A revolution has emerged; patients have discovered the ‘magical’ weight-loss drug semaglutide, a GLP-1 receptor agonist. The popularity of GLP-1 receptor agonist drugs has skyrocketed, with reports now estimating that sales will reach more than US$125bn by 2033.
But what in particular has instigated such an increase in prescriptions for these drugs? As a trainee pharmacist working on the frontline in a pharmacy supplying semaglutide to patients in central London, I can confidently say that one of the primary reasons behind this increase is how easy it is for patients to access these medicines.
In September 2022, the National Institute for Health and Care Excellence (NICE) recommended semaglutide as an option for weight loss and weight maintenance in patients with at least one weight-related comorbidity and a body mass index (BMI) of at least 35.0kg/m2, or in those with a BMI of 30.0–34.9kg/m2 who meet the criteria for referral to specialist weight management.
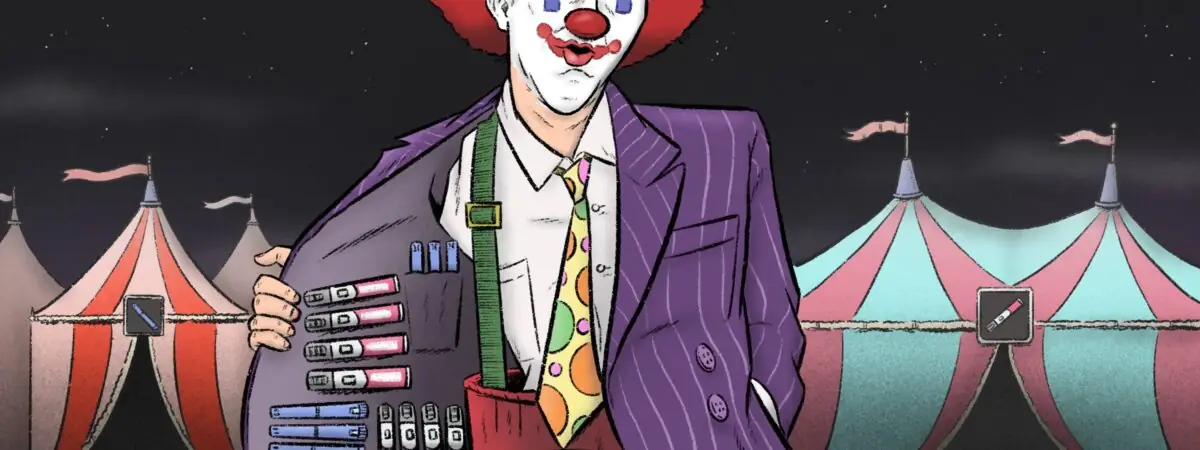
In reality, however, the patients I have seen receiving these prescriptions in the pharmacy range from personal trainers in world-renowned gyms to vulnerable teenagers and holidaymakers making the most of a very loose online prescribing system — many of whom do not meet the criteria to be clinically appropriate for this drug. The unregulated online prescribing of semaglutide, which is being facilitated by several major community pharmacy chains — charging upwards of £100 per month – poses a major threat to patient health.
Associated risks
The risks associated with using semaglutide outside to NICE’s recommendations, include reports of diabetic ketoacidosis, a life-threatening condition requiring urgent hospital admission; acute pancreatitis; and dehydration. Even supplied in line with NICE guidance, risks include acute pancreatitis and dehydration. Another consideration is the increasing incidence of body dysmorphic disorder in young people; potentially vulnerable patients can and should not continue to be exposed to such high-risk drugs.
There are patients mocking the lack of regulation of these online prescribing platforms for weight-loss drugs, completely oblivious to the risks they themselves face
However, inappropriate supply of these drugs is all too common. In June 2024, Vicky Price, president-elect of the Society for Acute Medicine, said hospitals were seeing an “increasing number” of patients with life-threatening complications from weight-loss drugs they had purchased online, including patients with inflammation of the pancreas gland and alterations in blood salt levels.
Price called for “urgent regulation and control of access for weight-loss drugs online to avoid more patients becoming unwell”.
But so far, nothing has changed. In the pharmacy I was training in, patients have expressed their joy to me at how easy and convenient the whole online process of obtaining a prescription for semaglutide is. One of my patients joked: “You must get so many lies coming through. It’s so easy and I never have the same doctor every time I fill in the form.” This is unacceptable. There are patients mocking the lack of regulation of these online prescribing platforms for weight-loss drugs, completely oblivious to the risks they themselves face. Patients simply type in their weight, submit any photo and send off their request.
I have also seen tourists making the most of this prescribing pathway, eagerly coming to collect their medication. One customer from overseas came into the pharmacy with a prescription for a one-year supply of Ozempic (semaglutide; Novo Nordisk) from a private clinic. When I questioned this with the prescriber, I was instructed to “give them whatever quantity they’re looking for”. Patients are not medical practitioners; patients are not self-prescribers; patients do not have the clinical skills to decide what is appropriate.
The safeguards in place are insufficient. While many private prescribing services, including those affiliated with pharmacy multiples, do request the patient’s GP details, the NHS is already exhausted — GPs cannot take responsibility for a private doctor’s prescribing. From personal experience, when it comes to supplying the medicine to the patient, pharmacists are asked to confirm the patient’s address, but there are no follow-up questions. I was not made aware of any protocol to raise concerns. A pharmacist can use their own clinical judgement to intercept the sale of any medication, but I never saw that happen for this drug.
The lack of regulation by the General Pharmaceutical Council (GPhC) or Medicines and Healthcare products Regulatory Agency is actively causing patient harm with no apparent consequences. Regulatory bodies that inform our everyday practice need to start enforcing regulations on to online prescribing platforms. However, the attitudes from pharmacists in community pharmacies towards supplying these online prescriptions are also at risk of facilitating these inappropriate supplies.
Pharmacist responsibility
After personally refusing to hand out a Wegovy (semaglutide; Novo Nordisk) prescription to a clinically inappropriate patient, the on-duty Responsible Pharmacist proceeded to hand it out instead, explaining to me that the provision of this medication was at the prescriber’s discretion and not our responsibility.
After five years of preparing to practise as a pharmacist, I don’t agree. Pharmacists are equally responsible for ensuring the sale of medication is clinically appropriate. Providing person-centred care is the first of the GPhC’s professional standards for pharmacists and requires “thinking about the impact their decisions have on people” (6). Shifting the blame is not acceptable when patient safety is at risk.
This cannot continue to be nobody’s responsibility. Without regulation, such inappropriate sales will continue to rise, along with fatal incidents, with the patient far from the centre of the pharmacist’s care.
In response to concerns raised in July 2024, Wes Streeting, now health secretary, backed calls for tighter regulation, which he said he will “look into carefully”(7). But patients cannot wait for election promises to be put into practice.
As a first step, in-store clinical assessments should be undertaken to submit BMI figures ahead of prescribing. This should be feasible given that many pharmacies are equipped to take BMI measurements already.
Focus on appropriate use
Instead of these drugs causing hospital admissions, strict regulation of prescribers and pharmacies could allow GLP-1 receptor agonist drugs to revolutionise medical care and change the lives of the right patients. Data published in January 2023 show that 63.9% of adults in the UK are overweight or obese (8). Obesity is defined as a BMI of 30 or above, and overweight is classified as a BMI of between 25 and 30. Owing to their weight, these adults are at an increased risk of cardiovascular disease, diabetes and cancer. If used appropriately, these drugs could stop this obesity epidemic and reduce the financial burden on the NHS.
As pharmacists, it is our duty to intervene in a clinically inappropriate or unethical supply of a medication. When it comes to online prescribing in particular, we are the only members of the healthcare team coming face to face with these patients. It is our responsibility to call for regulation and end the exploitation of vulnerable patients. We are at the forefront of supplying these prescriptions and we are equally responsible for the harm coming to patients. Pharmacy teams need to call for change and challenge these prescriptions, not follow the leader and become part of the problem.
I never imagined that at the start of my career I would need to speak out about such a situation, but watching it unfold so rapidly has left me no choice but to speak out for our patients. It’s time to end this disaster.
Resources
- For more information on national guidelines for prescribing semaglutide for weight loss, visit the National Institute for Health and Care Excellence website;
- If you are a member of the Royal Pharmaceutical Society (RPS) and would like one-to-one support on pharmacy practice, ethics, medicines sale and prescription queries, you can access the support helpline every weekday 9am to 5pm;
- If you are an RPS member and would like practical advice and guidance on prescribing, you can access the prescribing support helpline every weekday 9am to 5pm;
- For more information on how to report a concern about a pharmacy, pharmacists or pharmacy technicians, visit the General Pharmaceutical Council website.
- This article was amended on 27 August 2024 to include a box of relevant resources
1 comment
You must be logged in to post a comment.



Dear Brona - well done for critically reviewing the appropriateness. Like you I'm concerned about the use of these drugs. Interesting letter.