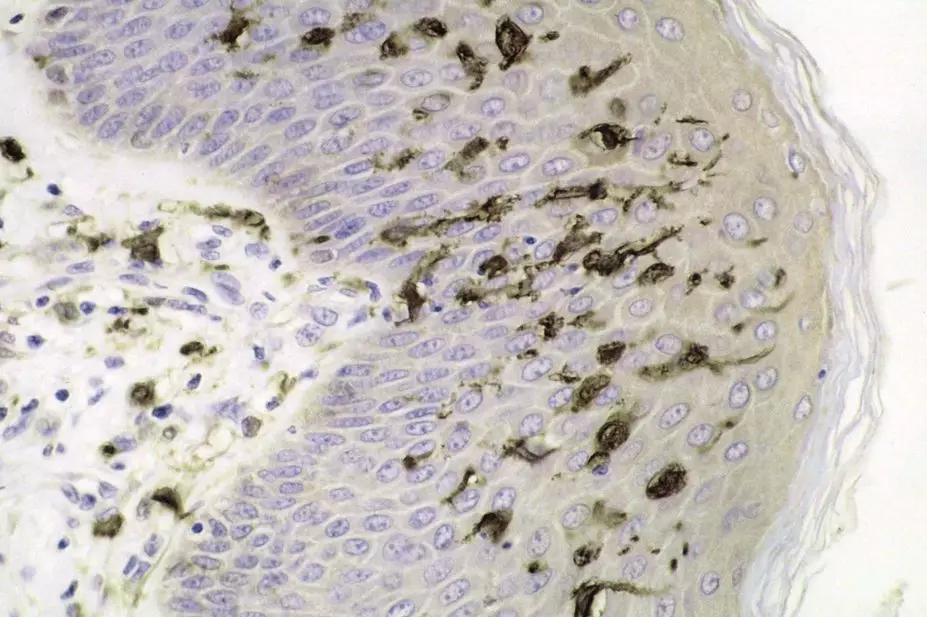
Haymanj / Wikimedia Commons
A single injection of a patient’s own modified dendritic cells appears to safely deliver anti-inflammatory and immunoregulatory effects for rheumatoid arthritis (RA), a phase I study has shown.
The therapy, Rheumavax, is a personalised immunotherapy approach in which patients’ own dendritic cells — antigen-displaying immune cells that regulate immune tolerance — are used as a vehicle for citrullinated peptides.
Autoantibodies to anti-citrullinated peptides (ACPA) are found in approximately 70% of patients with RA. They are strongly associated with the HLA-DRB1 risk alleles and are known to activate the immune system during cell death or inflammation.
Researchers led by Helen Benham, from the University of Queensland, Australia, now report findings from a first-in-human study involving Rheumavax.
They first obtained blood samples from 18 patients with HLA-positive RA, extracted dendritic cells and treated with a nuclear factor kB (NF-kB) inhibitor that had been exposed to four citrullinated peptide antigens. The modified autologous dendritic cells were then reintroduced to the patients via a single, intradermal injection at one of two doses.
Writing in Science Translational Medicine
[1]
, Benham’s group reports that Rheumavax was well tolerated and did not induce flares in patients with minimal disease activity.
One month after treatment, patients given Rheumavax showed markedly reduced levels of activated T-cells and proinflammatory molecules in the blood relative to a control group of 16 untreated RA patients. Furthermore, Rheumavax-treated patients with active RA showed a significant reduction in disease activity, as indicated by the Disease Activity Score in 28 joints (DAS28) at one month.
Ranjeny Thomas, the study’s senior author, also from the University of Queensland, concedes that the technique used to develop Rheumavax is unlikely to be widely adopted due to its cost and time demands. However, he notes: “The promising results of this trial lay the foundations for the development of a most cost-effective, clinically-practical vaccine technology that could deliver similar outcomes for patients.”
Natalie Carter, head of research liaison and evaluation at Arthritis Research UK, is enthusiastic about the results. “This treatment acts to re-educate the immune system so that it recognises healthy tissue, stopping the vicious cycle of joint inflammation and damage,” she says. Her group is funding trials of a similar immunotherapy, but was not involved in this study. “This is particularly exciting as it is not simply a way to treat symptoms but to stop RA in its tracks,” she adds. Carter says more research is needed into the treatment.


