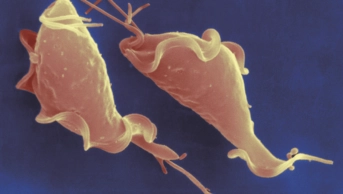
Shutterstock.com
Chlamydia testing in community pharmacies fell by 7% in 2019, despite a 2% overall increase in tests carried out through the National Chlamydia Screening Programme during the same year.
The data, published by Public Healh England (PHE) in ‘Sexually transmitted infections and screening for chlamydia in England, 2019’ on 2 September 2020, also revealed a 5% increase in sexually transmitted infections (STIs) overall.
Community pharmacies are able to screen for Chlamydia in sexually active young people aged 15–24 years through the locally commissioned National Chlamydia Screening Programme, which is also provided by specialist sexual health services, GPs and other healthcare providers.
Overall, 2% more young people were diagnosed with Chlamydia though the programme in 2019 compared with 2018, in line with the 2% increase in testing during that time.
But, according to the data, the number of tests carried out in pharmacies fell from 12,431 in 2018 to 11,598 in 2019. Of these tests, 1,295 patients were diagnosed with Chlamydia in 2019 — a 3% decrease on the year before.
Claire Anderson, chair of the Royal Pharmaceutical Society’s English Pharmacy Board, said community pharmacies are ”well placed to help patients with any questions and issues around sexual health”.
”We want commissioners to consider additional opportunities and clinical services for pharmacy teams, such as appropriate resources and support, so that they can continue to promote good sexual health and help prevent transmission,” she said
In March 2019, PHE similarly advised commissioners to recognise “the value of pharmacy” to provide better sexual health services to patients, adding that Chlamydia screening and treatment, sexual health promotion and providing information on HIV “are not consistently provided across the country”.
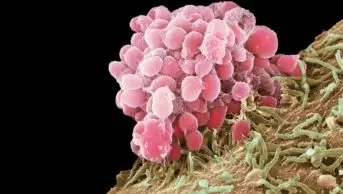
Overall, the report highlights a 5% increase in STI diagnoses from 447,522 in 2018 to 468,342 in 2019. This includes a 26% increase in gonorrhoea diagnoses, from 56,232 in 2018 to 70,936 in 2019, and a 10% increase in syphilis diagnoses, with 7,982 cases reported in 2019.
Ian Green, chief executive of Terrence Higgins Trust, said the overall statistics are “heading the wrong way”.
“There was a 2% increase in Chlamydia diagnoses among young people since 2018, despite a 13% decline in the number of tests since 2015. All of this underlines the need for urgent action,” he said
“The government has committed to a national sexual health strategy to improve the nation’s sexual health, which has been delayed by the COVID-19 pandemic. These new figures underline why this can’t be delayed any further — that includes the need for significant investment in public health to ensure sexual health services are accessible as lockdown continues to ease,” he continued.
However, PHE said that the overall rise in STIs is, in part, due to increased testing, more accurate diagnostic tests and “more comprehensive data” on STI diagnoses.
Hamish Mohammed, national lead for sexually transmitted infection surveillance at PHE, warned that gonorrhoea has become more resistant to antibiotics, and that PHE “expects to see further cases of antibiotic-resistant gonorrhoea in the future, which will be challenging for healthcare professionals to manage”.
He added that “consistent and correct use of condoms with new and casual sexual partners is the best defence against all STIs”.