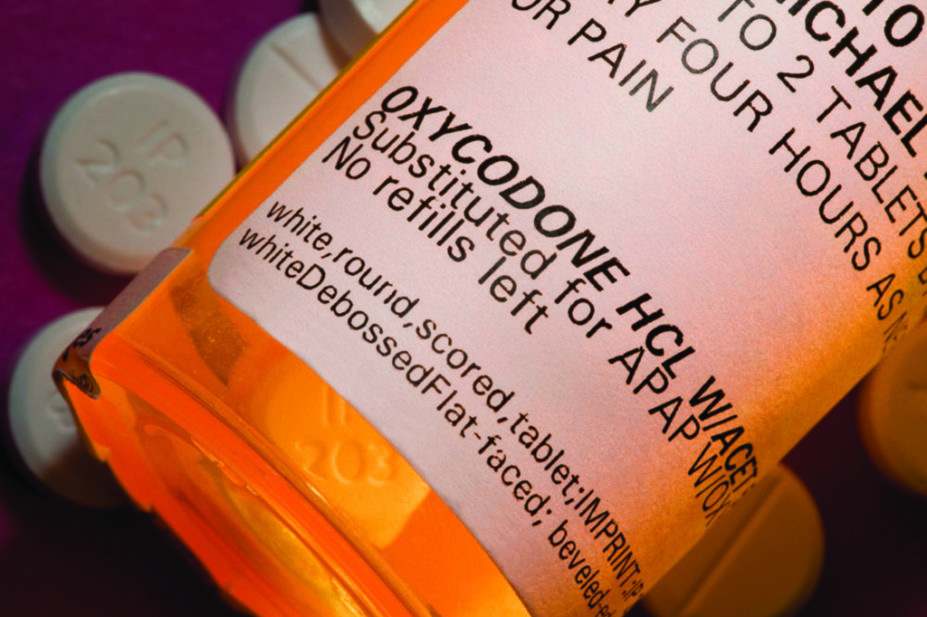
Michael Siluk/Alamy Stock Photo
Before starting treatment with antidepressants, opioids, benzodiazepines or other drugs associated with dependence, patients should be warned about how hard it may be to stop taking them, recommends draft guidance from the National Institute for Health and Care Excellence (NICE).
In the institute’s first ever guideline specifically concerning medicines that can cause dependence or withdrawal symptoms, NICE says that prescribers must offer patients all of the alternative options for treatment, such as non-pharmacological treatment and watchful waiting, before prescribing a high-risk medicine.
However, if pharmacological treatment is required, then patients should be adequately prepared with enough information about the risks of dependence and/or withdrawal, with prescribing perhaps delayed until after the first appointment “to allow time for the person to think about their options”.
The guidelines follow on from the publication of Public Health England’s 2019 evidence review, ‘Dependence and withdrawal associated with some prescribed medicines‘, which revealed that more than a quarter of the adult population in England (26.3%) had been prescribed a dependency-forming medicine in the previous year.
The NICE draft guideline, published on 22 October 2021, focuses on medicines usually used for conditions that are chronic, complex and difficult to treat, such as anxiety, insomnia, chronic pain and depression.
Historically, there have been few guidelines that focus on avoiding dependence and managing withdrawal from prescribed medicines.
The guidance states that prescribers should discuss withdrawing a medicine if the patient is no longer benefiting from treatment; if the patient has developed problems with dependency; if the condition for which the medication was prescribed has resolved; if the patient wants to stop; or if the harms of the medicine outweigh the benefits.
For opioids, benzodiazepines, Z-drugs and antidepressants, it recommends a “slow, stepwise rate of reduction proportionate to the existing dose — so that decrements become smaller as the dose is lowered”, and to ensure that the rate of reduction is likely to be tolerable for the individual.
For gabapentinoids, the guidance advises that prescribers reduce the dose by a fixed amount at each decrement.
If distressing symptoms occur after a dose reduction, it states that prescribers should consider delaying the next dose reduction.
“At all stages of prescribing and withdrawal management, aim to foster collaborative, trusting and supportive relationships with people taking an opioid, benzodiazepine, gabapentinoid, Z-drug or antidepressant,” the guidance says.
During the process of withdrawal, the guidance advises considering increasing the frequency of reviews and offering non-pharmacological therapies, such as group cognitive behavioural therapy, to support patients discontinuing benzodiazepines.
Paul Chrisp, director of the centre for guidelines at NICE, said that many people continue to be prescribed dependence-forming medicines, despite evidence that the risks outweigh their benefits.
“People are being harmed and we cannot ignore it,” he said. “Although these medicines can provide lasting symptom management for a proportion of people taking them, they do not work for everyone.
“Having the right strategy for withdrawing safely from these medicines is key, and that is why these evidence-based guideline recommendations are required to support healthcare professionals and patients.”
David Taylor, director of pharmacy and pathology at the Maudsley Hospital, London, and professor of psychopharmacology at King’s College London, welcomed the publication of the guidelines, which, “for perhaps the first time, formally recognise the dependence potential of antidepressants, Z-drugs and gabapentinoids”.
“The guidelines contain valuable information on patient education, duration of treatment and methods of withdrawal,” he said.
“Their publication should make prescribers more cautious about initiating these medicines and help patients stop them in a way that causes the least distress.”
On 19 October 2021, research from the Council for Evidence-Based Psychiatry and the All-Party Parliamentary Group (APPG) for Prescribed Drug Dependence, published in Addictive Behaviours, revealed the estimate that around £500m of taxpayer’s money was wasted each year in England on medicines that can cause dependency, including antidepressants, painkillers and sleeping pills.
“This research reveals that £500m of public money is being wasted on unnecessary prescriptions that, in many cases, also cause harm, with lives sometimes devastated by the impact of dependency and withdrawal,” said Danny Kruger, chair of the APPG for Prescribed Drug Dependence.
“The economic argument is now clear — a fraction of these wasted costs should now be invested in a helpline and dedicated withdrawal support services, as recommended by Public Health England back in 2019. This investment will benefit both public health and the public purse.”
The consultation on the guideline is open until 2 December 2021.
What the National Institute for Health and Care Excellence draft guideline says
Before starting treatment with an opioid, benzodiazepine, gabapentinoids, Z-drug or antidepressant, explain to the patient:
- The potential side effects;
- The additional implications of taking the medicine if the person is pregnant or planning pregnancy;
- What the options might be if the medicine does not work;
- How difficult it might be to stop the medicine later;
- The risks, signs and symptoms of developing dependence or tolerance if the medicine is an opioid, benzodiazepine, gabapentinoid or Z-drug;
- For antidepressants or gabapentinoids, that the effect of the medicine may occur slowly, they might experience side effects before noticing any benefits and that any side effects are likely to ease over time.
Source: NICE draft guideline, Medicines associated with dependence or withdrawal symptoms: safe prescribing and withdrawal management for adults. October 2021
You may also be interested in

Voice of the Voiceless: co-produced materials to help reduce stigma for people receiving opioid substitution treatment in pharmacies
PJ view: The government’s approach to illegal street drugs should focus on treatment and prevention
