Shutterstock.com
Revalidation officially began on 30 March 2018, replacing the old continuing professional development (CPD) process[1]
. Pharmacists and pharmacy technicians entering their second year of revalidation now need to submit one peer discussion and one reflective account, as well as four CPD entries covering planned and unplanned learning.
The Academy of Medical Royal Colleges defines reflective practice as “the process whereby an individual thinks analytically about anything relating to their professional practice with the intention of gaining insight and using the lessons learned to maintain good practice or make improvements where possible”[2]
.
In practical terms, a reflective account should be a brief, written description of an experience and your actions, including what went well and what did not go well, and what you have learnt for the future. It should be a formalisation of what is already being done subconsciously as a pharmacy professional and should describe how service users have benefited as a result[3]
. Service users are varied and will depend on your role; they may include patients, commissioners, staff and other healthcare professionals. Academic pharmacists may describe the impact that their services have had on students, while pharmacists who work in industry might explain their impact on colleagues developing or manufacturing medicines.
What should be reflected on?
The General Pharmaceutical Council (GPhC) decides which of the nine standards should to be reflected on each year[4]
(see Box 1). If you are completing your reflective account for the first time, the standards you should reflect on are numbers 3, 6 and 9[5]
.
Box 1: The General Pharmaceutical Council’s standards
Professionalism and safe and effective practice are central to the role that pharmacy professionals have in delivering and improving the health, safety and wellbeing of patients and the public. The nine standards outline what it means to be a pharmacy professional:
- Standard 1: Provide person-centred care;
- Standard 2: Work in partnership with others;
- Standard 3: Communicate effectively;
- Standard 4: Maintain, develop and use their professional knowledge and skills;
- Standard 5: Use professional judgement;
- Standard 6: Behave in a professional manner;
- Standard 7: Respect and maintain the person’s confidentiality and privacy;
- Standard 8: Speak up when they have concerns or when things go wrong;
- Standard 9: Demonstrate leadership.
Source: General Pharmaceutical Council[4]
The GPhC says it chose these standards because it thinks it is important to assure members of the public that their trust in pharmacists and pharmacy technicians is well placed; the standards relate well to one another (one standard must be reflected on, but it may be easy to produce one reflective account to cover all three standards); and standard 3 was used in the pilot study[3]
, so evaluating reflective accounts based on this standard will help the GPhC assess how revalidation is working.
Communicating effectively with others (standard 3) could include information about how you have overcome barriers to communication, demonstrated active listening, or adapted your communication style to meet the needs of the person you are communicating with[4]
.
Behaving in a professional manner (standard 6) could include examples of when you have shown empathy and compassion, a time that you have acted with honesty and integrity, or an example of treating people with respect and safeguarding their dignity[4]
.
Demonstrating leadership (standard 9) could include examples of when you have led by example, or contributed to the education and training of others[4]
. See Box 2 for relevant resources from The Pharmaceutical Journal.
Box 2: Relevant resources from The Pharmaceutical Journal
To help support Royal Pharmaceutical Society members and subscribers to The Pharmaceutical Journal and Clinical Pharmacist complete their reflective account, a special page on pharmaceutical-journal.com has been developed and will be available from the end of May 2019. These relevant learning and careers articles can be used to support the development of your reflective account entries, while also providing ideas for the scope of activity that could be included.
Communicate effectively (Standard 3)
- How pharmacists can encourage patient adherence to medicines;
- Discussing the MMR vaccine with patients.
Behave in a professional manner (Standard 6)
- How to spot signs of child sexual exploitation;
- Communicating with palliative care patients nearing the end of life, their families and carers.
Demonstrating leadership (Standard 9)
How much detail should be included?
The reflective account needs to be a brief example (or examples) of something that happened in the previous year, specifically thinking about why you did what you did.
First, outline your area of practice in two or three short sentences, including details of where you work and what your main roles are. For example:
- I am a pharmacy technician working in a hospital setting. My main role involves dispensing medicines for inpatients and outpatients, plus checking dispensed medicines
[5]
. - I am a pharmacist working in a clinical commissioning group (CCG), which oversees the implementation of local prescribing formularies in line with my sustainability and transformation plan footprint. I am also the education and training lead for our CCG, which means I champion the development of our ten pharmacists
[6]
.
Then, describe the typical users of the service you provide in another two to three short sentences. If you do not have direct patient access, then you can describe how your services indirectly impact on patient care. For example:
- The users of my services include patients, pharmacy staff and other hospital staff
[5]
. - Typical users of my service include prescribing leads, commissioners and GPs. This has an indirect effect on patient care because the information I provide is used by them to improve the standard of care provided
[5]
.
You then need to explain how you are meeting one or more of the three standards for pharmacy professionals (see Box 1). Set the scene by explaining the situation; if you are struggling with where to start, use ‘free writing’ as a technique to collect your thoughts.
To begin, spend ten minutes writing down thoughts that come into your head relating to the standard or element of professional practice you want to reflect on. Then re-draft and edit it to add depth.
Ensure that the examples used are relevant. There are many different situations and experiences you could potentially reflect on, but try not to focus on a particular number or type of reflective notes. Instead, it would be most valuable to reflect on experiences that relate to your professional practice and offer the potential for you to develop, learn lessons and gain insight.
Before you begin to write the rest of your reflective account, it is important to remember to keep your reflections anonymous. Although real-life examples are required by the GPhC, it is important to remember that patient confidentiality must still be maintained. Therefore, be careful to anonymise anything that could be used to identify a patient (e.g. the patient’s name, the time and date of the event, the location where the event occurred). Similarly, precise locations, dates and times should not be specified. Separating the timing of the reflective documentation of an event and its actual occurrence may help to achieve this[2]
.
How can learning be demonstrated?
Focus on the learning resulting from an event, rather than a full discussion of a case or situation[2]
. Start with the aims of what you were doing. For example:
- To learn why we saw an increase in the number of medicine errors in March
[5]
. - To improve electronic communication with a nursing home manager and a GP
[5]
.
Describe your role and the skills you used. Focus on what went well, what you are most proud of and how people benefited from using your service. Then, look at anything that did not go well. Try to keep your response free of emotion and state what could be done to avoid or improve similar situations in the future. It does not have to focus on criticism — it can be positive. For example:
- The results made me realise that we do not engage students in any of the decision-making processes and only request their feedback for teaching sessions and other activities retrospectively. I decided to review how we communicated and engaged with our students
[5]
. - I produced a revised prescription-handling protocol to standardise the recording process within the medicine centre
[5]
. - After speaking to customers during the day and afterwards,
it was clear to me that this method was highly effective, not only in health promotion, but also in their views on us as a pharmacy. It also directly benefited some customers with referrals to the GP about their issues that otherwise may have been left for longer
[5]
.
Now you have thought about the situation in greater detail, think about why things happened as they did. How did you and others interact at the time? Is there anything you could do differently next time? If so, what would you do and why?
Think about what factors you could have influenced: is there anything you could have tried that may have improved the situation, or is there anything you did that was particularly important in the situation? It is easy to remember the things that you did not do and it is often the things that you did well that are forgotten. For example:
- I could have been more proactive in my approach with my team and identified clear learning opportunities with them at the start of the year. Rather than just sending an email to the team with some suggested courses, I could have met with them individually and understood their training needs in greater detail, so I could have tailored my suggestions for additional training to best suit them
[5]
.
You need to pull everything you have outlined together before you can learn, change your own practice and improve. It might be useful to look beyond what you would do differently, and instead think whether you have identified any transferable knowledge or skills you can utilise elsewhere[7]
. Think about how you have changed or improved your practice as a result of that experience and anything you can share with your peers. For example:
- Because I changed the way I communicated with the GP, we built a rapport prior to the visit to the nursing home. I continued to use my improved communication skills to lead a successful clinical ward round
[5]
. - Following implementation of this process, two clinical colleagues and I wrote a ‘white paper’ describing the process and challenges that we encountered
[5]
.
You may find it useful to test your reflections. For example, when comparable situations happen again, do things change as you would expect them to? This is a chance to repeat the reflective cycle to refine and develop your understanding[7]
.
Can this process be made easier?
The following tips may help you improve your reflection in preparation for writing your account:
1. Make reflection a habit
Reflecting on your activity soon after the event will make your recollection more truthful. Writing notes may be time consuming, so recording reflections on your phone that could be transcribed later could be useful.
2. Recognise the benefits
Reflection on both good and bad experiences is vital to wellbeing and development, as well as improving the quality of care for patients.
3. Think about times when you avoid reflection
If you are not able to write down your feelings or you struggle to describe your experiences, you could record reflections, or talk to someone, perhaps even seek their permission to record the conversation. Drawing word clouds or illustrations may also help.
4. Avoid leaving it to the last minute
Plan your learning and CPD across the year, regularly reviewing your learning opportunities, and perhaps tie this in with your annual appraisal. This could provide a useful opportunity to get feedback[8]
.
There are many resources that you can access to help you to record learning as you go along. The Royal Pharmaceutical Society (RPS) MyCPD app has a facility to help recording ongoing learning (see Box 3). The app is available for iOS devices via the App Store and Android devices via Google Play.
The RPS is also providing members with a dedicated Revalidation Support Service, who can be contacted by phone or email (0333 733 2570; support@rpharms.com), and a dedicated revalidation support hub, which also provides more information on the various support services offered, is available on the RPS website.
The GPhC also has a number of resources to help pharmacy professionals. If you are unable to complete your revalidation submission owing to exceptional circumstances (e.g. maternity or sick leave), let the GPhC know as soon as possible as they might be able to extend your deadline, allow you to submit fewer records or, in some cases, skip the process for a year.
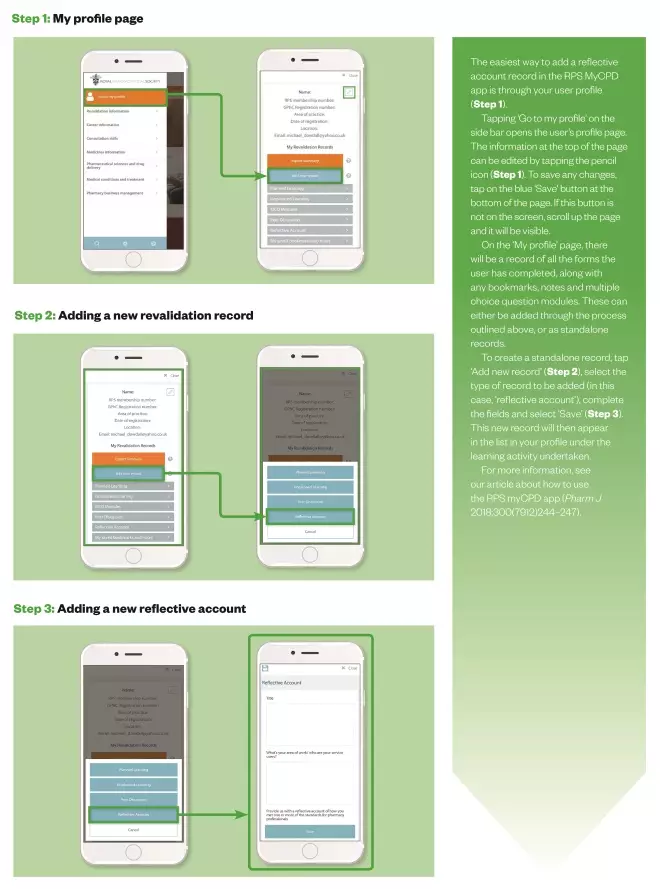
Photoguide: How to record a reflective account in the RPS MyCPD app
Source: JL / The Pharmaceutical Journal
For more information, see our article about how to use the RPS myCPD app
For information on how to complete your peer discussion, read the accompanying learning article here.
References
[1] Torjesen I. Revalidation: support and implementation. Pharm J 2018;300(7909) doi: 10.1211/PJ.2018.20204267
[2] The Academy of Medical Royal Colleges and the Conference of Postgraduate Medical Deans of the United Kingdom. Academy and COPMeD Reflective Practice Toolkit. 2018. Available at: http://www.aomrc.org.uk/wp-content/uploads/2018/08/Reflective_Practice_Toolkit_AoMRC_CoPMED_0818.pdf (accessed May 2019)
[3] General Pharmaceutical Council. Revalidation: find out which standards you will need to reflect on. 2018. Available at: https://www.pharmacyregulation.org/regulate/article/revalidation-find-out-which-standards-you-will-need-reflect (accessed May 2019)
[4] General Pharmaceutical Council. Standards for pharmacy professionals. 2017. Available at: https://www.pharmacyregulation.org/sites/default/files/standards_for_pharmacy_professionals_may_2017_0.pdf (accessed May 2019)
[5] General Pharmaceutical Council. Revalidation resources for pharmacy professionals. Available at: https://www.pharmacyregulation.org/revalidation-resources-pharmacy-professionals (accessed May 2019)
[6] Royal Pharmaceutical Society. Example revalidation records. 2018. Available at: https://www.rpharms.com/professional-development/revalidation/example-revalidation-cpd-records (accessed May 2019)
[7] Koshy K, Limb C, Gundogan B et al. Reflective practice in health care and how to reflect effectively. IJS Oncol 2017;2(6):e20. doi: 10.1097/IJ9.0000000000000020
[8] Royal College of Nursing. Eight ways to improve your reflection. 2015. Available at: https://www.rcn.org.uk/professional-development/revalidation/eight-ways-to-improve-your-reflection (accessed May 2019)