use of phosphodiesterase type-5 inhibitors (e.g. sildenafil, tadalafil) should be offered to patients who are experiencing loss of sexual function; if these fail to restore erectile function, alternatives such as vacuum devices or intracavernosal injections of vasoactive treatments (e.g. papaverine, intraurethral inserts) can be considered[1] .Androgen deprivation therapy
ADT has been the mainstay of advan ced prostate cancer management for many years. Recently, there has been a move towards the use of hormonal treatment in younger men with earlier disease (i.e. non-metastatic) or recurrent disease after definitive treatment (e.g. radiotherapy or surgery) [2] . NICE recommends ADT, together with radiotherapy, as a treatment option for men with intermediate- and high-risk localised prostate cancer[1] . ADT can be used before, during or after radical EBRT, and is often continued for up to three years in patients with high-risk localised prostate cancer[1] . The ‘gold standard’ ADT is bilateral orchiectomy (castration). However, the negative psychological effect of castration has led to a preference for therapies offering reversible testosterone suppression. ADT has been based on luteinising hormone-releasing hormone (LHRH) agonists, which act to reduce testosterone levels by blocking the production and release of gonadotrophins, exerting a negative feedback control on hypothalamic luteinising hormone (LH) secretion and reducing follicle-stimulating hormone (FSH) in the medium- to long-term. If prostate cells are deprived of androgenic stimulation, they undergo apoptosis. LHRH agonists include goserelin[3] , triptorelin[4] and buserelin, with the choice of treatment based on local formulary and cost, rather than any significant differences in clinical effectiveness. Side effects of ADT include hot flushes, weight gain, loss of libido, loss of peripheral hair growth, gynaecomastia, an elevated risk of diabetes, loss of bone mineral density and raised risk of fracture, and an increased risk of cardiovascular complications. Hot flushes can be managed with medroxyprogesterone or cyproterone acetate. Gynaecomastia caused by ADT can be treated with tamoxifen or prophylactic radiotherapy to the breast buds. ADT initially results in an increase in testosterone levels, producing a testosterone surge, prior to down-regulation of testosterone production. This elevation in testosterone levels can result in a ‘tumour flare’ in some patients, who experience a temporary deterioration in their condition. It is common practice to pre-treat patients with anti-androgen therapy prior to starting LHRH therapy and for the first two weeks of LHRH therapy. Anti-androgen therapy reduces the testosterone surge symptoms by blocking the action of testosterone, rather than lowering serum testosterone levels. The most commonly used anti-androgens include nonsteroidal agents (e.g. flutamide, bicalutamide) and steroidal agents (e.g. cyproterone, megestrol). LHRH antagonists (e.g. cetrorelix, ganirelix, degaralix), in contrast to LHRH agonists, bind immediately and competitively to LHRH receptors in the pituitary gland. The effect is a rapid decrease in LH, FSH and testosterone levels without tumour flare. This seemingly more desirable mechanism of action has made LHRH antagonists appear to have an advantage over LHRH agonists, but so far they remain in limited use. Degaralix is currently being reviewed by NICE; draft guidance recommends it as an option only for advanced hormone-dependent prostate cancer patients with spinal metastases who present with signs or symptoms of spinal cord compression (because the tumour flare when starting an LHRH agonist would be dangerous for these patients)[5] . LHRH antagonists are more expensive than LHRH agonists and less cost-effective for all patients; NICE reported it costs £12,306 (excluding VAT) per course of treatment. Clinical trials have compared degarelix with leuprorelin or goserelin with or without bicalutamide, with the primary outcome being prostate-specific antigen (PSA) suppression. These trials were powered for non-inferiority, so improvement in overall survival or tumour reduction was not studied[6] .Treatment of advanced disease
Advanced disease that is initially responsive to androgen blockade can become resistant to blockade with LHRH agonists and antagonists or castration. Previously, this was called ‘hormone refractory’ or ‘androgen independent’ prostate cancer, but is now more accurately known as metastatic castrate resistant prostate cancer (mCRPC). The reason for this change in terminology is a result of greater understanding of the disease, with clinical evidence showing that the androgen receptor axis remains functional, even when patients become ‘hormone refractory’. Historically, patients with metastatic disease showed disease progression to mCRPC within 12–18 months of diagnosis and androgen ablation, despite having castrate levels of serum testosterone (traditionally defined as <50ng/dL), with a median survival of two to three years[6] . Many patients progress while on ADT and experience an increase in PSA without any physical symptoms. Until a few years ago, the only viable treatment option for metastatic disease after failure of ADT was chemotherapy, typically with docetaxel. In recent years, several new effective treatments for metastatic prostate cancer have become available, all of which have been shown to improve overall survival in large-scale, randomised phase III trials. Patients with prostate cancer should be managed by a urology team until they develop mCRPC; at this point they should be referred to an oncology team.Docetaxel
Since its approval by NICE in 2006, docetaxel has been the mainstay of chemotherapy treatment in the UK[7] . The phase III trial that established docetaxel as standard practice was TAX 327, which compared two different schedules of docetaxel and prednisone (weekly and three-weekly) with mitoxantrone and prednisone[8] . The primary endpoint was overall survival, with secondary endpoints including quality of life, PSA changes and pain evaluation. A total of 1,006 patients were recruited and the arms of the trial evenly balanced. A survival advantage was shown with the three-week docetaxel and prednisone schedule versus mitoxantrone and prednisone; 18.9 months medium overall survival versus 16.5 months medium overall survival (P=0.009; hazard ratio (HR) 0.76). No significant survival advantage over mitoxantrone and prednisone was seen in patients receiving the weekly dosing schedule; however, the trial demonstrated a significant improvement in pain response and improved quality of life scores. Docetaxel is associated with a high rate of neutropenia in practice; however, in the TAX 327 trial, only 3% of patients had febrile neutropenia. This might have been because the trial protocol allowed treatment with granulocyte colony-stimulating factor for neutropenia patients, which is not common practice in the UK[8] . To date, three trials have examined the use of docetaxel chemotherapy at earlier stages of prostate cancer, either for high-risk, localised disease or metastatic hormone sensitive prostate cancer (mHSPC). The GETUG-AFU 15 trial was a randomised, open-label, phase III trial that enrolled 385 patients with newly diagnosed mHSPC[9] . Patients received ADT alone (orchiectomy or LHRH agonists) or ADT with docetaxel 75mg/m2 every 21 days for nine cycles. The trial did not demonstrate a statistically significant overall survival benefıt by adding docetaxel to ADT; 58.9 months for the docetaxel arm versus 54.2 months for the ADT arm (P=0.95; HR 1.01). The trial had a relatively small sample size and included a substantial percentage of patients with good prognostic factors. High levels of toxicity were reported, with more than a 10% incidence of grade 3 neutropenia and four deaths in the ADT plus docetaxel arm; 21% of men who received docetaxel plus ADT discontinued treatment because of toxicity[9] . CHAARTED, a larger phase III American clinical trial conducted in 790 patients with hormone-naive mHSPC, compared ADT alone to ADT plus docetaxel chemotherapy at 75mg/m 2 every three weeks, for a maximum of six cycles[10] . Patients were stratifıed as having high-volume or low-volume metastatic disease. The primary endpoint was overall survival, and the trial showed a median overall survival of 57.6 months for the early docetaxel arm, compared with 44 months for ADT alone (P=0.0003; HR 0.61). In the subset of patients with high-volume disease, a 17-month improvement in overall survival was observed in the ADT plus docetaxel arm[10] . The UK-led STAMPEDE trial is a complex multi-centre, randomised controlled trial for patients with locally advanced or metastatic prostate cancer who are about to commence ADT[11] . The trial randomises patients to receive a variety of medicines in combination with ADT, including zoledronic acid, docetaxel, celecoxib, abiraterone and enzalutamide. In June 2005, the first results of four of the trial’s arms were presented, with data from 2,962 men randomised at a 2:1:1:1 ratio to receive ADT; ADT plus six cycles given e very three weeks of docetaxel; ADT with zoledronic acid; or ADT with docetaxel and zoledronic acid[11] . In total, 61% of participants had metastatic disease and 39% had locally advanced, non-metastatic prostate cancer. Patients assigned to the docetaxel arm had a significantly improved median overall survival of 77 months compared with 67 months for patients in the ADT-only arm (P=0.003; HR 0.76). The subset of patients with metastatic disease had an even better 22-month improvement in overall survival, compared with ADT alone (65 months versus 43 months, P=0.002; HR 0.73). The trial is ongoing.Cabazitaxel
After standard docetaxel, cabazitaxel has been used as second-line chemotherapy for mCRPC. In the UK, cabazitaxel has been rejected by NICE and the Scottish Medicines Consortium (SMC) because they do not consider it to be cost-effective, but it has been made available for patients in England through the Cancer Drugs Fund (CDF). The TROPIC phase III study randomised a total of 755 patients with mCRPC, previously treated with a docetaxel-containing regimen to receive cabazitaxel 25mg/m2 plus prednisone every three weeks versus mitoxantrone 12mg/m2 plus prednisone every three weeks[12] . The primary end point was overall survival, which increased with cabazitaxel treatment (15.1 months versus 12.7 months, respectively, a difference of 2.4 months [P<0.0001; HR 0.70]). The secondary end point of progression-free survival (PFS) was also significantly prolonged with cabazitaxel (2.8 months versus 1.4 months, respectively). However, patients in the cabazitaxel arm experienced greater toxic effects, including diarrhoea , vomiting, neutropenia and febrile neutropenia[12] .Abiraterone and enzalutamide
For the treatment of adult men with mCRPC whose disease has progressed during, or after, docetaxel therapy, abiraterone and enzalutamide are approved by NICE[13],[14] . Abiraterone acetate is an androgen biosynthesis inhibitor that blocks biosynthesis of extragonadal androgens. Abiraterone leads to a rebound increase in LH and in adrenocorticotropic hormone (ACTH), and so it is given with low-dose corticosteroids to normalise mineralocorticoid levels and reduce side effects. Abiraterone is taken as a 1g oral dose, in combination with prednisolone 5mg twice daily, on a 28-day cycle. It is available in 250mg tablets, which must not be taken with food. Patients should be advised that taking the dose at night can often minimise the lethargy that is a potential side effect. If toxicity occurs, treatment should be suspended and restarted with the advice of the treating oncologist; there is no evidence to support reducing the dose. The most commonly observed side effects are hypokalaemia, hypertension, lower limb oedema, diarrhoea and lethargy[15] . Enzalutamide acts on three steps in the androgen receptor signalling pathway; as an androgen receptor antagonist (no agonist activity); by inhibiting translocation of the androgen-receptor complex to the cell nucleus; and by inhibiting receptor binding to DNA in the nucleus and therefore preventing cell replication and instigating apoptosis. Enzalutamide is taken as a 160mg oral dose once daily, on a 28-day cycle. It is available as 40mg capsules, which should be swallowed whole with water and can be taken with or without food. If a patient experiences serious toxicity or an intolerable adverse reaction, they will require interruption of abiraterone therapy and dosing should be withheld for one week, or until symptoms improve, then resumed at the same or a reduced dose (120mg or 80mg) if warranted. The most common side effects are hypertension, hot flushes and headache. Although they have slightly different mechanisms of action, clinically both treatments are considered interchangeable, with evidence of clinical benefits similar between the two[13],[14] . Clinicians can use one or the other, but not both. Currently there are no published phase III trials of either drug where patients had previously received the other treatment. There is also emerging evidence of cross resistance among abiraterone, enzalutamide and taxane chemotherapy, although the implications for the order of treatment are not yet known[16] . The COU-AA-301 phase III trial for abiraterone post-chemotherapy examined 1,195 patients who had previously received docetaxel and randomised them to receive 5mg of prednisone twice daily, with either 1g of abiraterone (797 patients) or placebo (398 patients)[17] . The primary end point was overall survival, which was longer in the abiraterone plus prednisone group than in the placebo plus prednisone group, at 14.8 months versus 10.9 months, respectively (P<0.001; HR 0.65). All secondary end points, including time to PSA progression (10.2 months versus 6.6 months; P<0.001) and PFS (5.6 months versus 3.6 months P<0.001), favoured the treatment group. However, the side effect profile was worse in the abiraterone prednisone group, with more mineralocorticoid-related adverse events, including fluid retention, hypertension and hypokalaemia[17] . The AFFIRM phase III trial of enzalutamide post-docetaxel randomised 1,199 patients to receive either enzalutamide (at a dose of 160 mg) or placebo once daily at a 2:1 ratio and patients were allowed, but not required, to take up to 10mg prednisone a day[18] . Enzalutamide demonstrated a 4.8 month improvement in the primary outcome of overall survival compared with placebo, at 18.4 months versus 13.6 months, respectively (P<0.001; HR 0.631). The benefit of enzalutamide was demonstrated by the secondary end points, including the time until the initiation of cytotoxic chemotherapy, the time until the first skeletal-related event and the time until PSA progression. Fatigue and hypertension were the most common clinically relevant adverse events associated with enzalutamide treatment[18] . Both abiraterone and enzalutamide can interact with other drugs. Abiraterone may increase exposure of other medicines metabolised by cytochrome P450 (CYP) 2D6, which include metoprolol, propranolol, desipramine, venlafaxine, haloperidol, risperidone, propafenone, flecainide, codeine, oxycodone and tramadol. Enzalutamide is a strong CYP3A4 enzyme inducer. Interactions with medicines that are eliminated via CYP3A4 metabolism are expected, including fentanyl, clarithromycin, cabazitaxel, warfarin, anti-epileptics and calcium channel blockers. The clinical significance of these interactions is unknown.- If the drugs are being used for indications included in the Cancer Drugs Fund (CDF), there should be a clear understanding of whom is responsible for registering the patient on the CDF. This should ideally be the consultant initiating therapy.
- Patients should be seen initially by a consultant uro-oncologist (to be prescribed abiraterone or enzalutamide) and then referred to the pharmacist for monitoring. The consultant must have ensured a baseline assessment of cardiac function has been considered and there should be an agreed interval (e.g. every three-months) when the patient is reviewed by a consultant.
- There may be a requirement for more frequent review (e.g. every two weeks in the first three months), as it is common to see the disease flare initially, when bone pain worsens and PSA rises. The consultant may see the patient more frequently at first, until the patient is tolerating medication well and can then move to four-weekly review with a pharmacist.
- The pharmacist should see the patient monthly and only issue one month’s medication at a time. A medication history should be taken, in addition to checking for potential interactions.
- Pharmacists will need to make arrangements for blood to be taken on each visit, so the pharmacist can monitor the patient’s blood counts (e.g. urea and electrolytes, liver function tests and full blood count). PSA should also be requested from the patient’s blood sample.
- Response and progression is monitored using PSA and patient symptoms and if there is a rise in PSA and/or symptoms of progression, the pharmacist should refer the patient back to the consultant. The protocol for monitoring can vary with the experience of the pharmacist, however, it is suggested that if there are three consecutive rises in PSA, or deterioration in a patient’s well-being and performance status, or progression of disease-related symptoms, such as bone pain, poor appetite or increasing frequency of micturition, a consultant review is required to assess disease progression. Currently there are no commonly used radiological indicators to assess response.
Sipuleucel-T and ipilimumab
The autologous cellular immunotherapy vaccine Sipuleucel-T stimulates the patient’s own immune cells to identify and attack prostate cancer cells. It is generated from a patient’s own peripheral immune cells, obtained via leukopheresis, which are then exposed to a fusion peptide of granulocyte macrophage colony stimulating factor (serving as immune adjuvant) and pulmonary alveolar proteinosis [21] . The IMPACT trial was a randomised placebo-controlled trial of 512 asymptomatic or minimally symptomatic men with mCRPC, and provides the main evidence for Sipuleucel-T[21] . The trial demonstrated a 4.1-month improvement in median overall survival in the Sipuleucel-T arm compared with the placebo arm (25.8 months versus 21.7 months; P=0.03, HR 0.78). No difference in time to progression or PSA response was reported, which may be a reflection of the late onset of benefit of immune therapy. Sipuleucel-T is not recommended by NICE on cost-effectiveness grounds[22] . Ipilimumab is an immune checkpoint inhibitor used for the treatment of metastatic melanoma. Its use in prostate cancer was evaluated in a phase III study in patients previously treated with chemotherapy[23] . Patients received a single dose of radiation followed by either ipilimumab 10mg/kg or placebo, every three weeks, for up to four doses. The study did not meet its primary end point of improved overall survival, so ipilimumab remains investigational and is not used. However, there is renewed interest in immune therapy in oncology, so further trials are expected.Bone metastases
One important part of the treatment of metastatic prostate cancer involves the prevention and treatment of the complications of bone metastases. Patients are at substantial risk of skeletal complications from bone metastases, often referred to as skeletal-related events (SREs), and include fracture, skeletal instability or loss of skeletal integrity, spinal cord compression, the need for surgery or radiation therapy for a symptomatic bone metastasis and hypercalcaemia. NICE recommends that bisphosphonates should not be used for prevention, but only for pain relief for men with mCRPC when other treatments (including analgesics and palliative radiotherapy) have failed[1] . NICE also recommends the use of strontium-89 as a treatment option for men with painful bone metastases. Denosumab is licensed for preventing SREs and has shown superiority to bisphosphonates[24] ; however, it is not recommended by NICE for men with bone metastases from prostate cancer. Radium-223 is a radioactive isotope that emits low levels of alpha particle radiation, which causes double-strand breaks in DNA, killing cells. It acts as a ‘calcium mimetic’ that, like calcium, accumulates preferentially in areas of bone that are undergoing increased turnover, and therefore acts against bone metastases. The ALSYMPCA trial targeted men with symptomatic bone metastases in the absence of visceral disease[25] . Radium-223 was administered at a dose of 50 kBq/kg once every four weeks, for six cycles. Radium-223 improved overall survival by 3.6 months: 14.9 months for Radium-223 versus 11.3 months for placebo (P=0.001; HR 0.7). Patients receiving radium-223 also reported a better quality of life than patients in the placebo group[25] .References
[1] The National Institut e for Health and Care Excellence (NICE) Guidelines [CG175]. Prostate cancer: diagnosis and treatment. Available at: https://www.nice.org.uk/guidance/cg175/resources/guidance-prostate-cancer-diagnosis-and-treatment-pdf (accessed June 2015).
[2] European Association of Urologists (EAU) Prostate Cancer Guidelines 2012. Available at: www.uroweb.org (accessed June 2015).
[3] Vogelzang NJ, Chodak GW, Soloway MS et al; Zoladex Prostate Study Group. Goserelin versus orchiectomy in the treatment of advanced prostate cancer: final results of a randomized trial. Urology 1995;46:220–226.
[4] Crawford ED, Eisenberger MA, McLeod DG et al. A controlled trial of leuprolide with and without flutamide in prostatic carcinoma. N Engl J Med 1989;321:419–424.
[5] The National Institute for Health and Care Excellence (NICE). Guidelines in development [GID-TAG352]. Prostate cancer (advanced, hormone dependent) — degarelix depot. Available at: https://www.nice.org.uk/guidance/indevelopment/gid-tag352/documents (accessed June 2015).
[6] Chang S. Treatment options for hormone-refractory prostate cancer. Rev Urol 2007;9(Suppl 2):S13–S18.
[7] The National Institute for Health and Care Excellence (NICE). Technology Appraisal Guidance [TA101]. Docetaxel for the treatment of hormone-refractory metastatic prostate cancer 2006.
[8] Tannock IF, de Wit R, Berry WR et al. Docetaxel plus Prednisone or Mitoxantrone plus Prednisone for Advanced Prostate Cancer. N Engl J Med 2004;351:1502–1512.
[9] Gravis G, Fizazi K, Joly F et al. Androgen-deprivation therapy alone or with docetaxel in non-castrate metastatic prostate cancer (GETUG-AFU 15): a randomised, open-label, phase 3 trial. Lancet Oncol 2013;14:149–158.
[10] Sweeney C, Chen Y, Carducci M A et al . Impact of overall survival (OS) with chemohormonal therapy versus hormonal therapy for hormone-sensitive newly metastatic prostate cancer (mPrCa): An ECOG-led phase III randomized trial. J Clin Oncol 2014;32;3s(suppl; abstr LBA2).
[11] James DN, Sydes MR, Mason MD et al . Docetaxel and/or zoledro nic acid for hormone-naïve prostate cancer: First overall survival results from STAMPEDE (NCT00268476). J Clin Oncol 2015:33;(suppl; abstr 5001).
[12] de Bono JS, Oudard S, Ozguroglu M et al . Prednisone plus Cabazitaxel or mitoxantrone for metastatic castration-resistant prostate cancer progressing after docetaxel treatment: a randomised open-label trial. The Lancet 2010;376:1147–1154.
[13] The National Institute for Health and Care Excellence (NICE). Technology appraisal guidance [TA259]. Abiraterone for castration-resistant metastatic prostate cancer previously treated with a docetaxel-containing regimen 2012.
[14] The National Institute for Health and Care Excellence (NICE). Techno logy appraisal guidance [TA316]. Enzalutamide for metastatic hormone‑relapsed prostate cancer previously treated with a docetaxel‑containin g regimen 2014.
[15] European Medicines Agency. SPC for abiterone. Available at: http://www.ema.europa.eu/docs/en_GB/document_library/EPAR_-_Product_Information/human/002321/WC500112858.pdf (accessed June 2015).
[16] Van Soest RJ, van Royen ME, de Morre´e ES et al . Cr oss-resistance between taxanes and new hormonal agents abiraterone and enzalutamide may affect drug sequence choices in metastati c castrationresistant prostate cancer. Eur J Cancer 2013;49:3821–3830.
[17] De Bono JS, Logothetis CJ, Molina A et al. Abiraterone and increased survival in metastatic prostate cancer. N Engl J Med 2011;364:1995– 2005.
[18] Scher HI, Fizazi K, S aad F et al . Increased survival with enzalutamide in prostate cancer after chemotherapy. N Engl J Med 2012;367:1187–1197.
[19] Ryan CJ, Smith MR, Fizazi K et al. Abiraterone acetate plus prednisone versus placebo plus prednisone in chemotherapy-naive men with metastatic castration-resistant prostate cancer (COU-AA-302): final overall survival analysis of a randomised, double-blind, placebo-controlled phase 3 study. Lancet Oncol 2015 ;16(2):152–160.
[20] Tomasz M, Beer MD, Armstrong AJ et al; for the PREVAIL Investigators. Enzalutamide in metastatic prostate cancer before chemotherapy. N Engl J Med 2014;371:424–433.
[21] Kantoff PW, Higano CS, Shore ND et al. Sipuleucel-T immunotherapy for castration-resistant prostate cancer. N Engl J Med 2010;363:411–422.
[22] The National Institute for Health and Care Excellence (NICE). Technology appraisal guidance [TA332]. Sipuleucel-T for treating asymptomatic or minimally symptomatic metastatic h ormone-relapsed prostate cancer 2015.
[23] Kwon ED, D rake CG, Scher HI et al. Ipilimumab versus placebo after radiotherapy in patients with metastatic castration-resistant prostate cancer that had progressed after docetaxel chemotherapy (CA184-043): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol 2014;15:700–712.
[24] Fizazi K, Carducci M, Smith M et al. Denos umab versus zoledronic acid for treatment of bone metastases in men with castration-resistant prostate cancer: a randomised, double-blind stu dy. The Lancet 2011;377:813–822.
[25] Parker C, Nilsson S, Heinrich D et al. Alpha-emitter radium-223 and increased survival in metastatic prostate cancer. N Engl J Med 2013;36 9:213 –223.