This content was published in 2011. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Key points
- Cushing’s syndrome can be treated with surgery, radiotherapy, chemotherapy and cortisol-inhibiting drugs or, in iatrogenic Cushing’s syndrome, steroid withdrawal.
- Some patients may need corticosteroid replacement therapy. They should carry a steroid card and wear a Medic-Alert bracelet.
- Patients on steroid replacement therapy will need special counselling related to timing of doses, symptoms of adrenal insufficiency and when emergency doses are required.
Cushing’s syndrome, characterised by symptoms caused by chronic exposure to excessive cortisol, was first described in the early 20th century. It affects one in 200,000 people and is five times more common in women than in men. It usually has a slow onset and is commonly diagnosed between the ages of 20 and 50 years. There are about five to six new cases per million per year1.
Cortisol and homeostasis
Cortisol is produced by the adrenal glands in response to hormonal stimulation from the master glands: the hypothalamus and pituitary. The hypothalamic hormone — corticotrophin releasing hormone (CRH) — stimulates the anterior pituitary to release adenocorticotrophic hormone (ACTH), which then acts on the adrenal gland so that it produces cortisol. Cortisol levels rise with increased levels of ACTH. When they reach a certain level, a negative feedback mechanism tells the pituitary to slow ACTH production.
Cortisol is a “fight or flight” hormone — stress provokes its release along with adrenaline. In stressful situations, such as trauma or illness, cortisol helps to maintain homeostatic balance — in the absence of corticosteroids, stress would result in hypotension, shock and death. Cortisol is classed as a glucocorticoid, although it has some mineralocorticoid properties. Glucocorticoids are non-specific cardiac stimulants that activate the release of vasoactive substances. Cortisol helps regulate blood pressure and cardiovascular function. It raises blood pressure by increasing the sensitivity of vascular muscles to catecholamines. It is also reported to effect carotid artery intima media thickness.
Under stress, the body’s natural response is to produce more cortisol, which helps to release energy (eg, via gluconeogenesis) to maintain metabolism and repair damage. So cortisol balances the effect of insulin on blood glucose control.
Cortisol also reduces the inflammatory response from the immune system, partly by a reduction in circulating T-cells.
Hypercortisolism
The most common cause of excess cortisol is excess ACTH as a result of a pituitary tumour. The condition is then termed Cushing’s disease, a subtype of Cushing’s syndrome and the most common cause of excess endogenous cortisol. Other types of endogenous Cushing’s syndrome are those that result from adrenal disorders (eg, benign or malignant tumours, hyperplasia) or ectopic ACTH. In cases of ectopic ACTH, neuroendocrine tumours (eg, bronchial carcinoid tumour and small cell lung carcinoma) produce ACTH outside the control of the pituitary. In this subtype, the ACTH levels are much more elevated than those resulting from pituitary tumour.
Use of high doses of corticosteroids for immunosuppression after organ transplant, in the treatment of chronic respiratory diseases, or factitious steroid abuse (a psychiatric disorder) can also cause Cushing’s syndrome. This is why patients on long-term corticosteroid therapy should be maintained on the lowest effective dose.
Symptoms
The clinical features of Cushing’s syndrome include:
- Skin changes Increased breakdown of skin and tissue proteins makes the skin more fragile and also causes weakening of capillaries —the skin can thin and easily bruise. Pigmented stretchmarks (striae) are also common, especially in ACTH dependent subtypes;
- Facial rounding and fullness (“moon face”) A round flushed face is a common presentation;
- Muscle wasting and myopathy Excess cortisol destroys muscle mass and patients tend to be weak;
- Truncal obesity Increased cortisol causes accumulation of fat deposits and a redistribution of fats to the face, neck and abdomen. In some people there is increased fat between the should blades (“buffalo hump”);
- Osteoporosis Fracture may be a presenting complaint because cortisol reduces bone formation;
- Psychosis or depression Excess steroid has a direct effect on the brain and tends to produce dramatic mood swings;
- Hypertension;
- Hirsutism High levels of cortisol affect the balance of sex hormones, leading to high androgen levels;
- Diabetes mellitus or glucose intolerance.
Diagnosis
Diagnosis is usually based on medical history, laboratory tests and scans. Old photographs can help identify physical changes such as facial fullness. No single test is perfect and several are usually needed. Some of these tests are described in Panel 1. Further tests and investigations include the CRH stimulation test, high dose dexamethasone suppression test and petrosal sinus sampling. Computed tomography and magnetic resonance imaging are useful for locating tumours.
Panel 1: Tests Used To Diagnose Cushing’s Syndrome
Urine cortisol Normally cortisol levels fall at night and are higher in the morning. A 24-hour urinary cortisol screening test provides an average measure of serum cortisol. Multiple collections over three or more separate periods may be required to provide a more accurate estimate of average cortisol production. A normal result in a symptomatic patient does not rule out excess cortisol because in cyclical Cushing’s syndrome the levels fluctuate over a longer period.
Dexamethasone suppression test Dexamethasone suppression tests are based on the ability of the synthetic glucocorticoid to suppress ACTH and cortisol production. An overnight test is useful where there is low clinical suspicion of Cushing’s syndrome. Oral dexamethasone 1mg is given at 11pm and the cortisol level is measured at 9am the next morning.
The standard low dose test, involves giving 500mg of dexamethasone orally every six hours for 48 hours. Blood is taken (for cortisol and sometimes ACTH levels) immediately before the first dose, usually prescribed to be administered at 9am on day 1. Blood is also taken at the end of the test (ie, at 9am on day 3 — six hours after the last dose of dexamethasone.)
Levels below 50nmol/L indicate suppression and would be expected in healthy subjects. Higher levels indicate suppression failure and Cushing’s syndrome.
Medicines that can affect test results include oestrogens, phenytoin, spironolactone and tetracyclines.
Salivary cortisol Measuring salivary cortisol is a simple and convenient way of obtaining a night-time sample. Patients are able to collect their samples at home. It is an expensive test, but gaining interest. Readings over several evenings are required to increase accuracy.
Treatment strategies
Iatrogenic Cushing’s syndrome is usually reversible on reduction or withdrawal of steroid therapy. However, prolonged excess exogenous steroids cause the normal cortisol production pathway to switch off —the body’s adrenocortical response is diminished — so treatment cessation must be gradual in order to avoid acute adrenal insufficiency (characterised by hypotension, which may lead to shock and death). In endogenous Cushing’s syndrome, the goals of therapy are to reverse the clinical manifestations of the syndrome by:
- Reducing cortisol secretion to normal;
- Eradicating any tumours that impair health;
- Avoiding hormonal deficiency and dependence on medication.
Treatment is usually a combination of the options, including surgery.
Surgery
Pituitary tumours can be removed with transsphenoidal surgery and this is usually the mainstay of treatment. Where the tumour is large, the pituitary can be damaged during the procedure and patients might require hormone replacement following surgery. Adrenal tumours can also be surgically removed. The procedure, an adrenalectomy, can also be done where pituitary surgery has failed to provide the expected outcome.
Corticosteroid replacement is usually required after adrenalectomy. This is described in Panel 2.
Radiotherapy
Pituitary radiotherapy can be used where surgery is contraindicated or fails to reduce cortisol levels. The expected outcomes are to control cortisol levels (in the case of active tumours) and to prevent regrowth of large tumours. Radiotherapy can take at least one to three years to take effect.
Chemotherapy
In cases of ectopic ACTH production (eg, in small cell lung cancer or carcinoid tumour) cytotoxic agents are used if tumours cannot be surgically removed. The choice of regimen depends on the type of cancer and how widespread it is.
Cortisol-inhibiting drugs
Cortisol-inhibiting drugs are used at various stages of therapy. They decrease adrenal corticosteroid production and are generally used for mild hypercortisolism or short-term in severe hypercortisolism before other therapies. They should only be initiated by endocrinologists familiar with their use.
In particular, high circulating levels of cortisol in Cushing’s syndrome makes patients more susceptible to infections and poor wound healing which, inevitably, will affect post-operative recovery. Excess cortisol also impacts on peri-operative management due to effects on, for example, blood pressure and blood glucose. These agents can, therefore, be used to reduce cortisol levels before surgery both to reduce morbidity and prevent complications.
Metyrapone
Metyrapone is a competitive inhibitor of 11β-hydroxylation. It inhibits the conversion of pregnenolone to cortisol in the adrenal cortex. It should be administered with food at an initial oral dose of 250mg three to four times daily. This can be increased every few days, according to response, to a maximum of 6g per day in three or four divided doses. The capsules should be taken with milk or after a meal, to minimise nausea and vomiting. Doses are either low (tailored to cortisol production) or high, in which case corticosteroid replacement therapy (see Panel 2) is also needed — if levels are markedly raised and symptoms disabling, a “block and replace” strategy may be used.
Side effects include hypotension, allergic skin reactions, hypoadrenalism and hirsutism. Metyrapone can also cause drowsiness and patients should be warned about the effect on performance of skilled tasks (eg, driving).
Long-term treatment can cause hypertension as the result of accumulation of desoxycorticosterone in the corticosteroid synthesis pathway2.
Ketoconazole
Ketoconazole inhibits 11β- hydroxylase and so the final conversion of pregnenolone to cortisol. In addition, it inhibits 17-hydroxylase and 18-hydroxylase activity as well as sex steroid production by action on C17-20 lyase.
Due to its C17-20 lyase inhibition and consequent anti-androgenic properties, ketoconazole is particularly useful in female patients with hirsutism but it can cause unacceptable gynaecomastia and reduced libido in male patients and alternative agents (eg, metyrapone) may be required.
A further advantage of ketoconazole is its inhibition of cholesterol synthesis, particularly low-density lipoprotein cholesterol.
Higher doses than those for antifungal therapy are needed. Treatment (unlicensed but commonly used) is usually started at an oral dose of 200mg twice daily.
Ketoconazole has a slower onset of action than metyrapone but it has been used successfully to lower cortisol levels in patients with different subtypes, including ectopic ACTH and invasive ACTH-producing pituitary carcinoma, with doses up to 1,200mg per day in up to four divided doses.
Ketoconazole should be taken with food for maximal absorption. Absorption is impaired when gastric acidity is decreased2 so acid neutralising medicines should not be used for at least two hours after taking ketoconazole tablets. In patients with achlorhydria and those on acid suppressants (eg, H2-antagonists, proton pump inhibitors), it is advisable to administer ketoconazole with a cola beverage2.
Monitoring of liver function (before treatment, at weeks 2 and 4, then monthly) is required due to a rare risk of fatal hepatotoxicity. Patients should be advised to seek immediate medical attention if they experience abdominal pain, fatigue, jaundice or dark urine.
Ketoconazole is mainly metabolised through cytochrome CYP3A4 so has potential for interaction with other drugs metabolised via this pathway. For example, use of simvastatin is contraindicated during treatment with ketoconazole but pravastatin can be used.
Panel 2: Steroid deficiency and replacement therapy
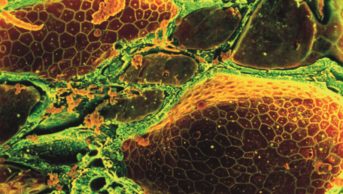
Adrenal glands Adrenal glands consist of two parts: the inner medulla (which makes catecholamines in addition to other sites of the body, [eg, the sympathetic nervous system]) and the outer cortex.
Most of the gland consists of the outer cortex, which has three layers. The outermost layer produces mineralocorticoids, of which the principal steroid is aldosterone. (Aldosterone helps regulate blood pressure by controlling salt and water retention in the body. Secretion is regulated by the renin-angiotensin system.)
The innermost layer secretes adrenal androgens in both men and women. The middle layer produces glucocorticoids, which are important for the body to maintain energy levels. Cortisol is the main steroid produced by this layer. cortisol replacement In patients with a history of Cushing’s syndrome, cortisol deficiency can occur after pituitary surgery, after adrenalectomy or with high doses of cortisol-inhibiting drugs such as metyrapone.
Cortisol replacement is usually required after surgery until the pituitary or remaining adrenal gland recovers. Life-long therapy may be required in some cases (eg, if the pituitary is damaged during surgery) and always after bilateral adrenalectomy. Depending on the extent of pituitary damage, there may also be need for other forms of hormone replacement (eg, levothyroxine).
Hydrocortisone The first-line drug for cortisol replacement is hydrocortisone (it is closest to cortisol) at a usual dose of 10 to 50mg per day, based on a hydrocortisone day curve assessment in hospital and clinical response. The day curve involves measuring a patient’s cortisol levels throughout the day while hydrocortisone is taken, allowing for dosing to be optimised. The aim is to achieve adequate cortisol levels throughout the day (peak <900nmol/L, trough >100nmol/L).
A standard regimen would be 10mg on waking (irrespective of meal); 5mg at lunchtime and 5mg with the evening meal. Larger doses are given in the morning and the smaller doses at the other times of the day to mimic natural cortisol production — natural levels fall during the day to a nadir at around midnight. The last dose should be taken by 6pm. Doing this also helps to minimise insomnia related to high cortisol levels.
Twice daily dosing can also be used, again with the larger dose in the morning.
Adrenal insufficiency Symptoms of adrenal insufficiency include severe nausea, extreme weakness, headache, dizziness, chills, confusion and muscle pain. Patients should be encouraged to carry a steroid card and wear Medic-Alert bracelet; they should also be educated on symptoms of adrenal insufficiency.
Doubling doses Patients on regular cortisol replacement therapy need to double their usual oral dose or administer an injection of hydrocortisone, where appropriate, during periods of stress or illness to mimic the body’s natural response to increasing cortisol output at such times.
Emergency steroid tablets and or injection can also be provided, for example, for patients on cortisol-inhibiting drugs who do not routinely require daily cortisol administration but may need urgent replacement if symptoms suggestive of adrenal insufficiency occur while on the cortisol inhibitor. A review of therapy is needed urgently and patients must seek immediate medical attention.
At my centre, all patients on steroid replacement are given hydrocortisone injection and counselled on when and how to use it, but injections should be available from community pharmacies if necessary. Hydrocortisone sodium phosphate solution for injection is the preferred form to reduce any delays, difficulties and risks that may be encountered by patients or carers in reconstituting hydrocortisone powder for injection before administration. There is campaign by the Pituitary Society to make hydrocortisone injection available in a device similar to that used for Epi-Pen.
Other steroids Prednisolone 7.5mg per day or dexamethasone 750mg per day (both have predominantly glucocorticoid activity) can be used in place of hydrocortisone — these are given twice daily with the same principle of a larger morning dose. Higher steroid doses (doubling of the usual dose) may be needed in patients on enzyme-inducing drugs such as rifampicin.
Additional mineralocorticoid replacement is needed after bilateral adrenalectomy. Fludrocortisone is the drug of choice here and usually given at 50–300mg per day in up to two divided doses. The dose of fludrocortisone does not require adjustment with common illnesses treated at home.
Side effects Side effects are less likely to occur when physiological doses (equivalent to prednisolone 7.5mg per day) or lower are used, as is the case with replacement in most patients. Patients are monitored and careful adjustment of dosage is crucial to preventing development of side effects. Gastrointestinal effects can occur and patients can be advised to take their medicine after food. It is important, however, to emphasise the need to take the first morning dose on waking even if this means taking on empty stomach and having a meal shortly after.
Mitotane
Mitotane selectively inhibits the activity of the adrenal cortex. It has a direct cytotoxic effect in adrenal carcinoma, shrinking adrenal tumours and decreasing steroid production. It takes six to eight weeks for a maximal effect and metyrapone can be used to bridge therapy at the start (eg, six-week overlap). Gastrointestinal side effects, such as anorexia, nausea and vomiting, and endocrine side effects, such as hypogonadism and thyroid disorders, are very common with mitotane. Neurotoxicity can also occur. Plasma concentrations should be monitored with the aim of 14–20mg/L as the optimal range for efficacy while avoiding toxicity. The usual dose range is 2–6g/day in three divided doses taken with or after food to minimise the gastrointestinal effects.
Patients should be advised to seek immediate medical attention if injury, infection or illness occurs (because of risk of acute adrenal insufficiency). Glucocorticoid replacement may be necessary.
Prolonged bleeding time has been reported in patients treated with mitotane and this should be taken into account when surgery is considered. Mitotane has also been reported to accelerate the metabolism of warfarin through hepatic enzyme induction, leading to an increase in dose requirements for warfarin. Close monitoring is, therefore, required when administering mitotane to patients on coumarin-like anticoagulants2.
Fat tissue can act as a reservoir for mitotane, resulting in a prolonged half-life and drug accumulation, so monitoring mitotane plasma levels (eg, every two months) is also necessary after interruption or cessation of treatment, because prolonged release of mitotane can occur. Caution and close monitoring of mitotane plasma levels are recommended when treating overweight patients2.
Mifepristone
Mifepristone is licensed as an abortifacient. It is a glucocorticoid and progestin receptor antagonist. Several reports3,4 have described a potential benefit in antagonising the effects of hypercortisolism before surgery or while awaiting radiotherapy induced remission. The initial oral dose is 200mg twice daily or 6mg/kg/day. The dose can be titrated up to 25mg/kg/day according to symptomatic response.
Careful attention must be paid to clinical signs of adrenal insufficiency and dose increases should be gradual. Efficacy is difficult to monitor via serum ACTH and cortisol levels because the drug antagonises hypercortisolaemic effects at the receptor level rather than altering corticosteroid production. Hypokalaemia can occur and patients should be closely monitored and treated with spironolactone where necessary.
Etomidate
Etomidate is an imidazole-derived anaesthetic agent which was reported to have an adverse effect on adrenocortical function in the early 1980s. When used for its licensed indication in anaesthesia, a single induction dose blocks the normal stress-induced increase in adrenal cortisol production for up to eight hours.
Compared with ketoconazole (also an imidazole), etomidate more potently inhibits adrenocortical 11β-hydroxylase. It inhibits 17-hydroxylase to a similar extent but has less effect on C17-20 lyase. At higher concentrations, it also appears to have an effect on cholesterol side-chain cleavage. There have been case reports5, 6 of its use (unlicensed) to reduce hypercortisolaemia in seriously ill patients with Cushing’s disease or ectopic ACTH syndrome.
Etomidate is usually given by continuous intravenous infusion at a dose of 2.5–3.0mg/hour (non-hypnotic dose), which is adjusted based on the serum cortisol levels. Its use is limited by the requirement for chronic intravenous administration. Nevertheless, it is an effective, rapidly acting adrenolytic agent and can be life-saving in hypercortisolic emergencies where high levels of cortisol result in markedly elevated blood pressure and gastric ulceration. Use is short-term (usually no more than seven days) under the care of an endocrinologist and with close monitoring of cortisol and blood pressure. Supplementation with exogenous cortisol is usually needed at some point during treatment (initiation guided by cortisol levels) to maintain an appropriate serum cortisol level (eg, as essential for post-operative recovery).
Panel 3: Counselling
Taking hydrocortisone tablets:
- Take your tablets as recommended; the first tablet(s) of the day should be taken immediately on waking (ie, before getting out of bed). The evening dose should be taken no later than 6pm;
- Carry a steroid card giving details of your current dose of steroid tablets and the names and contact details of your next of kin and hospital doctor;
- Never stop taking your steroids suddenly.
When you are ill
- If you have a mild illness (eg, a cold with no fever) then you do not need to change your dose. If you have a fever and feel more unwell (eg, influenza, infection) you need to take twice your normal number of tablets until you are well again. (Where steroid tablets are not taken regularly but have been prescribed for emergency use only, patients should be advised to take them as prescribed);
- If you are seriously ill and have diarrhoea or are vomiting then you will need an emergency hydrocortisone injection.
Hydrocortisone injection
- Carry an injection with you at all times and check its expiry date regularly;
- When needed, follow the relevant instructions for the product (eg, to prepare the injection);
- Inject 100mg intramuscularly through clean bare skin on the right or left upper thigh as taught by your nurse;
- Seek medical help if there is no improvement within 24 hours.
Pharmacist support
Pharmacists can offer support in a number of ways, including:
- Ensuring appropriateness of medication and dosing, including gradual titration where advised
- Monitoring effectiveness and toxicity of therapy
- Providing guidance on dose adjustment of any interacting drug where relevant
- Ensuring appropriate procedures are followed with the unlicensed use of medicines
- Providing adequate drug information to patients (eg, how it works, dose, when to take it and important side effects to look out for)
- Counselling patients and emphasising the need to seek medical attention when symptoms suggestive of adrenal insufficiency are experienced.
- Advising on the use of emergency hydrocortisone packs where prescribed (see Panel 3)
- Signposting patients to support groups.
Signposting
- The Pituitary Foundation has local support groups and further information can be obtained from www.pituitary.org.uk
- Further information for patients on Cushing’s syndrome is available from the Association for Cushing’s Treatment and Help (www.acthcushings. org.uk)
Practice points
Reading is only one way to undertake CPD and the regulator will expect to see various approaches in a pharmacist’s CPD portfolio.
1. Make sure your patients on long-term steroids have a steroid card.
2. Check that your patients on cortisol replacement (eg, hydrocortisone tablets) are taking their doses correctly.
3. Broaden your overview of pituitary disorders by visiting www.pituitary. org.uk
References
1. The Pituitary Foundation website www.pituitary .org.uk (accessed 25 April 2011).
2. Summaries of product characteristics for Metopirone 250mg capsules, Nizoral tablets and Lysodren 500mg tablets. Available at www.medicines.org.uk (accessed 25 April 2011).
3. Chu JW, Matthias DF, Belanoff J, Schatzberg A, Hoffman AR, Feldman D. Successful long term treatment of refractory Cushing’s disease with high-dose mifepristone (RU 486). J Clin Endocrinol Metab 2001;86:3568–73.
4. Johanssen S & Allolio B. Mifepristone (RU 486) in Cushing’s syndrome. Eur J Endocrinol 2007;157:561–9.
5. Drake WM, Perry LA, Hinds CJ, Lowe DG, Reznek RH, Besser GM. Emergency and prolonged use of intravenous etomidate to control hypercortisolemia in a patient with Cushing’s syndrome and peritonitis. J Clin Endocrinol Metab 1988;83:3542–4.
6. Moyes VJ, Wat W, Akker SA, Drake WM, Monson JP. Use of etomidate for control of severe hypercortisolism. Endocrine Abstracts 2005;9:P214.