Over the past few years, the number of patients attending Mount Vernon Hospital (MVH) for chemotherapy in an outpatient setting has increased. Reasons for this include:
- an increase in the number of patients being diagnosed early as a result of self examination and improved screening (“Health of the Nation” initiatives)
changes in treatment strategies, in particular an increasing use of adjuvant and neo-adjuvant chemotherapy
advances in drug delivery systems, eg, multiday infusors, which has allowed more patients to be treated in their homes rather than having to be admitted into hospital
an increased usage of drugs which could be administered over shorter periods, e.g. carboplatin and raltitrexed - a new haematology /lymphoma consultant was appointed and more complex regimens were being used
These developments led to an overall increase in the workload within the outpatient chemotherapy suite leading to an increase in waiting times. Consequently a chemotherapy quality improvement team (QIT) was set up to improve workflow through the chemotherapy suite. It consists of pharmacists (including a Baxter Healthcare pharmacist), consultants, nurses and the business manager of the cancer directorate. The team meets regularly to identify ways in which the service provided to chemotherapy outpatients can be improved.
The old system
The chemotherapy suite (CHS)
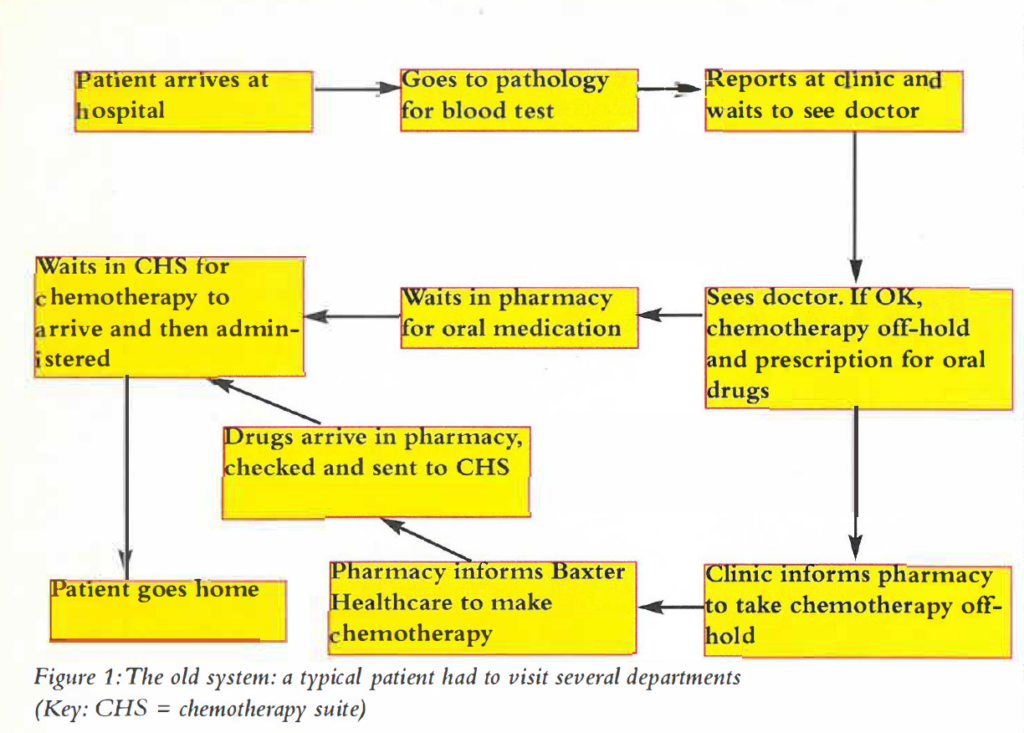
Previously a patient attending the chemotherapy suite would have had to visit several departments. The various stages are illustrated in Figure 1.
The pharmacy service
The original service was dispensary based. It consisted of screening chemotherapy orders. At MVH, all intravenous cytotoxic drugs were prepared on site by Baxter Healthcare. Chemotherapy was ordered in advance on a special order form (C-form) and the doses were based on the patient’s body surface area, i.e., patient specific. The order was a provisional order and said to be “on-hold”. On treatment day, the patient was assessed by the clinician and, if chemotherapy was to continue as planned, it was taken “off-hold”[1,2]. The time from “off-hold” to providing drugs was one hour.
The role of the pharmacists was to liaise between the wards/ doctors and Baxter Healthcare. In addition, pharmacists were involved in the traditional role of dispensing supportive treatments for example, antiemetics, and counselling chemotherapy outpatients at the pharmacy hatch.
Weaknesses of the old system
These can be considered under patient-oriented and workload issues.
Patient-oriented
A visit to the hospital as a chemotherapy outpatient involved going to several departments. As a result, patients often spent the whole day waiting to be treated.
In addition, different doctors often saw patients at different cycles, which could result in discrepancies in the drugs prescribed. For example, a patient who had not experienced any problems with previous medication could have different or new anti-emetics prescribed. This caused confusion for the patient, and led to interventions being made after the dispensing process.
Workload issues
Ideally, all chemotherapy should be ordered in advance, to minimise patient waiting times, and also to plan work within the pharmacy and at Baxter Healthcare[1,2]. In practice, with the increasing number of patients, this was not happening and resulted in late orders on the day of treatment.
Another problem was that the one-hour target from “off-hold” to availability of drugs was not being met. This contributed to an overall increase in patient waiting times.
The new system
Several measures were taken in an attempt to address the issues raised above and they are listed below.
Changes made in the CHS
- Installation of a blood analysis machine in the CHS, which provides a total blood count within one minute
- Implementation of protocol guidelines, enabling nurse practitioners to assess the patient and, based on the full blood count, take selected regimens off-hold before the patient sees the doctor
- For certain regimens, the patient is not always required to be seen by the doctor at every visit
- Doctors seeing patients in the CHS and patient notes being kept in the CHS
- Direct link between CHS and pharmacy via pneumatic tube system
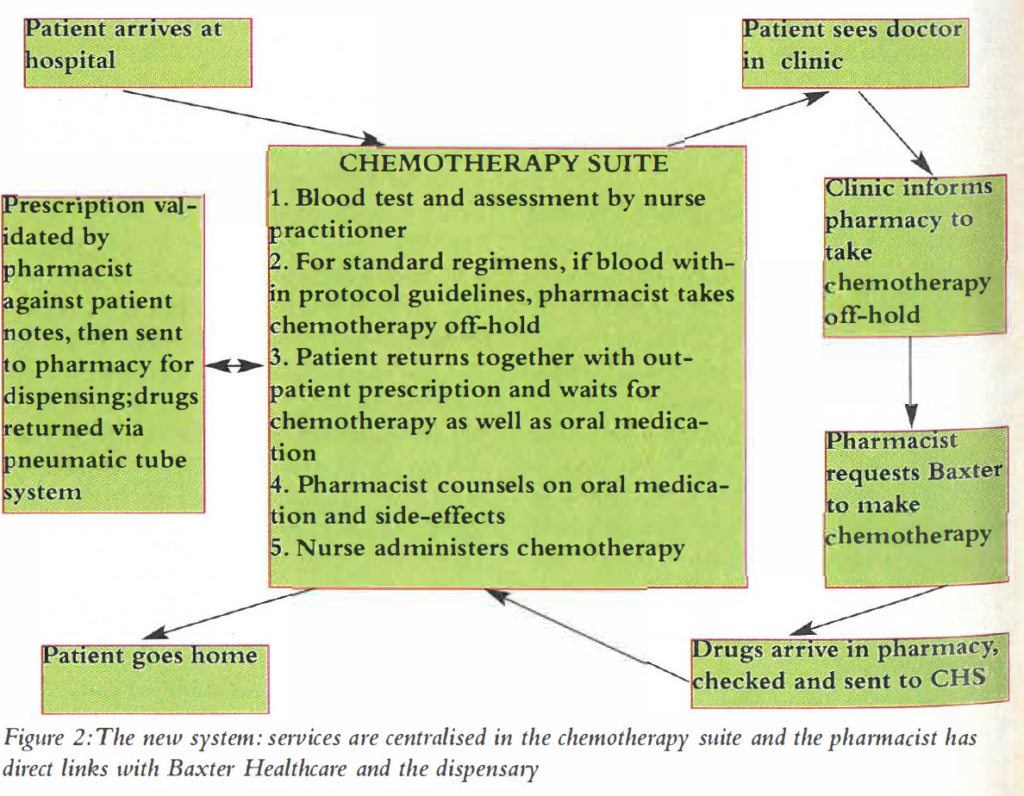
The result of these measures was to centralise the service provided in the CHS. These changes in the CHS, together with an increase in workload and complexity of chemotherapy, made it necessary to review the provision of pharmacy services.
It was perceived that the presence of a pharmacist in the CHS would further improve patient care and the quality of pharmacy service provided. The pharmacist based in the CHS has direct links to the dispensary (via pneumatic tube system, telephone and computer system) and Baxter Healthcare (via telephone and fax machine). This is shown in Figure 2.
Changes to pharmacy services
Clinical screening of out-patient chemotherapy at the decision making stage
The pharmacist is in a position to identify and anticipate potential dose changes due to low blood counts, abnormal biochemistry results, changes in body surface area, or uncontrolled side effects.
Patients are asked to bring their outpatient prescription to CHS, rather than taking it to the pharmacy, so that the pharmacist, who is based in the CHS, can clinically evaluate the prescriptions using medical notes, and thus intervene before the dispensing process.
Counselling
The presence of the pneumatic tube system has allowed dispensed drugs to be sent to the CHS where the patient can be counselled by the chemotherapy pharmacist in relation to chemotherapy timings and other medication. Potential drug interactions are often identified at this stage, eg, concomitant use of methotrexate and overthe-counter NSAIDS. In addition, the patient-pharmacist relationship has improved. The pharmacist is a recognised and easily accessible source of information on drug-related inquiries for the patient.
Repeat prescription sheets and prepacks of oral medication
Standard anti-emetics were proposed for selected regimens to reduce the problems associated with seeing different doctors. Repeat prescription sheets that can be used for the entire treatment course were introduced to facilitate this. These sheets are kept in the medical notes, and act as a record of all the oral medication prescribed for the patient. They also ensure continuity of care for the patient. The appropriate drugs are prepacked, pre-labelled and stored m a designated cupboard in the CHS. The chemotherapy pharmacist dispenses from this supply.
Co-ordinating the ordering of chemotherapy
One way of reducing late orders was to order the entire course of treatment in advance, rather than one cycle at a time. Together with Baxter Healthcare, a repeat C-form was designed for this purpose.
The presence of a pharmacist in the CHS has improved communication between clinics, CHS and pharmacy. In addition, the CHS pharmacist can take drugs off-hold directly from the CHS, provided blood results are within protocol guidelines.
Prefilled syringes
The QIT proposed the introduction of prefilled syringes in the CHS in an attempt to overcome the one hour lag-time from “off-hold” to availability of drugs. In order to use prefilled syringes, a number of standard dosages must be prescribed. A retrospective study was carried out over a period of six months to look at the doses used, in relation to body surface area, for one of the simpler regimens. The study was carried out by looking at the CMF regimen for breast cancer:
- Cyclophosphamide orally on days 1 to 14 ( or rarely, IV days 1 and 8)
- Methotrexate IV days 1 and 8
- 5-fluorouracil IV days 1 and 8
This is repeated every four weeks. The doctor sees the patient on day 1 of each cycle, and all the necessary drugs (oral and IV), for the entire cycle, are prescribed. On day 8, the patient attends for a full blood count. Provided this is within protocol guidelines and there are no complications or problems, the patient is treated without having to see a doctor.
Variations in dosage used for a specific surface area were noted, depending on the prescriber’s preference for rounding doses up or down. This data was used to propose standard doses for a range of surface areas, and presented to consultants for comment.
The consultants all agreed to prescribe the CMF (cyclophosphamide, methotrexate, 5-fluorouracil) chemotherapy within the proposed standard dosage guidelines for all new patients.
Syringes of the appropriate drugs were then ordered in advance and stored in the CHS, where the chemotherapy pharmacist dispensed them after checking blood results.
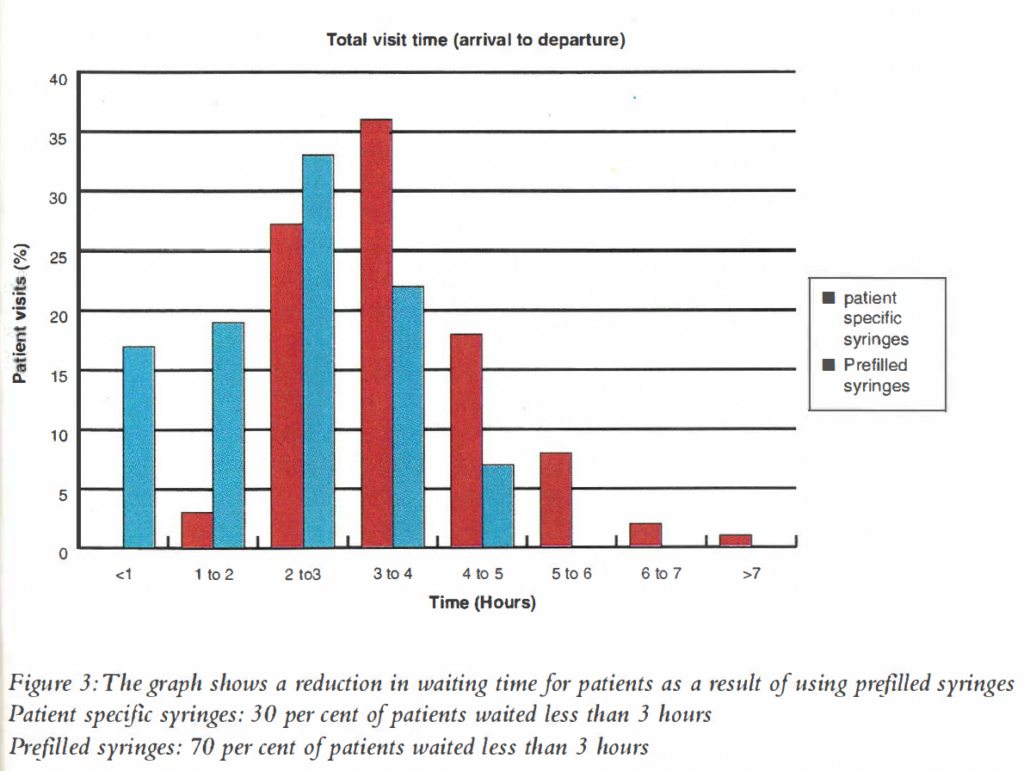
The use of pre-filled syringes has led to a significant reduction in the length of waiting times for this group of patients (Figure 3).
Conclusion
The development of the pharmacy service, together with changes in the CHS, have improved the quality of patient care, and streamlined the throughput of chemotherapy outpatients.
The presence of a pharmacist in the chemotherapy suite has been well received by doctors, nurses and patients. The pharmacist is a valuable member of a team consisting of different healthcare professionals, and has an active role in the management of drug therapy for cancer patients.
It was recently suggested that the NHS reforms and the Calman-Hine report on the future of cancer services have largely bypassed the pharmacy profession[3]. In this article we have described an active, patient-focused approach in the provision of pharmacy services for this group of patients.
Acknowledgements
We would like to thank Joan Ashby, pharmacy manager, Kay Bell, senior nurse, cancer centre, and the staff in the chemotherapy suite for their help and support.
References
- Ashby J. A collaborative venture in cytotoxic reconstitution, past, present and future.Pharm J 1988;240:HS 34-6.
- Ashby J. Cytotoxic reconstitution at Mount Vernon – the joint venture continues. Ibid 1992;249:HS 39-41.
- Adapting to the demands of patient focused care. Hosp Pharm 1998;5:56.