Greg Wright / Alamy
In this article you will learn:
- How to assess a patient who has fallen and lost a tooth
- The steps you should take to preserve and replant a tooth
- How to support patients following the replacement of a tooth
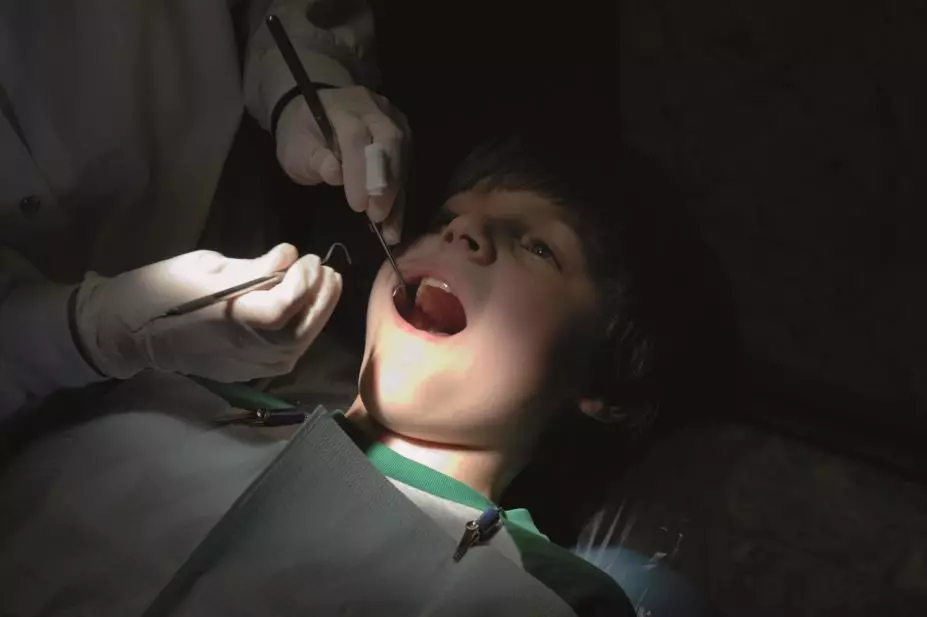
A ten-year-old boy trips on the pavement outside the pharmacy and knocks one of his permanent front teeth out of its socket (see Figure 1). His mouth is bleeding and, although he appears a little stunned, he is conscious and aware of his surroundings. His mother has retrieved the tooth and is holding it in her hand.
What should you do?
Step one: assessment
Avulsion (complete displacement) of a permanent tooth is a relatively common dental emergency, and seen in up to 3% of dental injuries[1]
.
First, assess the boy’s injuries to ensure they are limited to the lost tooth; in particular, the boy should be checked for signs of head injury (e.g. vomiting, impaired consciousness, disorientation) and referred to a local emergency department if necessary. Assuming the wound is limited to the lost tooth, the boy should be instructed to gently bite on a piece of gauze to absorb the blood from the socket.
There is no medical contraindication to replanting a tooth. However, you should confirm whether or not the boy has any clinically significant medical conditions (e.g. bleeding disorders) or is taking medicines that could affect treatment (e.g. immunosuppressants). These should be recorded and passed on to the patient’s dentist (see step three).
While this assessment is being performed, the tooth should be stored in saline or milk.

Source: Richard Welbury
Figure 1: In the case shown, a ten-year-old boy lost his upper right permanent central incisor tooth after a fall.

Source: Richard Welbury
Figure 2: The tooth was recovered and replanted under local anaesthesia, then held in position with a flexible splint, consisting of orthodontic brackets and wire, for 14 days.

Source: Richard Welbury
Figure 3: The splint was removed after 14 days. Root canal treatment was required because the tooth had been out of the mouth for nearly 70 minutes before it was replanted, and the dental pulp did not survive.
Step two: replant the tooth
If the tooth is intact, it should be replaced immediately into its socket after removal of any obvious foreign debris; this can be done by anyone present. Primary (also known as milk or baby) teeth should not be replanted.
The success of replanting the tooth depends on the action that is taken immediately after the avulsion[2]
; reducing the time the tooth is out of the mouth and preventing the root surface from drying can markedly improve prognosis.
An avulsed tooth should be held by the crown, avoiding contact with the tapered root. It should then be rinsed under cold running water for a maximum of ten seconds to remove debris, before being placed back into the socket root-first. The patient should then be instructed to bite gently on a piece of gauze to hold the tooth in position.
If the tooth cannot be replanted immediately, it should be placed in milk or normal saline. It is still worth storing a tooth that is not intact (fractured) so the dentist can make a final decision whether repair is possible. These storage media are iso-osmolar and help preserve the vitality of the periodontal ligament cells.
If it is not possible to store an avulsed tooth in milk or saline, it should be wrapped in cling film and not be allowed to become dry. Drying the surface of the periodontal ligament by wrapping the tooth in a tissue or handkerchief reduces the chances of the tooth being replanted successfully and is not recommended.
The boy’s mother should then be advised to take him to a dentist as soon as possible.
Why is this urgent?
The length of time the tooth has been out of its socket and not kept wet is called the extra-alveolar dry time (EADT). Current guidelines[2]
suggest that if a tooth has been dry for less than 60 minutes the cells of the periodontal ligament – the fibres that attaches the tooth to the bone – can survive. If these cells do not remain vital, they will be a source of necrotic tissue and ultimately result in tooth loss. Research indicates that after five minutes the risk of permanent damage to the cells starts to increase significantly[3]
.
If the EADT is greater than 60 minutes, the risk of ankylosis (fusion of the root of the tooth directly to the bone), typically followed by bone remodelling and root resorption, is high and can lead to premature tooth loss. This risk is even greater for younger children in whom the root tip has not fully formed (referred to as an immature apex).
Step three: dental care
The aim of reimplanting an avulsed tooth in a child is to ensure the tooth is in its correct place in the dental arch at least until full facial alveolar growth has occurred (usually at age 18–20 years). This allows all neighbouring teeth to erupt into their correct positions. Following this age, if the reimplanted tooth is lost it can be replaced by a permanent dental implant or dental bridgework.
Once replanted, the tooth needs to be splinted to keep it in place while it reattaches to the socket. This procedure is performed under local anaesthesia using a flexible splint consisting of orthodontic brackets and wire (see Figure 2).
After the tooth has been splinted, care must be taken to prevent infection of the affected area. This can be done by advising the patient to:
- Brush teeth twice a day (morning and night as normal) and, if feasible, after eating at lunchtime;
- Use chlorhexidine mouthwash (0.2%) twice a day to help reduce the amount of plaque and improve oral cleanliness.
In accordance with International Association of Dental Traumatology guidelines[1]
, a five-day course of an antibiotic should also be prescribed (phenoxymethylpenicillin, amoxicillin, or tetracycline if there is a history of allergy to penicillin). A tetanus booster is also advised if history of cover is uncertain.
The splint can be removed after 14 days following the removal (extirpation) of the dental pulp by the dentist. The dental pulp contains the nerve supply and blood vessels to the tooth, but commonly becomes necrotic in an avulsed and reimplanted tooth. If the pulp is not removed, this can cause recurrent infection that can spread to the alveolar bone of the jaw. If the dental pulp has not survived, the patient may require root canal surgery.
Extirpation may not be necessary for a tooth with an immature apex that has been out of the mouth for less than 30–45 minutes. This is because the pulp of such teeth may undergo regeneration and retain its vitality.
Care checklist for avulsed teeth
Pharmacists can improve the likelihood of a tooth being successfully replanted by taking the following steps:
- Check for any signs or symptoms of a head injury (e.g. vomiting, loss of consciousness, disorientation) that require urgent referral to a local emergency department;
- Determine if the person has any medical complications (e.g. bleeding disorders) that would require specialist assistance;
- Confirm the avulsed tooth is permanent, as primary teeth should not be replanted;
- Hold the tooth by the crown and rinse under cold, running water for up to ten seconds to remove debris;
- Replant the tooth into its socket;
- Instruct the individual to hold the tooth in position by lightly biting down on a gauze or handkerchief;
- If replantation is not possible, store the avulsed tooth in normal saline or milk, or wrap it in cling film to avoid it drying;
- Seek emergency dental treatment.
Christine Lyttle, BSc, MFDSRCPSG, is a core trainee and Richard Welbury, PhD, FDSRCPSG, is professor/honorary consultant in paediatric dentistry, both at the Oral Health Directorate at Glasgow Dental Hospital and School. Nairn Wilson, PhD, FDS, is professor of dentistry at King’s London Dental Institute.
References
[1] Andersson L, Andreasen JO, Day P et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: Avulsion of permanent teeth. Dental Traumatol 2012;28:88–96.
[2] Andreasen JO, Andreasen FM & Andersson L. Textbook and color atlas of traumatic injuries to the teeth. Oxford: Blackwell 2007.
[3] Kinirons MJ, Gregg TA, Welbury RR et al. Variations in the presenting and treatment features in reimplanted permanent incisors in children and their effect on the prevalence of root resorption. Br Dent J 2000;189:263–266.


