Shutterstock.com
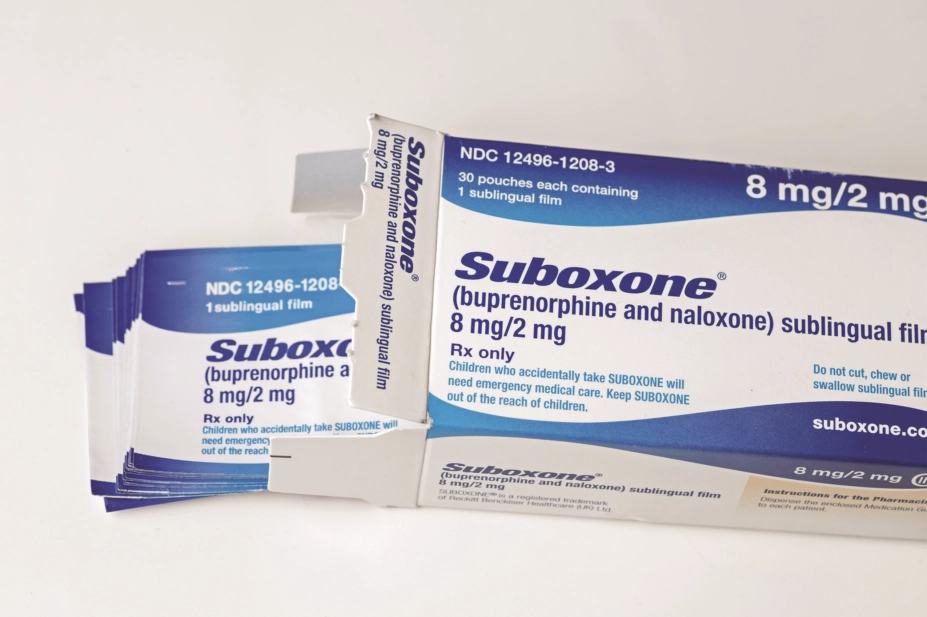
The US Food and Drug Administration (FDA) plans to encourage greater use of what it regards as less harmful opioid drugs such as methadone and buprenorphine to manage addiction to prescription opioids in a radical shift in policy.
FDA Commissioner Scott Gottlieb said that the FDA will be investing in a series of measures both to prevent new addictions and treat existing ones, which he admitted may make some in the addiction field, who believe abstinence is the only effective treatment, “uncomfortable”.
The announcement came as President Trump declared the US opioid crisis a “public health emergency”.
Measures to prevent new addiction could include steps such as restrictions on prescribing, mandatory education for healthcare professionals, and recommending that certain products be withdrawn from the market. Gottlieb said the FDA may also promote “the development of new, less addictive pain remedies, as well as opioids that are harder to manipulate and abuse”.
“But given the scale of the epidemic, with millions of Americans already affected, prevention is not enough,” he added.
“We must also help those who are suffering from addiction by expanding access to lifesaving treatment.”
Gottlieb said the FDA would promote the development of new addiction treatments and the more widespread use of existing FDA-approved therapies to help combat addiction. All of these treatments work in combination with counselling and psychosocial support.
Recently, the Commonwealth of Massachusetts found that patients treated with methadone or buprenorphine after a non-fatal overdose had a greater than 50% reduction in the risk of death from a subsequent overdose, he said. “So one concept the FDA is actively pursuing is the research necessary to support a label indication for medication-assisted treatment for everyone who presents with an overdose.”

Courtesy of Roger Knaggs
Roger Knaggs, associate professor in clinical pharmacy practice at the University of Nottingham and Royal Pharmaceutical Society spokesperson on pain, said that the UK and other European countries had seen an increase in opioid prescribing, but not the associated rise in mortality seen in the United States.
Roger Knaggs, associate professor in clinical pharmacy practice at the University of Nottingham and the Royal Pharmaceutical Society spokesperson on pain, said that while the UK and other European countries had seen an increase in opioid prescribing, unlike the United States they had not seen a similar rise in mortality associated with that prescription.
“There are a myriad of reasons for the differences in mortality between the US and Europe that have been proposed, including differences in the healthcare structure and funding, and provision of services for people with persistent pain,” he said.
“Methadone and buprenorphine have been used for a long time in the management of opioid addiction and there is already good access to these medicines through substance misuse services in the UK. However, they have a smaller role to play for patients who misuse prescription opioids and their use does require specialist knowledge and experience.”


