Alamy
Monoclonal antibodies designed to lower cholesterol by inhibiting proprotein convertase subtilisin/kexin type 9 (PCSK9) are effective and associated with few major side effects, suggests research published in the Annals of Internal Medicine
[1]
on 28 April 2015.
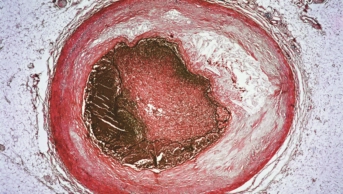
The systematic review and meta-analysis of 24 randomised controlled trials (RCTs) found that monoclonal antibodies against PCSK9 bring about profound reductions in low-density lipoprotein (LDL) cholesterol as well as reducing cardiovascular endpoints and all-cause mortality.
PCSK9 is an enzyme involved in lipid metabolism. PCSK9 antibodies prevent circulating PCSK9 from binding to the low-density lipoprotein receptor (LDLR) on the surface of liver cells, thereby preventing PCSK9-mediated LDLR degradation and leading to reductions in serum LDL-cholesterol.
Three PCSK9 monoclonal antibodies are in late-stage clinical development. Amgen/Astellas’s evolocumab (Repatha) and Sanofi/Regeneron’s alirocumab (Praluent) are expected to be approved in late 2015 or early 2016 for the treatment of hypercholesterolaemia, and Pfizer’s bococizumab is currently in phase III trials.
To evaluate the available evidence, Eliano Pio Navarese, from Heinrich Heine University, Düsseldorf, Germany, and colleagues identified 24 phase II and phase III RCTs involving 10,159 adult patients treated with PCSK9 antibodies (evolocumab, alirocumab or bococizumab).
Compared with no PCSK9 antibodies, treatment with a PCSK9 antibody led to a significant reduction in LDL-cholesterol levels (mean difference –47.49%, 95% confidence interval [CI] –69.64% to –25.35%; P<0.001).
PCSK9 antibodies also significantly reduced all-cause mortality (odds ratio [OR] 0.45, CI 0.23 to 0.86; P≤0.015), cardiovascular mortality (OR 0.50, CI 0.23 to 1.10; P≤0.084) and myocardial infarction (OR 0.49, CI 0.26 to 0.93; P≤0.030). This is the first large-scale report to show a mortality benefit with these agents, the authors remark.
The frequency of serious adverse events was not increased with PCSK9 antibodies compared with controls. Also, of potential relevance to patients who are unable to tolerate a statin, treatment with PCSK9 antibodies resulted in a statistically significant reduction in serum creatine kinase levels.
The researchers say that the reduction in all-cause and cardiovascular mortality associated with PCSK9 antibodies is consistent with the observed 50% reduction in LDL-cholesterol. However, they note that the trials they analysed were not powered to assess hard endpoints and results of four ongoing trials — due to report in 2018 — will be needed to confirm this.
“Ongoing trials should provide further data on the safety of this innovative strategy and on the relationship of lower LDL cholesterol levels and the rate of cardiovascular events,” the researchers write. “In particular, these trials should validate or refute the findings on mortality that, if confirmed, could have a profound effect on public health.”
Peter Weissberg, medical director at the British Heart Foundation and not involved in the research, says the results are promising but need to be considered cautiously. “Longer term information on more patients will be needed to confirm that PCSK9 inhibitors do save lives with no serious long-term adverse effects before their use is likely to be approved for patients, other than those at high risk with dangerously high cholesterol levels despite statin treatment,” he says.