Shutterstock.com
The government has launched an independent review to investigate potential bias in the design of medical devices and the impact this has on patients from different ethnic groups.
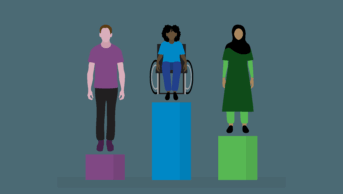
In a statement on 21 November 2021, the Department of Health and Social Care (DHSC) said the review follows concerns that the way medical devices are designed and used “could mean a patient’s diagnosis and treatment is affected by their gender or ethnic background”, exacerbating existing health inequalities.
The UK-wide rapid review is expected to lead to recommendations on how any biases should be mitigated when developing medical devices.
Current UK regulations do not include provisions to ensure that medical devices are equally effective, regardless of demographic factors, such as ethnicity.
For example, the government’s statement highlighted research which concluded that pulse oximeters — used to measure oxygen levels — were less accurate for patients with darker skin owing to a tendency for this group to present with higher levels of oxygen in the blood.
In April 2021, the NHS Race and Health Observatory (NHS RHO) called for a review of pulse oximeters, after an analysis by Michigan University in the United States found that pulse oximeter readings of blood oxygen levels were three times more likely to be inaccurate among African-American patients, adding that most oximeters “have been developed based on studies measuring oxygen levels in Caucasian and light-skinned individuals”.
While appearing on the BBC’s The Andrew Marr Show on 21 November 2021, UK health secretary Sajid Javid was asked whether he thought people had died from COVID-19 as a result of racial bias in medical devices, to which he responded: “I think possibly, yes.”
“These oximeters are being used across every country and they all have the same problem, and the reason is that a lot of these medical devices, or even some of the drugs, the procedures and some of the textbooks — most of them are put together in majority-white countries,” he said.
“This is a systemic issue and I’ve discovered this really through taking a real interest in disparities and wanting to know, for example, why, during the height of this pandemic, a third of people in ICU [intensive care units] with COVID-19 were from black and minority ethnic backgrounds — double the representation in the general population.”
MRI scanners — which are still not recommended for use for pregnant or breastfeeding women — will also be included in the review to determine how to expand the scope of the equipment’s use.
The DHSC would not respond to requests for further information on the review but said all medical devices will be looked at to identify potential discrepancies in how they work for different ethnic groups.
Elsy Gomez Campos, workforce, equality, diversity and inclusion lead at Kent Community Health NHS Foundation Trust and president of the UK Black Pharmacist Association, said it was “worrying” that health inequalities could result from the design and use of medical devices and technologies.
“Everyone should receive a high quality of healthcare, regardless of their gender and ethnicity,” she said.
“I, therefore, welcome the announced independent review by the DHSC. The review is a positive step towards ensuring health outcomes, systems and related technologies are bias-free.”
Mahendra Patel, honorary visiting professor at the University of Bradford, University of Sussex and Birmingham City University, said the review was “certainly not before time” as research has highlighted “for many years” inaccuracies in readings when measuring oxygen levels in ethnic minority communities.
“What’s also worrying is that these racial disparities extend beyond medical devices,” he added.
“In dermatology, for example, skin diseases such as eczema, psoriasis [and] acne can manifestly appear differently in darker-skinned people compared to white skin and can lead to misdiagnosis.”
Patel said that a “dedicated and targeted” commitment for more culturally inclusive research and data on people with darker skin was “urgently needed” to help address some of these unacceptable disparities.
“Furthermore, training and learning at undergraduate level within medical, dental, nursing and pharmacy professions has to be more inclusive in terms of images and disease states of people with darker skin if we are to truly understand and clinically treat people of colour equally and more successfully.”
The Pharmaceutical Journal revealed in November 2021 that 24 of the 28 pharmacy schools in the UK are committed to ‘decolonising’ their MPharm degree curriculums to make them more racially inclusive, with planned changes including additional learning on health inequalities and race, cultural competence and revising modules on dermatological conditions to incorporate a wider range of skin tones.
Initial findings from the DHSC’s review are expected to be presented by the end of January 2022.
Read more: Recognising common skin conditions in people of colour

Health inequalities
The Royal Pharmaceutical Society’s policy on health inequalities was drawn up in January 2023 following a presentation by Michael Marmot, director of the Institute for Health Equity, at the RPS annual conference in November 2022. The presentation highlighted the stark health inequalities across Britain.
While community pharmacies are most frequently located in areas of high deprivation, people living in these areas do not access the full range of services that are available. To mitigate this, the policy calls on pharmacies to not only think about the services it provides but also how it provides them by considering three actions:
- Deepening understanding of health inequalities
- This means developing an insight into the demographics of the population served by pharmacies using population health statistics and by engaging with patients directly through local community or faith groups.
- Understanding and improving pharmacy culture
- This calls on the whole pharmacy team to create a welcoming culture for all patients, empowering them to take an active role in their own care, and improving communication skills within the team and with patients.
- Improving structural barriers
- This calls for improving accessibility of patient information resources and incorporating health inequalities into pharmacy training and education to tackle wider barriers to care.