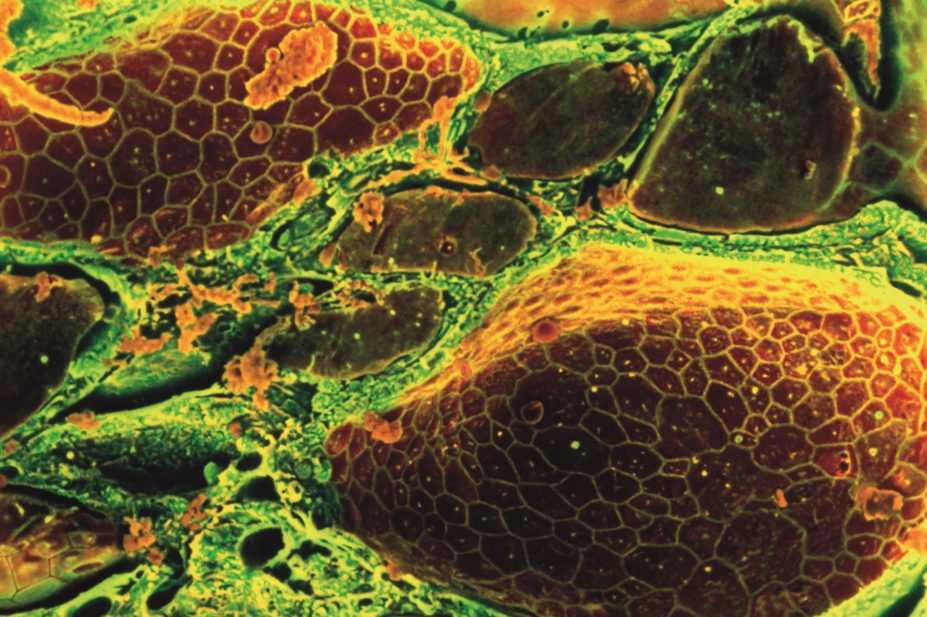
Steve Gschmeissner / Science Photo Library
In this article you will learn:
- How thyroid dysfunction can affect drug metabolism
- Common drug interactions with levothyroxine and liothyronine
- Dose adjustments required in patients with changing thyroid status
The thyroid is a gland located in the front of the neck, it produces the hormone tri-iodothyronine (T3) and the pre-hormone thyroxine (T4), which is subsequently converted in the periphery to the active hormone T3. The thyroid hormones stimulate diverse metabolic activities throughout the body, leading to regulation of the basal metabolic rate.
Iodide absorbed from the diet is an essential element for thyroid hormone production. The iodide ion is transported into the hormone-producing follicular cells, where it is oxidised by the enzyme thyroperoxidase and added to the protein thyroglobulin as part of thyroid hormone synthesis.
A negative feedback loop regulates the levels of thyroid hormones. When circulating T3 and T4 levels drop too low, the hypothalamus increases release of thyrotropin-releasing hormone (TRH), which acts on the anterior pituitary gland to stimulate the release of thyroid stimulating hormone (TSH), causing the thyroid gland to release more T4 and T3. Disruption to this mechanism results in hypothyroidism or hyperthyroidism.
TSH and free T4 levels are used initially to assess if patients have thyroid dysfunction. A TSH value within its standard reference range (0.4–4.5mU/L) excludes most cases of thyroid dysfunction. The normal reference range for free T4 is 9–25pmol/L.
Strategies for managing thyroid disorders aim to alleviate symptoms and restore normal thyroid hormone levels. Thyroid hormones are essential for metabolism, and disordered thyroid function can alter the metabolism of some medications. It is therefore important to consider this effect on medicines, and be aware that this may change when treatment for thyroid dysfunction is started. The potential for medication interactions should also be considered.
This article aims to provide an overview of the common considerations for both physiological and pharmacological interactions encountered during the management of thyroid disorders.
Hypothyroidism refers to any state when thyroid hormone production is inadequate. In the UK, the annual incidence is 1–2% of the general population[1]
, with the incidence being six times greater among women. Potential hypothyroidism symptoms include tiredness, cold intolerance, constipation and weight gain.
Hypothyroidism is typically managed by administration of a synthetic form of T4, levothyroxine, or occasionally the synthetic form of T3, liothyronine. Both medicines are available as intravenous and oral preparations.
The peak therapeutic effect may not be achieved for several weeks, and there is a slow response to dose changes and effects of treatment persist for several weeks. As such, the dose should be individualised based on clinical response (e.g. improvement of symptoms) and biochemical tests (e.g. serum TSH, free T3 and free T4). The usual initial dose of levothyroxine for adults is 50–100µg once daily, adjusted in steps of 25–50µg according to response. The usual maintenance dose is 100–200µg once daily.
Oral liothyronine may be indicated in acute patients (e.g. those with severe hypothyroidism and hypothyroid coma). It is rapidly absorbed from the gastrointestinal tract, has a rapid onset of action of a few hours and short duration of action.
Hyperthyroidism occurs when the thyroid gland produces excessive amounts of thyroid hormones. The UK annual incidence of hyperthyroid disease is approximately 0.8% of the general population[2]
.
Propylthiouracil and carbimazole are antithyroid drugs used for the management of hyperthyroidism. They lead to a reduction in thyroid hormone synthesis through inhibition of thyroperoxidase, subsequently preventing the iodination of thyroglobulin. The drugs are administered orally and are rapidly absorbed from the gastrointestinal tract. They concentrate in the thyroid gland, and their duration of action is closely related to the intrathyroidal drug concentration, rather than plasma half-life. The elimination half-life may be increased in hepatic and renal impairment[3],[4]
.
Carbimazole and propylthiouracil can cause bone marrow suppression, and concurrent use with clozapine is contraindicated owing to the increased risk of this adverse effect[5]
.
Gastrointestinal absorption
Oral levothyroxine is variably absorbed from gastrointestinal tract, and metabolites undergo enterohepatic recycling; therefore absorption can be irregular. It should be taken on an empty stomach or at night, although in practice this may cause problems with adherence, as such regularly taking the medicine and meals at the same time of day is more important. Consistency when taking other medicines is also important, as binding interactions can occur.
As levothyroxine will be co-administered for prolonged periods, the significance of the interaction is often negligible, particularly as doses are individualised. However, the potential for an interaction is important when any medicine is started, adjusted or stopped, and can result in an inappropriate dose.
There is less evidence for interactions with liothyronine, although a similar mechanism of interaction may be assumed (see ‘Binding interactions with levothyroxine and liothyronine’).
Binding reactions with carbimazole and propylthiouracil have not been reported.
| Table: Binding interactions for levothyroxine and liothyronine | |||
|---|---|---|---|
| [6] Stockley’s Drug Interactions | |||
Medicine | Mechanism | Practical consideration | Further information |
Lanthanum carbonate | Gastrointestinal (GI) binding with the lanthanum ion | Interval of two hours between administration | Close monitoring of thyroid stimulating hormone levels during concurrent use. Adjust levothyroxine dose as appropriate |
Polystyrene sulfonate | GI binding | Separate doses as much as possible. Give ten hours apart (limited evidence) | |
Sevelamer | GI binding | Other drugs should be given one hour before or three hours after sevelamer | Limited evidence of the time interval between administration, recommendation based on guidance for similar interactions |
Sucralfate | Reduced absorption | ||
Aluminium hydroxide | Non-specific adsorption/ complexing | Consider alternative antacid | Monitor thyroid function and adjust dose accordingly |
Calcium carbonate | Adsorption at low pH (in the stomach) | Consider separating administration time by four hours if interaction suspected | Limited clinical importance for most individuals |
Ferrous sulphate | Production of an iron-levothyroxine complex | Considering separating administration by two hours | Monitor thyroid function and adjust dose accordingly |
Colestyramine, colesevelam, colestipol | Binding reaction in the GI tract, including enterohepatic recirculation | Administration interval of four to six hours; colestyramine and colestipol also appear to reduce the levels of endogenous thyroxine
| Significant interaction. Separation of doses diminishes the interaction |
Orlistat | Uncertain, presumed [12] binding in the GI tract in line with known interaction route of both drugs | Administration interval of four hours | Monitor thyroid function and adjust dose accordingly |
Close monitoring may be considered to be taking thyroid function tests every three months, as it takes two months to three months for TSH levels to stabilise following a change. Once stabilised annual measurement should be considered as levothyroxine requirements may change with ageing.
Distribution interactions
Protein binding affects the amount of free drug available. Levothyroxine is extensively protein-bound to thyroxine-binding globulin (TBG) and albumin[7]
. Circulating liothyronine is mostly bound to TBG[8]
, while thiamazole, the active metabolite of carbimazole, is moderately bound to plasma proteins, while 80% propylthiouracil is bound to plasma proteins.
Endogenous and exogenous oral sex hormone (oestrogens and androgens) levels affect the concentration of TBG. In normal thyroid function, the feedback loop and stimulation of thyroxine synthesis compensate for this, and maintain normal free thyroxine concentrations.
In hypothyroidism, this mechanism does not compensate; therefore patients taking levothyroxine who start taking sex hormones may require dose adjustment. Starting an oral contraceptive or hormone replacement therapy (HRT) increases TBG, reducing circulating thyroid hormone and thus requiring an increased levothyroxine dose, whereas starting androgens reduces the concentration of TBG, and patients may require dose reduction of the levothyroxine.
The interaction should not affect the efficacy of sex hormone therapy. Thyroid function should be assessed within several months of starting or stopping sex hormone therapy and the dose adjusted accordingly[9]
.
Metabolic interactions
Enzyme induction by rifampicin, carbamazepine, phenytoin or barbiturates enhances thyroid hormone metabolism, and can result in reduced serum concentrations. This interaction is of little significance for patients who have had the dose of levothyroxine titrated according to a clinical response and thyroid function test. However, clinical hypothyroidism can occur in patients taking levothyroxine if started on an enzyme-inducing drug, and the levothyroxine dose should be increased appropriately following a thyroid function test. Conversely, if the enzyme-inducing therapy is stopped, hyperthyroidism could occur[10]
.
Case reports indicate that use of chloroquine with proguanil for malaria prophylaxis may cause induction of liver enzymes, with a subsequent increased metabolism of levothyroxine. Monitoring of the thyroid function should be considered if an interaction is suspected.
Thyroid function interactions
Medicines used for the management of unrelated conditions may have a direct effect on thyroid function. The most commonly implicated drugs are amiodarone and lithium, and thyroid function should be monitored closely.
Amiodarone is known to have complex effects on thyroid function owing to its high iodine content. It has been implicated in causing both hyperthyroidism and hypothyroidism. Amiodarone may inhibit the peripheral de-iodination of T4 to T3 resulting in a decreased concentration of active hormone, which can cause more overt symptoms in patients with existing hypothyroidism Amiodarone is therefore contraindicated in patients with current or previous thyroid dysfunction.
Lithium may lead to clinical hypothyroidism due to a direct action on the thyroid gland, inhibiting the release of thyroid hormones.
Changes in thyroid status
As thyroid status influences metabolic activity, thyroid disorders and their subsequent correction may have a wide range of implications on medicines[11]
.
Antidiabetic medicines can be affected as correction of the hypothyroidism may increase insulin or oral hypoglycemic requirements. Therefore blood glucose monitoring should be performed and reviewed frequently in patients with diabetes starting treatment for hypothyroidism, for patients already monitoring their blood glucose, they may continue with the usual schedule, for patients that do not manage their own testing, they should ensure they have blood glucose checked every two to three months during the period of adjustment. As levothyroxine takes weeks to achieve therapeutic levels these changes may be prolonged.
Propranolol plasma concentrations are reduced in hyperthyroidism, probably owing to increased clearance. Propanolol may also inhibit the de-iodination of T4 to T3.
Digoxin serum concentrations appear to be lower in patients with hyperthyroidism and higher in those with hypothyroidism. Patients with hyperthyroidism have a degree of insensitivity to digoxin therapy, and therefore may require higher digoxin doses than normal, which then need to be reduced as treatment with antithyroid drugs is started. Conversely, patients with hypothyroidism may need digoxin doses increased as hypothyroidism is corrected. Proposed mechanisms for these effects include altered response of the heart due to changes in thyroid hormone levels, and altered glomerular filtration rates affecting digoxin clearance.
Oral anticoagulants(e.g. warfarin) can be affected by thyroid dysfunction, and patients will require increased monitoring of international normalised ratio (INR) when thyroid therapy is started, adjusted or stopped. The suggested mechanism is that changes to metabolic rates governed by the thyroid hormones affect the metabolism of clotting factors.
Hypothyroidism decreases the metabolism of clotting factors. Therefore, patients taking an anticoagulant may have been taking a higher dose than normally required to achieve their target INR. If such a patient starts treatment for hypothyroidism his or her dose of anticoagulant may need to be reduced. Conversely, patients with hyperthyroidism treated with anti-thyroid drugs may require an increase in the anticoagulant dose.
Starting other medicines that can alter thyroid function as an adverse effect (e.g. amiodarone) may also require the patient’s anticoagulant doses to be adjusted.
Theophylline levels may be modestly altered in thyroid dysfunction. In hyperthyroidism, theophylline metabolism is increased, and therefore the dose may need to be reduced as thyroid levels are corrected. Conversely, patients with hypothyroidism may need the dose of theophylline increased as treatment with levothyroxine or liothyronine continues.
Sallianne Kavanagh MPharm, MRPharmS, MSc is lead pharmacist for diabetes and endocrinology and joint chair of the UKCPA diabetes and endocrinology group, and Priya Boparai MPharm, Clin Dip is advanced pharmacist in medicines information and endocrinology, both at Sheffield Teaching Hospitals NHS Foundation Trust.
Correspondence: sallianne.kavanagh@sth.nhs.uk
References
[1] Clinical Knowledge Summaries, Hypothyroidism. Accessed on 2/4/2015, available at: http://cks.nice.org.uk/hypothyroidism
[2] Clinical Knowledge Summaries Hyperthyroidism. Accessed on 2/4/2015, available at: http://cks.nice.org.uk/hyperthyroidism
[3] Summary product characteristics, Carbimazole, Amdipharm Mercury Company Limited. Last Updated on eMC 29/9/2014. Accessed on 2/4/2015, available at: http://www.medicines.org.uk/emc/medicine/26933
[4] Summary product characteristics, Propylthiouracil, Wockhardt UK Ltd. Last updated on eMC 3/6/2013. Accessed on 2/4/2015 http://www.medicines.org.uk/emc/medicine/27760
[5] Summary product characteristics, Clozapine, Novartis Pharmaceuticals UK Ltd. Last updated on eMC 6/10/2014. Accessed on 2/4/2015, available at: http://www.medicines.org.uk/emc/medicine/1277
[6] Stockley’s Drug Interactions. Accessed on 2/4/2015, available at: https://www.medicinescomplete.com/mc/stockley/2010
[7] Summary product characteristics Levothyroxine, Amdipharm Mercury Company Limited. Last updated on eMC 25/9/2014. Accessed 2/4/2015, available at: http://www.medicines.org.uk/emc/medicine/22561
[8] Summary product characteristics Liothyronine, Amdipharm Mercury Company Limited. Last updated on eMC 18/9/2014. Accessed 2/4/2015, available at: http://www.medicines.org.uk/emc/medicine/24153
[9] Arafah BM. Increased need for thyroxine in women with hypothyroidism during estrogen therapy. N Engl J Med 2001;344:1743–1749.
[10] Lossius MI, Taubøll E, Mowinckel P et al. Reversible effects of antiepileptic drugs on thyroid hormones in men and women with epilepsy: a prospective randomized double-blind withdrawal study. Epilepsy Behav 2009;16:64–68.
[11] Martindale. Accessed 2/4/2015, available at: https://www.medicinescomplete.com/mc/martindale/current
You might also be interested in…

Identifying patients at risk of diabetes
