UrbanImages / Alamy Stock Photo
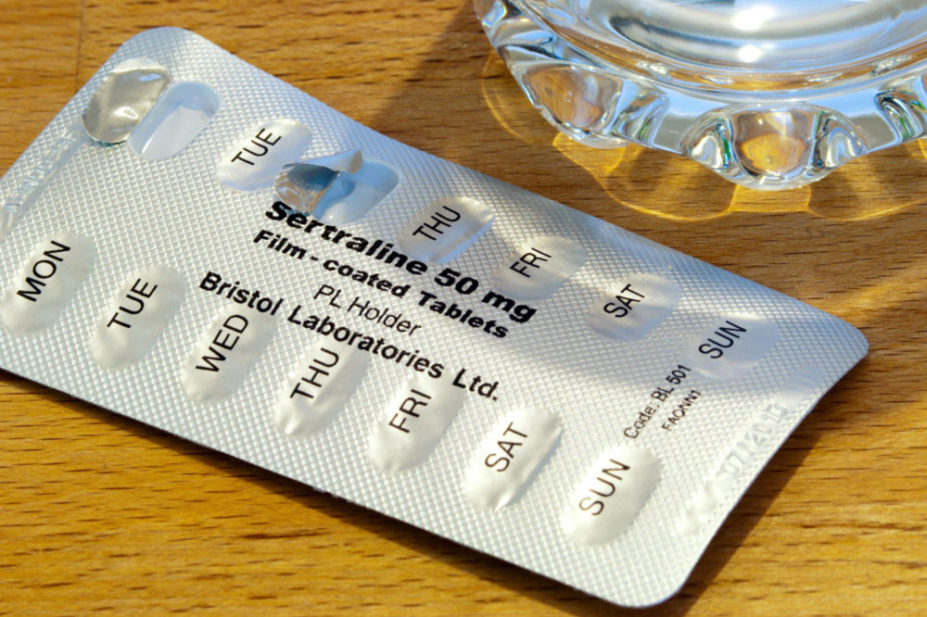
Adults with “less severe” depression should not be routinely offered antidepressants as a first-line treatment, draft guidance from the National Institute for Health and Care Excellence (NICE) has advised.
In its first new guideline on the management of depression in adults in 12 years, NICE divided its recommendations into two broad categories: adults with less severe depression and adults with more severe depression.
For people with less severe depression, the guidance recommends a variety of non-pharmacological options as first-line treatment, including cognitive behavioural therapy (CBT), exercise and psychotherapy. It states that, when choosing a first-line treatment, clinicians should move through the variety of different options until a shared decision is made with the patient as to which treatment should be tried first.
It also states that antidepressants should not be routinely offered as first-line treatment unless that is the patient’s preference.
In its rationale for the recommendation, the guideline committee said: “The evidence suggested that some psychological therapies were more effective than antidepressants, medication should not be the default treatment for people with less severe depression, unless it was the person’s preference to take antidepressants rather than engage in a psychological intervention.”
In contrast, for patients with “more severe” depression, which includes the categories of moderate and severe depression, the committee highlighted that there was “good evidence” for the effectiveness and cost-effectiveness of antidepressants, and for the effectiveness of CBT combined with antidepressants.
When prescribing antidepressants, the guidance states that patients should be given information about how they might be affected when they first start taking antidepressant medication, how some side effects may persist throughout treatment, and the withdrawal symptoms and how the effects can be minimised.
It also says that clinicians should explain to patients that, on stopping antidepressant medication, it was usually necessary to reduce the dose in stages over time; a process called “tapering”.
“As a committee, we have drawn up recommendations that we hope will have a real impact on people who are suffering from depression, and their carers,” said Nav Kapur, professor of psychiatry and population health at the University of Manchester and chair of the guideline committee.
“In particular, we’ve emphasised the role of patient choice — suggesting that practitioners should offer people a choice of evidence-based treatments and understanding that not every treatment will suit every person.”
Ciara Ni Dhubhlaing, president of the College of Mental Health Pharmacy, welcomed the amendments made in the draft guideline recommending a “more holistic” assessment and treatment according to individual patient needs, saying that it “more closely reflects good clinical care in practice”.
“The committee note that integrating the recommendations into consultations may be more time-consuming and therefore impact on NHS appointment times,” she added.
“It is a valid concern; however, the morbidity and mortality associated with depression is such that initiating the right combination of treatments and supports for individuals to reduce risk of relapse and reoccurrence is an investment in reduced need for NHS resources in the future.
“The guidance includes information and advice on stopping antidepressant medication. There is a clear role here for primary care pharmacists with expertise in mental health.”
The draft guideline consultation closes on 22 January 2022.
Read more: Prescribers should warn patients about dependence before starting them on high-risk drugs, says NICE
1 comment
You must be logged in to post a comment.



Informative and useful, confirms patient’s lived experiences and practical advice for professionals. Thanks PJ.