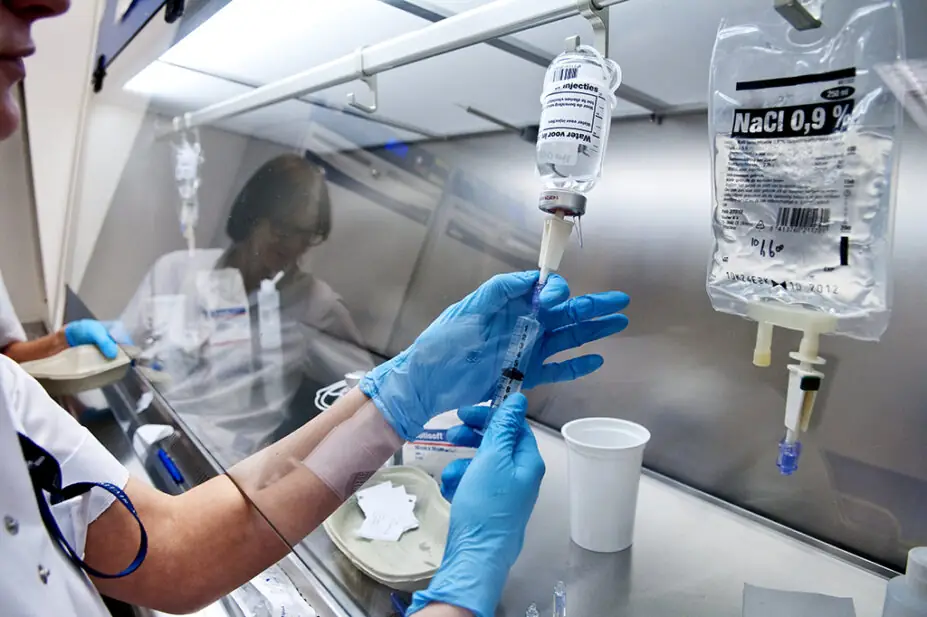
ARNO MASSEE / SCIENCE PHOTO LIBRARY
Allowing pharmacy technicians to supervise the preparation, assembly and dispensing of medicines in hospital aseptic facilities will increase the “risk of catastrophic clinical error”, the Pharmacists’ Defence Association (PDA) has said.
The comment came in a position statement in response to the Department of Health and Social Care’s (DHSC’s) consultation on pharmacy supervision, which sets out proposals to amend the Medicines Act 1968 and The Human Medicines Regulations 2012.
In the statement, published on 19 February 2024, the PDA outlines why it does not support one of three proposals included in the consultation: to “permit registered pharmacy technicians to supervise the preparation, assembly and dispensing of medicines in hospital aseptic facilities”.
The PDA said that although pharmacy technicians may be the most experienced individuals for the technical aspects of a technical process in an aseptic unit, “this can never substitute for the clinical knowledge, understanding and decision-making skills of the pharmacist”.
It raised concerns that pharmacy technicians would not have the clinical knowledge “to make or suggest changes to clinician colleagues in the wards”, such as when an urgent substitute is required for a product in short supply.
“The risk of catastrophic clinical error will increase as pharmacy technicians do not have the underlying clinical knowledge of a pharmacist,” it said.
The PDA added that the “proposal fails to address the systemic problem around recruitment and retention of staff” and calls for “a more holistic approach to pharmacy staffing within hospital settings”.
It argued that the proposed governance system, in which a hospital chief pharmacist would oversee the activities of an aseptic unit, is “inherently unsafe” because the pharmacist is “too far removed from the day-to-day activities of an aseptic unit to exercise any meaningful oversight role”.
“Removing multiple stages of oversight and governance is therefore inherently dangerous for patients,” it said.
In addition, the PDA said that the DHSC proposal could cause rotational pharmacist training in aseptic units to “diminish or disappear altogether”, reducing overall capacity in the system over time.
It said that the proposal could lead to “a total loss of pharmacist involvement in aseptic production”, which would mean that the “valuable dual-aspect (clinical and technical) unique knowledge and involvement of the pharmacist (especially in specialist wards such as cancer or paediatrics) may be lost forever”.
The PDA said that it would publish “a detailed organisational response” to the supervision consultation “in due course”.
In its supervision consultation response, the Association of Pharmacy Technicians UK (APTUK) agreed with the DHSC proposal to allow pharmacy technicians to be responsible for hospital aseptic facilities.
APTUK said that pharmacy technicians are increasingly “the most skilled and experienced pharmacy professionals in these units, safely providing vital services to some of the most vulnerable patients”.
It added that many pharmacy technicians practising in aseptic units “have extensive post-registration training and qualifications and are well placed to take this responsibility with the support of the correct framework”.
APTUK argued that the additional responsibility outlined in the DHSC proposal “would support development of pharmacy technician roles and career frameworks in aseptics, helping to encourage training, recruitment, and retention”.
Nathan Burley, president of the Guild of Healthcare Pharmacists, told The Pharmaceutical Journal that he believed that supervision of aseptic facilities “merits a more comprehensive consultation process” than the one that is ongoing.
“Hospital aseptic facilities benefit from technical and clinical knowledge and experience. Senior leadership, accountability and, importantly, continuity are paramount in this high-risk area.
“Any move that results in these being negatively impacted would not be supported,” Burley said.
The consultation closes on 29 February 2024.
1 comment
You must be logged in to post a comment.



The PDA position statement succinctly details the problems with proposal 3 in the current Pharmacy Supervision Consultation, and I have already submitted my response along similar lines. For too long, Schools of Pharmacy and Health Education England have held up Clinical Pharmacy and Pharmacist Prescribing as the holy grail to which all Pharmacists must aspire. This ignores pharmaceutics and formulation which distinguish Pharmacy from the other health care professions. Aseptic/Technical services within hospital Pharmacy practice is in itself a rewarding career path which for some Pharmacists (myself included for more than thirty years) have found professionally satisfying. Pharmacists are able to use their clinical knowledge to ensure the right product reaches the right patient at the right time, whilst ensuring patient safety and minimising the inherent risks with injectable medication - Clinical Pharmaceutics! Proposal 3 throws this on the bonfire in the unachievable pursuit of filling the work force gaps elsewhere within the NHS, and to mix metaphors, throws the baby out with the bath water!
Pharmacy Technician education/qualification no longer includes any element of Aseptic/Technical services, and this makes it dangerous to allow Technicians to have overall control of an Aseptic Unit with little or no oversight from an experienced Aseptic Services Pharmacist. Chief Pharmacists are too remote from the coal face, and most have little or no relevant Aseptic/Technical services experience.
Along with others, including the PDA, I call upon the Department of Health to withdraw proposal 3, and instead implement a separate and more in-depth and comprehensive review and consultation before deciding the merits or otherwise of changing the supervision requirements within Aseptic/Technical Services. I urge others to repsond similarly before the 29th February deadline.
I am also disappointed that the RPS doesn't appear to have sought the views of those practicing within Aseptic/Technical Services before agreeing to support proposal 3!
David Lovett, Retired Aseptic Services Pharmacist and a past Chair of the NHS Pharmaceutical Aseptic Services Group