This content was published in 2013. We do not recommend that you take any clinical decisions based on this information without first ensuring you have checked the latest guidance.
Meningococcal disease is caused by infection with Neisseria meningitidis and presents as bacterial meningitis (15 per cent of cases), septicaemia (25 per cent of cases), or a combination of the two1. It is the leading infective cause of death in early childhood.
Neisseria meningitidis, often termed meningococcus, is an aerobic, Gram-negative bacterium. Pathogenic strains have a polysaccharide capsule that helps the bacteria resist phagocytosis and complement-mediated lysis. Strains without a capsule are usually not pathogenic. Almost all invasive disease is caused by one of five of the antigenically distinct capsule serogroups: A, B, C, Y and W135.
Meningococcal disease shows marked seasonal variation, with a peak in winter. It can occur at any age but children younger than nine years are the most at risk (due to lower immunity), with a peak incidence in those under one year. There is a smaller, secondary peak in incidence in young adults aged 15–19 years owing to increased exposure and higher rates of carriage caused by close social interactions.
Apart from age, risk factors for the development of meningococcal disease include passive smoking, preceding influenza A infection, overcrowding, immunodeficiency and abnormal spleen function (asplenia). There are approximately 1,700 reported cases of meningococcal disease each year in England and Wales.
Transmission and carriage
Meningococci are carried in the nasopharynx in about 10 per cent of the population. Carriage is usually without ill effects and may contribute to the development of immunity against meningococcal disease. In less than 1 per cent of colonised people the organism penetrates the mucosal cells and enters the bloodstream; in 50 per cent of these cases the organism crosses the blood-brain barrier and causes purulent meningitis. Meningococci are transmitted via aerosol droplets and those in close contact with a case are particularly at risk — risk of transmission is estimated to be two to four cases per 1,000 household members which, although low, is 500–800 times the risk of transmission in the general population2.
Because the bacteria cannot survive for long outside the human body, infection cannot be caught from water supplies, swimming pools or buildings. Meningococcus cannot be carried on objects such as cups, toys, furniture or clothing.
Course of the infection
The incubation period of meningococcal disease is three to four days, with a range of two to 10 days. Once meningococci enter the bloodstream, they multiply rapidly. If the bacteria cross the blood-brain barrier, meningitis develops. In other cases, overwhelming septicaemia causes death before meningitis can develop. As meningococcal bacteria multiply in the cerebral spinal fluid (CSF), the meninges become inflamed and swell. This increases pressure on the brain, producing the classic symptoms of meningitis such as headache, stiff neck and photophobia. As the disease progresses, patients will become drowsy, confused and delirious. They may have seizures and eventually lose consciousness.
In meningococcal septicaemia inflammation causes increased vascular permeability, pathological vasoconstriction and vasodilation, intravascular coagulation and profound myocardial dysfunction, leading to the development of shock and multiorgan failure.
Cardiovascular failure and peripheral shutdown leads to symptoms such as pale skin, cold hands and feet, and rapid breathing. Blood leaking into the surrounding tissues shows up as the typical non-blanching meningococcal rash. Without treatment the circulatory system is overloaded and the patient collapses. Urgent and aggressive resuscitation is required.
Although prompt recognition of the signs and symptoms of meningococcal disease is essential, half of children with meningococcal infection are sent home after their first primary care consultation because the conditions may, initially, be difficult to distinguish from other less severe (viral) infections.
However, the time-window for clinical diagnosis is narrow. Most patients have only non-specific symptoms in the first four to six hours — the “prodromal phase”, but may be close to death by 24 hours. The classic features of purpuric rash, stiff neck, photophobia, and impaired consciousness develop late (median onset 13–22 hours). However most patients have early symptoms of sepsis (leg pains, cold hands and feet, abnormal skin colour) that first develop much earlier4.
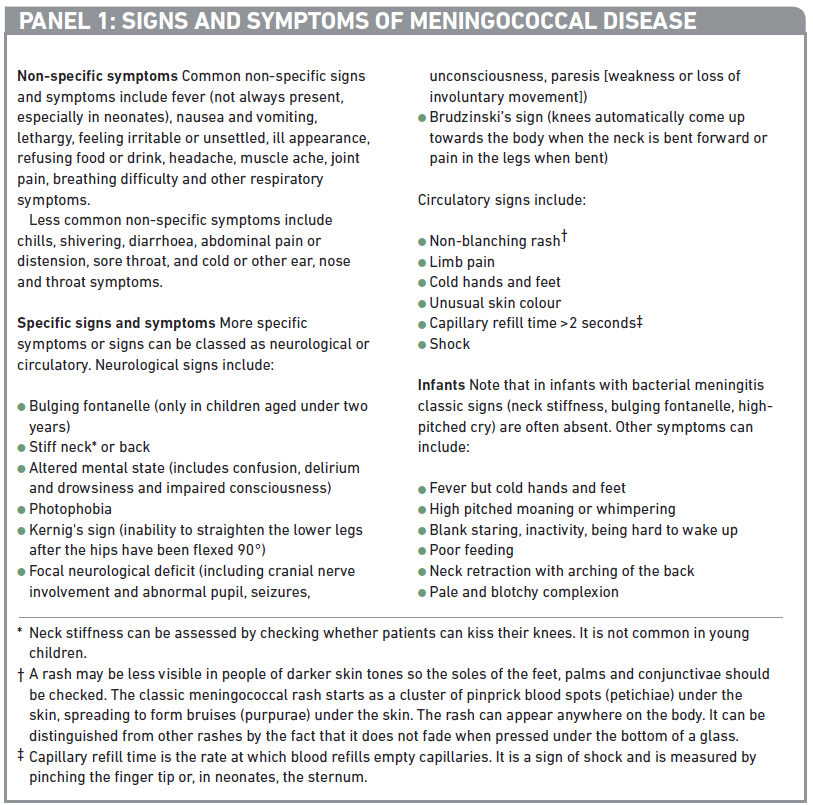
Panel 1 summarises the signs and symptoms to look out for.
According to a survey by the Meningitis Research Foundation, only 4 per cent of patients and carers sent home from the GP remembered having the symptoms of meningitis and septicaemia explained. Pharmacists could play a valuable role in educating the public on these.
Likely prognosis
Untreated meningococcal infection spreads rapidly and is fatal in about 50 per cent of cases. Up to 20 per cent of the children who contract severe meningococcal septicaemia die, usually within 24 hours of the first symptoms appearing and frequently before the patient receives specialist care. The fatality rate is influenced by a number of factors, including serogroup of the infecting pathogen, age and prompt antibiotic treatment (see later). More deaths are caused by septicaemia than by meningitis.
If meningococcal disease is treated promptly most people make a full recovery. However, about one in eight people experience some long-term effects. These can include headaches, joint stiffness, epilepsy, deafness and learning difficulties. Behavioural and emotional effects are common, although these usually resolve.
Septicaemia may lead to tissue necrosis and scarring which, in extreme cases, can result in the amputation of digits and even limbs.
When to refer
In the presence of a high temperature plus any of the following “red flag” symptoms an ambulance should be requested immediately:
- Limb pain, cold hands and feet, pale or mottled skin and blue lips and, in young children, drowsiness, rapid or laboured breathing, diarrhoea (ie, symptoms of early septicaemia);
- Non-blanching rash, particularly with fever, ill appearance or neck stiffness;
- Bulging fontanelle;
- Decreased level of consciousness;
- Convulsive status epilepticus.
Children with non-specific signs and who do not require referral should be offered a “safety net”. This means one or more of the following:
- Encouraging the parent, carer or patient to trust their instincts and reseek medical help if the illness gets worse, even if this is shortly after the patient has been seen
- Advising on access to further healthcare advice (including after normal working hours)
- Giving information about symptoms of serious illness, including how to identify a non-blanching rash
Parents and carers should be advised that if they are concerned they should check on an unwell child during the night and to be aware that an unsettled child who suddenly becomes quiet may be deteriorating.
It is worth noting that a survey has revealed six out of 10 parents would not feel confident recognising the signs of meningitis. A “meningitis early alert pack” (Arc) may help parents and carers quickly identify symptoms and can be a reassuring tool. It contains a device for identifying a non-blanching rash (i.e., replicating the tumbler test) a forehead thermometer and a chart to monitor fever and medication. It also describes the critical signs and symptoms and includes an image of the typical rash.
Pre-admission management
If meningococcal infection is suspected in primary care, patients should be transferred to an appropriate secondary care facility as soon as possible. Before transfer, supportive management, such as oxygen and intravenous fluids, should be given if facilities to do so are available.
The effectiveness of antibiotic therapy given before hospital admission is inconclusive because disease severity varies depending on presentation to primary care professionals. Consensus based recommendations and the National Institute for Health and Clinical Excellence3, however, suggest that patients with suspected bacterial meningitis but without a rash should be transferred to hospital directly without giving antibiotics because the disease progresses more slowly than septicaemia5. However, if urgent transfer is not possible (eg, in adverse weather conditions or remote locations), it is appropriate to administer antibiotics before transfer. (Meningitis is also caused by other bacteria such as group B streptococcus, E coli, Listeria species, Streptococcus pneumonia and Haemophilus influenzae type B (Hib). Viral meningitis is common but usually is less severe. Meningitis can also occur after neurosurgery.)
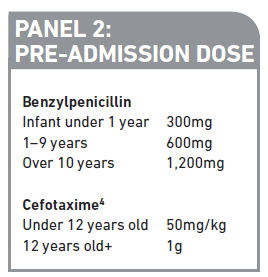
Patients with suspected meningococcal disease (i.e., meningitis with a rash or meningococcal septicaemia) should be given antibiotics at the earliest opportunity. GPs and ambulance crews are able to administer antibiotics en-route to hospital where required. The antibiotic of choice for immediate administration is benzylpenicillin given by intravenous or intramuscular (see Panel 2). Rash or nausea after previous doses of penicillin is not a contraindication for benzylpenicillin3. However, if the patient has a clear history of anaphylaxis after a previous dose of a penicillin, cefotaxime (see Panel 2) should be given instead. When cephalosporins are contraindicated, intravenous chloramphenicol may be used.
Diagnosis
Along with thorough examination of the patient and monitoring of vital signs, diagnosis is made by blood tests for C-reactive protein levels and white blood cell count together with examination of the CSF (taken by lumbar puncture) for white cells and protein — both are raised in bacterial meningitis. A polymerase chain reaction (PCR) blood test is also performed to look for Neisseria meningitides DNA.
Blood and CSF should be taken as soon as meningitis is suspected and, if possible, before antibiotic administration because CSF fluid can become sterile soon after antibiotic administration. If antibiotics have been given before these tests are performed this is taken into account in the analyses — antibiotics should never be delayed if there are problems or contraindications to performing lumbar puncture. The results of these tests are usually available within four hours.
Blood and CSF are also sent to microbiology for culture. A computed tomography scan is sometimes performed to look for space occupying lesions or abscesses within the brain.
Further management
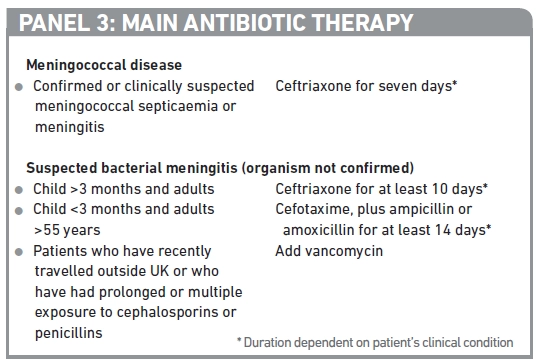
Depending on their clinical condition, patients may be managed on a general ward or in intensive care. Supportive therapies such as fluid replacement, respiratory support and correction of metabolic disturbances are given in response to the patient’s clinical condition. The mainstay of therapy, however, is intravenous antibiotics. The treatment courses in Panel 3 are recommended.
Third generation cephalosporins are the preferred choice for both meningococcal disease and bacterial meningitis because their broad spectrum covers meningococcus as well as other meningitis-causing pathogens. Although CSF penetration is usually poor, in patients with inflamed meninges cephalosporins are able to cross the blood-brain barrier in sufficient concentrations. Ceftriaxone may be used in children under three months of age but should not be used in premature babies or in those with abnormal liver function. Ceftriaxone should not be administered at the same time as calcium-containing fluids because this can cause precipitation.
Ampicillin or amoxicillin is added for children under three months or adults over 55 years to cover Listeria spp. Vancomycin is added when there are concerns of pneumococcal resistance (eg, recent travel or prolonged antibiotic exposure).
The results of blood or CSF cultures can confirm the causative organism and may change the choice of antibiotic after the initial empirical therapy — results are usually available 72 hours after admission.
Adjunctive early steroid administration reduces inflammation in the subarachnoid space in patients with bacterial meningitis — this inflammation is thought to contribute to mortality and morbidity. Corticosteroid administration has also been shown to reduce the risk of severe hearing loss and long-term neurological sequelae, such as cognitive impairment, compared with placebo in patients with bacterial meningitis3. However, there is no evidence of these benefits in neonates so this therapy is only indicated in children over three months old and adults. Treatment should be started within four hours of the first dose of antibiotics in patients with suspected or proven bacterial meningitis. The drug of choice is dexamethasone 0.15mg/kg (max 10mg) every six hours for four days.
In patients with meningococcal septicaemia and shock dexamethasone is not recommended by NICE because there are no proven benefits in terms of reduction in the severity of complications or improvement in mortality data. However, patients may receive hydrocortisone in intensive care units as an adjunct to vasoactive agents for severe sepsis.
Vaccination and control
Vaccination against meningococcus has been part of the UK routine immunisation programme since 1999 —this has corresponded to a reduction in the number of cases of meningococcal meningitis. Before the introduction of the group C vaccines, meningococcal C strains caused around 35–40 per cent of cases. The vaccine, extracted from cultures of group C Neisseria meningitidis, is given to infants at three and four months of age as part of routine immunisation. An additional booster dose is given at one year. People with additional risk factors for developing meningococcal disease, such as asplenia or complement deficiency, should receive vaccination with the MenACWY conjugate vaccine, which contains extracts from cultures of serogroups A, C, W135 and Y.
Travellers from the UK to areas where the risk of contracting meningococcal infection is high are also advised to be vaccinated with the MenACWY conjugate vaccine. Vaccination is an entry requirement to Saudi Arabia for haj pilgrimages and some community pharmacies offer this as a clinical service. The vaccine should have been received not more than three years and not less than 10 days before arrival. Two national outbreaks of disease due to W135 strains, previously rare in the UK, followed the haj pilgrimages in 2000 and 2001.
Group B strains now account for around 90 per cent of all cases with only around 1–2 per cent of cases caused by group C strains. A vaccine against group B Neisseria meningitides is expected to be available early in 2013 and is likely to be included in the routine childhood vaccination schedule. Successful introduction of a group B vaccine would significantly reduce the number of cases of meningococcal disease in the UK but the risk of being infected by strains that are not covered by routine immunisation remains.
Prophylaxis
Meningococcal disease is a notifiable disease and the relevant health protection authorities should be notified of every suspected and confirmed case. Risk of transmission to other people is low but prophylactic antibiotics should be given to people who have had prolonged close contact with the patient during the seven days before onset of illness (eg, those living in the same household, pupils in the same dormitory, students sharing a kitchen in halls of residence) and healthcare staff who have had transient close contact with a patient and have been directly exposed to large particle droplets or secretions from the respiratory tract (eg, during intubation).
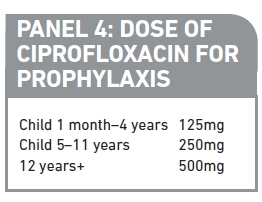
A single dose of ciprofloxacin (see Panel 4) is recommended prophylaxis for all age groups and in pregnancy and breast feeding1. The dose should be given as soon as possible — ideally within 24 hours of the patient’s diagnosis. If ciprofloxacin is contraindicated rifampicin is the preferred second-line antibiotic although it must be given twice daily for two days and there are number of contraindications. If rifampicin is not appropriate, azithromycin or ceftriaxone stat doses may be prescribed as alternatives.
Vaccination with the appropriate product should be offered to all those who have received prophylactic antibiotics within four weeks of diagnosis1. If clusters of infection occur in an institution, public health services will advise on the appropriateness of prophylaxis and vaccination.
Follow up
Formal audiological assessment should be carried out on all patients as soon as possible. Children and young people should be reviewed by a paediatrician within six weeks after discharge. Patients may also need referral for complications. All patients should be offered information about and access to further care after discharge as well as contact details of patient support organisations (see Signposting).
Signposting
- The Meningitis Research Foundation (www.meningitis.org) gives information about symptoms and vaccination, and offers support after a case of meningitis or septicaemia, including bereavement support.
- The Meningitis Trust (www.meningitis-trust.org) support services include home visits, financial grants, practical help, family days and counselling.
- Meningitis UK (www.meningitisuk.org) offers help and advice.
Practice points
Reading is only one way to undertake CPD and the GPhC will expect to see various approaches in a pharmacist’s CPD portfolio.
1. Consider stocking leaflets on meningitis symptoms, which can be kept at home and used as a quick reference.
2. Make sure your staff are trained to check for “red flag” symptoms and to offer “safety net” advice where appropriate.
3. A number of free apps provide quick reference guides and reminders of signs and symptoms. Search meningitis in the App Store or Google Play to explore what is available.