Courtesy of The Pharmacy Group, Wakefield Trinity
It was two years ago that we started running a needle exchange service from our community pharmacy in Wakefield, West Yorkshire.
The service has been a real success; it took off quickly and we are now seeing a significant number of patients for needle exchange alongside around 15–20 supervisions each week and at least 50 clients on instalment, or ‘blue’, prescriptions for methadone, although numbers haven’t yet returned to pre-COVID-19 levels.
Over this time, we have developed a good relationship with our clients; they appreciate the service, particularly as we are the only pharmacy in Wakefield City Centre that provides it.
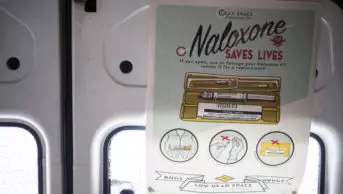
It was because of this success that we were approached in May 2020 by Turning Point, an organisation providing healthcare and social care services across England, to start providing the ‘Take Home Naloxone’ service alongside our existing substance misuse services. The service involves members of the pharmacy team supplying naloxone injections to people either at risk of having, or who might witness someone having, an opioid-related overdose, so that the injection can be administered during an emergency.
In Wakefield, I hear lots of stories about overdoses. In many cases, people are left standing there, helpless, watching someone they know overdose, unable to do anything about it. The COVID-19 pandemic has only made this situation worse by forcing people to isolate in their homes. However, we know that providing a take-home naloxone kit can save lives.
From the very beginning I explained to my team that, in order for the service to work, it would need to be a team effort; it is not a service that can be run by a solo pharmacist.
Owing to the fact that we were already providing needle exchange, it wasn’t too much of a stretch to start offering the naloxone kits during needle exchange transactions. We have had to make adjustments to the branch, although this was mostly prior to providing the needle exchange service and also because of the pandemic; for example, we’ve massively scaled back stockholding in the branch and there’s no self-selection available in the branch to avoid items getting stolen.
When we first started providing the kit we experienced a bit of defensiveness from our clients but, thankfully, no one has ever been horrified to be offered it, or been offensive to the team as a result.
It’s not our job to judge, it’s our job to get on with it
Once we got the first few kits out and word got around, we started getting positive feedback and were getting people coming in and asking whether we provided it. Sometimes people never want it and that’s fine, but we also get quite a few people that come in on repeat because they have lots of friends that have overdosed.
After a month of providing the service, we felt we had got it down to quite a fine art. We have it up on the counter and, when we see a client that we know might benefit from having a kit, we simply hold it up and ask “have you got one of these?”
Some will say they already have one from Turning Point, while others will occasionally say “no, what’s that?”, and we can then take the opportunity to explain what it is. Quite a few of them know what they are and will either ask for one or say “no, but I’ll bear it in mind”.
Overall, it’s a really quick transaction at the counter; I certainly wouldn’t be recommending that anyone does it in the consultation room. Ultimately, if you’re not happy with that situation and you want a private room, then we simply aren’t the pharmacy for you. So far, we have not been turned down by any clients because of that — they’re all happy to do it at the desk and go quickly in and out.
The biggest challenge we’ve had to overcome is making sure we had a smooth process as a team; all the team know what they’re doing so they can lead if I’m not here. There are still certain members of the team that don’t believe in substance misuse treatment but, despite this, they still step up and do the transactions; it’s not our job to judge, it’s our job to get on with it.
Before we started providing the service we were advised that there was a monthly budget across the area for naloxone. This meant that we would be expected to do between 20 and 25 interventions a month and I find that’s quite a comfortable target. In fact, of the 300 take-home naloxone kits distributed by community pharmacies in two areas of England over the past year, as part of Turning Point’s pilot project, over two-thirds were provided by our pharmacy.
Some clients were initially quite worried about getting stopped by the police with the kit on them but we try to reassure them that this is not about putting an ‘X’ on their back; it’s a good responsible thing to be doing if you’re living a particular lifestyle.
I’ve said to a few of them, you don’t want to be standing there when someone’s having an overdose thinking: “I can’t do anything.”
Now, we get clients coming in, sometimes together, and they’ll say to a member of their peer group: “You need one of these.” We’ve tried to encourage the fact that anyone can come in for it, whether it be a relative or a friend or whoever.
Nicola Torr is branch pharmacist at The Pharmacy Group, Wakefield Trinity
Read more: Pharmacy is the ‘logical place’ to provide naloxone kits, says Community Pharmacy Wales