TomBham / Alamy
Providing adequate healthcare to those who need it is a massive challenge for any region or country. In many places worldwide, public healthcare providers are struggling to meet the needs of patients, and the demands of an ageing and increasingly morbid populace will only set to put further pressure on healthcare systems. The strain is already starting to affect patients. In the UK, waiting times are getting longer and costs are rising[1]
.
Although the demand for treatment is increasing, not all the tests conducted, treatments initiated or surgical procedures performed are necessary, appropriate or beneficial. In fact, one estimate puts up to 20% of healthcare to offer little or no benefit[2]
. Fear of uncertainty and death by patients and clinicians is one of the proposed reasons for some of this extensive overuse in healthcare[3]
.
Many factors contribute further to a culture of excessive testing and treatment. These include: limited time in a busy environment; organisational and financial incentives towards risk aversion rather than risk management; inadequate training so that clinicians can address the issues of waste and overuse and have an informed discussion with their patient; easy access to testing; and defensive practice because of fear of litigation[3],
[4]
.
Waste in healthcare exists across professions, specialties and sectors. For example, 5.5% of hospital admissions, 14% of hysterectomies and 10–20% of antibiotics prescribed for upper respiratory tract infections are unnecessary and could be avoided[5]
. This is just the tip of the iceberg. With every medical intervention there is a price to pay beyond financial costs.
We have joined an international ‘Choosing wisely’ campaign that is challenging the belief of “more is better”. It was initiated in 2012 by the American Board of Internal Medicine Foundation (ABIMF) in collaboration with Consumer Reports, an independent consumer organisation. The Academy of Medical Royal Colleges (AoMRC) is now leading the UK leg of the campaign and the aim is simple: to initiate a conversation between patients and the public about the value of treatments and to tackle overuse.
Unnecessary tests and medicines
All medicines come with the risk of side effects. Tests and procedures can be painful and distressing to the patient and his or her family. Minor inexpensive interventions, while offering little or no benefit to the patient, can lead to adverse effects and have a financial and environmental cost. The cost of unused prescription medicines in the UK alone was estimated to reach £300m in 2010, and half of this sum is potentially avoidable[6]
.
In an era of an under supply of healthcare, as highlighted in NHS England’s ‘Five year forward view’, it is important to minimise these low-value, wasteful interventions and free resources so that they can be used in high-value, effective interventions and invested in research and innovation[7]
. By reducing unnecessary elective procedures and medication, the NHS could gain financial savings of up to £1.8bn each year, which could be used to support essential services[8]
.
We need to address overuse in healthcare, and move away from a culture of “more is better” to offering optimal care for every patient.
Choosing wisely
The ‘Choosing wisely’ international initiative brought attention, for the first time, to tests, procedures and interventions that are not well supported by evidence and are of questionable value.
The initiative’s main aim was to bridge the gap between professional responsibility to act as a steward of resources and actual physician behaviour, as highlighted by researchers at Massachusetts General Hospital, Institute for Health Policy, Boston[9]
. In a 2007 survey in the United States, although the majority of physicians were in agreement with the principles of waste and stewardship, 36% reported that they would order an unnecessary test to accommodate a patient who wanted it badly[10]
.
To change this behaviour the ABIMF, through ‘Choosing wisely’, invited professional societies to review their clinical practice and produce a list of the ‘Top five things physicians and patients should question’. So far, 70 medical and other clinical professional societies have participated in the United States and nearly 400 recommendations were produced.
The campaign in the United States is estimated to have reached 375,000 physicians and, in a recent survey, one in five physicians are aware of the campaign[11]
. In addition, those who were unaware of the initiative were more likely to offer unnecessary tests and procedures to their patients[11]
.
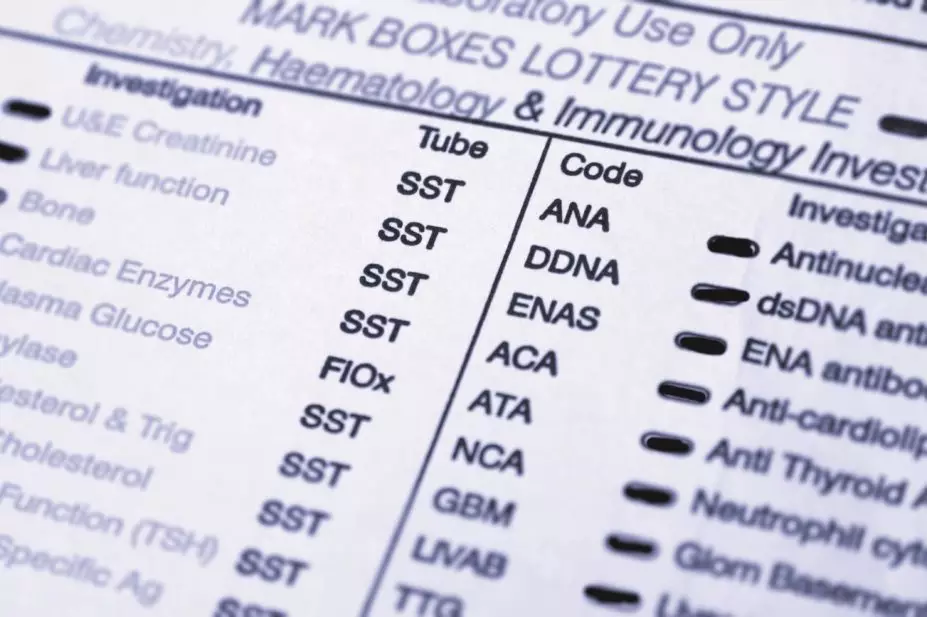
Studies are currently under way to measure the large-scale effect of the campaign in reducing the number of unnecessary interventions in the United States, specifically measuring the effect on magnetic resonance images requested for lower back pain, routine chest X-rays on admission and antibiotics for upper respiratory tract infections. Quality improvement projects inspired by ‘Choosing wisely’ have already led to significant results, with one medical centre in Washington state reducing antibiotics prescribed inappropriately for upper respiratory tract infection by 50%[12]
.
Since 2012, ‘Choosing wisely’ has spread around the world and inspired multiple similar campaigns, with Canada, Italy, Switzerland and the Netherlands launching similar campaigns. In Canada, within just one year of the campaign’s launch, 45 specialty societies have joined the campaign, representing 71,000 of the 77,000 physicians in Canada (92%)[13]
. In addition, more than 40 providers are now participating in the campaign’s Early Adoption Scheme, putting the recommendations into practice at a local level[11]
. One participating hospital in Ontario has reduced laboratory testing in the emergency department by 40% without any observable change in outcomes[14]
.
Several other countries around the world are also planning their own campaigns, including France, Austria, South Korea and New Zealand, and an international working group has been established to share experience and ideas between different countries[12]
. Now, the time has come for a similar initiative in the NHS in the UK. Bringing together multiple organisations across healthcare, such as medical royal colleges, NHS England, the National Institute for Health and Care Excellence (UK health technology appraiser), National Voices (a coalition of health and social care charities in England formed in 2008), patient lay groups, NHS Confederation and The BMJ, the academy is leading the ‘Choosing wisely’ initiative in the UK.
Taking action
In the coming months, AoMRC will ask its 21 member royal colleges and faculties to begin an audit across different areas of clinical practice, where each invited college or professional association will review the evidence and produce a list of five treatments or tests of questionable value. At the same time, the academy will work closely with partners across healthcare to develop a strategy of implementing these changes in clinical practice, embedding a culture of shared decision making in the NHS.
‘Choosing wisely’ goes beyond being a medical initiative in the UK. It is an initiative that will bring together all healthcare professionals with patients to have discussions and make informed decisions about value. The role of pharmacists is essential to the success of this campaign through participation in producing ‘Choosing wisely’ recommendations and also implementing them. Challenging unjustified prescriptions, performing regular medication reviews and, most importantly, engaging patients in a conversation regarding their medicines, are just a few examples of how pharmacists could help reduce overtreatment.
All healthcare professionals share values and responsibilities and we all can and should act as responsible stewards of resources. ‘Choosing wisely’ is just the beginning of a conversation we should all be having, with the ultimate aim of improving patient care and clinical outcomes.
Angeliki Zarkali is clinical fellow at the Academy of Medical Royal Colleges and member of the Choosing Wisely Steering Group.
References
[1] Consultant-led Referral to Treatment Waiting Times Data 2014–2015.
[2] Berwick DM, Hackbarth AD. Eliminating waste in US health care. JAMA 2012;307:1513–1516.
[3] Heath I. Role of fear in overdiagnosis and overtreatment — an essay by Iona Heath. The BMJ 2014;349:g6123.
[4] Richardson B. Clinical examination is essential to reduce overdiagnosis and overtreatment. The BMJ 2014;348:g2920.
[5] New England Healthcare Institute. How many more studies will it take? A collection of evidence that our health care system can do better. A compendium of evidence from 1998–2006.
[6] The School of Pharmacy University of London, Consortium THE. Evaluation of the scale, causes and costs of waste medicines. 3 November 2010;1–106.
[7] NHS England. The NHS Five Year Forward View. 2014.
[8] Monitor. Closing the NHS funding gap: how to get better value health care for patients. 2013.
[9] Campbell EG, Regan S, Gruen RL et al. Professionalism in medicine: results of a national survey of physicians. Ann Intern Med 2007;147:795–802.
[10] ABIMF. Unnecessary tests and procedures in the health care system: what physicians say about the problem, the causes, and the solutions, results from a national survey of physicians. The ABIM Foundation. 1 May 2014.
[11] Charting a fifty percent drop in antibiotics use. Choosing Wisely updates.
[12] Levinson W, Kallewaard M & Bhatia RS. Choosing Wisely: a growing international campaign. BMJ Qual Saf. doi:10.1136/bmjqs-2014-003821.
[13] Choosing Wisely Canada. Spring newsletter 2015.
[14] Choosing Wisely Canada. Updates from the field. North York General Hospital, Ontario – January 2015.


