
Transform / Halo Media
Plainly, the war on drugs is not being won. Drugs are often easily accessed and people will take them. More and more people are taking drugs, and more are dying.
In fact, deaths related to cocaine — now the second most commonly used drug after cannabis — have increased five-fold in England and Wales since 2012, rising to 637 deaths in 2018[1],[2]
. Similarly, in Scotland, 273 cocaine-related deaths were recorded in 2018, compared with 4 such deaths in 2000[3]
.
Startlingly, cocaine-related deaths of women have risen by 26.5% in the past year in England and Wales (compared with 7.7% in men) for reasons that are inconclusive[2]
. Also sobering is that, among people aged 15−34 years in Europe, the UK has the highest prevalence of cocaine use (4.7%) — more than double the European average (2.1%)[1]
.
Clearly, our punitive approach to drug policy could be doing better to curtail illegal supply or deter use.
Instead, prohibition exacerbates health-related harms by pushing people to use unregulated illegal drugs of unknown provenance, sold without even the most basic risk information or advice; all while empowering and enriching organised crime groups who control the drug chains.
So, what can we do? There is no agreement on this. The government’s position remains largely unchanged since the publication of its 2010 drug strategy, focused on targeting drug markets and on recovery for people who use drugs. But this approach is not supported by commissioning: funding for alcohol and drug services has been subjected to significant cuts in recent years (26% between 2014–2015 and 2019–2020) — even as demand for these services has increased[4],[5]
.
Decriminalisation of minor possession offences is one approach to reducing stigma and facilitating more effective health interventions. And this idea is gathering support, particularly from the government’s own expert advisory committee, the Royal Society for Public Health and the Royal College of Physicians, The BMJ and
The Lancet
, as well as all 31 United Nations entities, including the World Health Organization[6],[7],[8],[9],[10]
. To this end, many police forces have already implemented ‘diversion’ schemes, in which people caught in possession are diverted to a health response, rather than prosecution.
What if we could take public health entirely out of the hands of organised crime groups?
But, surely, there is a better way of approaching drug policy? What if we could take public health entirely out of the hands of organised crime groups? What if we could put it into the hands of people who specialise in medicines? What if we could reduce drug-related harm by providing these substances, under strict controls, through pharmacists in state-run pharmacies?
To answer these questions, first we need to understand the risks of taking drugs under our current approach to drug policy and how pharmacists currently support people who take these risks.
Health of people who use drugs
People who use stimulants, with increasing dosage and frequency, become more likely to have health-related issues. Using stimulants can increase high-risk behaviours, such as unsafe sex, polydrug use and sharing of paraphernalia. It can also incentivise crime that helps people who are dependent, and who have a lower income, to fund their purchases.
Some people who use stimulants can experience more serious negative physical and mental health effects, such as cardiovascular problems, anxiety, paranoia, psychosis and increased risk of infections or blood-borne virus transmission associated with sharing of drug paraphernalia, especially when injecting[11]
. There are further risks associated with illegal supplies owing to misselling, unknown strength and the presence of potentially toxic adulterants or bulking agents.
Dependency on illicit drugs is often associated with underlying trauma, especially adverse childhood experiences. The mainstay of treatment — in the case of stimulant dependency — is psychosocial interventions: prescribing of a substitute medication (such as dexamfetamine), while remaining an option, is not currently supported by a robust evidence base. Optimal opioid substitution treatment, however, may be helpful in stabilising and ameliorating stimulant use if the person has a concurrent opioid dependency[11]
,[12]
.
The deterioration of a person’s physical and mental wellbeing can be a significant cause for concern; it can rapidly lead to poor self-care, malnourishment and cardiovascular damage. Engaging people in treatment can also be challenging, especially when dealing with hard-to-reach populations, more complex cases with multiple needs and requirement for highly specialised treatment and support services.
Pharmacy has the skills
Pharmacy professionals already understand these needs and have an essential role in supporting people who use illegal stimulants, including identifying issues during medicines reconciliation and when undertaking medicines reviews. As experts in medicines, pharmacists can readily identify and advise on adverse drug reactions and interactions associated with stimulants, such as serotonin syndrome and QT prolongation[13],[14]
.
The provision of harm reduction advice is essential, and pharmacy teams can support with this
The provision of harm reduction advice is essential. Pharmacy teams can, and already do, provide support with this; for example, by outlining the need to avoid polydrug use, and viral transmission from sharing injecting equipment, pipes when smoking and ‘straws’ used for snorting. They may also supply appropriate paraphernalia and safer injecting advice through needle syringe services, and signpost to supportive organisations, such as the local drug service provider, peer support groups, sexual health and wound management services. Additional harm reduction interventions include providing vaccinations and testing for blood-borne viruses, such as hepatitis C[15]
.
All roads lead to pharmacy
These skills and this body of experience make pharmacy well suited to supporting people who use stimulants, which is why Transform Drug Policy Foundation (a UK-based charity advocating for better drug policies) has been attracting headlines for its argument that pharmacy professionals should be at the heart of a new approach to clamping down on organised crime and supporting those who use drugs[16]
.
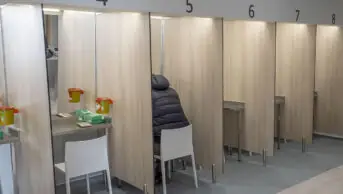
The proposal — which Transform outlines in ‘How to regulate stimulants: a practical guide’ — considers the strictly regulated availability of rationed quantities of certain stimulants for an adult-only, non-medical use market, through government-owned and managed retail outlets (effectively a state retail monopoly), using “a system modelled on pharmacy provision”[17]
.
Transform makes the case that this could provide an effective way of minimising harms where “licensed and trained health professionals serve as gatekeepers”, who are able to enforce regulatory “controls such as restrictions on age, intoxication and amount purchased”. And, crucially, they could “offer specialist advice on safer use, and access to services where needed”.
Vendors could be community pharmacy professionals (with additional training), who are in a good position to facilitate a service such as this, given their demonstrable understanding of drug regulations, safe storage, supply and expertise in drug interactions. The service could be seen as an extension of the support they already provide to people who use substances; and pharmacists already working in specialist substance misuse services could facilitate training. Or perhaps the role could be developed as a distinct professional niche.
Lessons from abroad
This idea isn’t new and lessons can be learned from other countries around the world. For example, cannabis is already being legalised and regulated for non-medical adult use in Uruguay, Canada, Mexico, Luxembourg and 15 US states, while many other countries are actively exploring it.
It is worth noting that the Uruguay model (which Transform was involved in developing) includes rationed retailing of cannabis for non-medical use, from existing pharmacies to registered individuals. Proposals for retailing drugs for non-medical use from existing pharmacies are understandably controversial — as indeed they proved to be in Uruguay, in the case of cannabis. Some Uruguayan pharmacists felt provision of drugs for non-medical use lay outside their responsibilities as health providers, while others made the case that they could encourage safer use and harm reduction, and therefore it fell within their remit of duty of care. Ultimately, only a small minority chose to participate, and plans to establish dedicated licensed retail outlets are being explored[18]
.
Would views differ in other countries or with substances other than cannabis? Transform’s proposal of a dedicated outlet based upon a pharmacy model, rather a service through existing pharmacies, could be more appropriate. Or is there a role for pharmacy at all?
In its proposal, Transform has deliberately not been over-prescriptive about pharmacy’s involvement, and it wishes to engage with pharmacists and facilitate dialogue among the profession, around the details of how such models might be developed.
Drug policy reform — including legal regulation of formerly prohibited drugs — is gathering momentum internationally
What is clear is that drug policy reform — including legal regulation of formerly prohibited drugs — is gathering momentum internationally, and not just with cannabis. In the UK parliament, a debate regarding stimulants such as cocaine, MDMA and amphetamines may still be some way off but, elsewhere, legally regulated markets are not as far-fetched as some may imagine. For example, a bill proposing a strictly regulated market for cocaine (informed by Transform’s book) is currently being debated in the Colombian senate[17],[19]
.
Where and when such reforms do happen, there will be a narrow window of opportunity to influence how they are developed into legislation and regulation. But key stakeholders and sources of relevant professional expertise, who have explored the ideas in advance, will be able to proactively and positively influence the evolution of policy.
Change is coming and it is important to make sure the right people, including pharmacists, are at the policy table.
Steve Rolles is senior policy analyst, Transform Drug Policy Foundation, and lead author, ‘How to regulate stimulants: a practical guide’.
Roz Gittins is director of pharmacy, Humankind, and vice president, College of Mental Health Pharmacy.
Authors’ declaration of interest: Both authors are members of the Scientific Committee for Drug Science.
References
[1] Black C. 2020. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/882953/Review_of_Drugs_Evidence_Pack.pdf (accessed December 2020)
[2] Office for National Statistics. 2020. Available at: https://www.ons.gov.uk/peoplepopulationandcommunity/birthsdeathsandmarriages/deaths/bulletins/deathsrelatedtodrugpoisoninginenglandandwales/2019registrations (accessed December 2020)
[3] National Records of Scotland. 2019. Available at: https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/drug-related-deaths-in-scotland/2018 (accessed December 2020)
[4] HM Government. 2010. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/98026/drug-strategy-2010.pdf (accessed December 2020)
[5] The Health Foundation. 2018. Available at: https://www.health.org.uk/sites/default/files/upload/publications/2018/Taking%20our%20health%20for%20granted_for%20web.pdf (accessed December 2020)
[6] Advisory Council on the Misuse of Drugs. 2011. Available at: https://www.gov.uk/government/publications/sentencing-guidelines-council-acmd-response-2011 (accessed December 2020)
[7] Royal Society for Public Health. 2018. Available at: https://www.rsph.org.uk/about-us/news/royal-college-of-physicians-backs-rsph-calls-on-drug-reform.html (accessed December 2020)
[8] Godlee F. BMJ 2018;361:k2057. doi: 10.1136/bmj.k2057
[9] The Lancet 2016;387(10026):1347. doi: 10.1016/S0140-6736(16)30115-5
[10] Jelsma M. 2019. Available at: http://fileserver.idpc.net/library/UN-Common-Position-Briefing-Paper.pdf (accessed December 2020)
[11] The Royal College of Psychiatrists and the Faculty of Forensic and Legal Medicine. 2020. Available at: https://www.rcpsych.ac.uk/docs/default-source/improving-care/better-mh-policy/college-reports/college-report-cr227.pdf (accessed December 2020)
[12] Arizona Center for Education and Research on Therapeutics. 2016. Available at: https://www.crediblemeds.org/drugsearch (accessed December 2020)
[13] Pharmaceutical Services Negotiating Committee. 2020. Available at: https://psnc.org.uk/services-commissioning/advanced-services/hep-c/ (accessed December 2020)
[14] The Health Foundation. 2018. Available at: https://www.health.org.uk/publications/taking-our-health-for-granted (accessed December 2020)
[15] Department of Health. 2017. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/673978/clinical_guidelines_2017.pdf (accessed December 2020)
[16] McDonald H. The Guardian 2020. Available at: https://www.theguardian.com/society/2020/oct/20/government-urged-to-sell-cocaine-and-ecstasy-in-pharmacies (accessed December 2020)
[17] Rolles S, Slade H & Nichols J. 2020. Available at: https://transformdrugs.org/product/how-to-regulate-stimulants-a-practical-guide/ (accessed December 2020)
[18] Hudak J, Ramsey G & Walsh J. 2018. Available at: https://www.brookings.edu/wp-content/uploads/2018/03/gs_032118_uruguaye28099s-cannabis-law_final.pdf (accessed December 2020)
[19] Barham E. Washington Post 2020. Available at: www.washingtonpost.com/politics/2020/10/19/colombias-lawmakers-are-debating-how-regulate-cocaine-heres-what-we-know-about-decriminalization/ (accessed December 2020)
You may also be interested in

Voice of the Voiceless: co-produced materials to help reduce stigma for people receiving opioid substitution treatment in pharmacies
PJ view: The government’s approach to illegal street drugs should focus on treatment and prevention
