
JL / Shutterstock.com
Scotland’s most recently published national data confirm that 1,187 people died in the nation in 2018 as a result of drug overdose[1]
. The sobering figures leave Scotland in the unenviable position of experiencing the highest drug-related death rate in the EU.
The toll equates to the passengers of three full jumbo jets dying each year, and behind the statistics lie personal tragedies — this situation demands outrage and a call for action. These shocking figures mean that Scotland’s drug deaths should be recognised as a public health emergency.
The causes of deaths from overdose are multifactorial, and there is no single solution to bring them to an end. However, there is a wealth of research describing strategies that can begin to reduce them. Some are within the remit of healthcare professionals, including pharmacists, while other interventions, such as reducing poverty and deprivation, require a multi-system approach.
Learning from British Columbia
In 2016, British Columbia, Canada, declared drug-related deaths a public health emergency after 480 people died of accidental drug overdose in 2015. Following the declaration, the province widely implemented interventions to reduce deaths from overdose[2]
. These included expanding access to treatment, facilitating more appropriate prescribing and dispensing, increasing the availability of naloxone, increasing the number of supervised injection facilities, developing facilities to check the content of street drugs, developing a targeted public awareness campaign, enhancing the collection and use of data, empowering service providers, and developing a strategy to promote cultural change.
In May 2019, I attended an interactive workshop that asked what Scotland could learn from British Columbia[3]
. The answer is — a lot.
Filling holes in access to treatment
Scotland should widen and improve its existing services and introduce new strategies to tackle drug deaths.
Some areas of Scotland already have the integrated community-based intervention teams that British Columbia’s response refers to. Methadone and buprenorphine (used to manage opioid addiction) can already be prescribed and dispensed in community-based and primary care settings in Scotland. There is currently no access to other therapies, including diamorphine (used to manage heroin addiction), but an ‘Enhanced drug treatment service’ (to include supervised diamorphine injections) is set to launch in Glasgow in autumn 2019.
We must urgently ensure that treatment is accessible in community pharmacy
We must urgently ensure that treatment is accessible in community pharmacy. We must engage more people in treatment, ensure that prescribed doses are adequate, and reduce unplanned discharges. Community pharmacists and their teams have important roles to play in providing supervised self-administration of methadone and buprenorphine; this supervision provides an opportunity to build positive therapeutic relationships. But prescribing services for addiction are not currently part of Scotland’s community pharmacy contract — pharmacies must opt in.
In other respects, Scotland is leading the way. Following successful local pilots, Scotland became the first country in the world to introduce a full national programme for naloxone (the drug used to treat opioid overdose) in 2010[4]
. But there are still gaps in the service’s provision, despite its success; supply of naloxone following release from prison or police custody, and on discharge from hospital, should become routine. There is also an urgent need to increase the number of kits available in the community, and to ensure that anyone acting in first response, including Police Scotland — who are likely to be first at the scene of an overdose — are able to administer naloxone immediately.
Looking at drug users differently
British Columbia recognised that a public health emergency strategy will not be successful without a change in culture. Stigma towards drug users in the province was widespread and marring interventions designed to reduce drug deaths. British Columbia’s action group sought to change the way people look at those who use drugs and drug services.
However, although organisations such as the Scottish Drugs Forum and the Scottish Recovery Consortium have made strenuous efforts to address stigma around drug use, the public’s discrimination remains largely unchallenged[5]
.
In September 2019, Catriona Matheson, pharmacist and chair of Scotland’s Drug Deaths Task Force, clearly articulated the case for decriminalisation of drug possession for personal use[6]
, and I support this measure to respond to the rising number of deaths. If we are serious about reducing drug-related deaths from overdose, we must have a health-led response to drug users, rather than treating them like criminals.
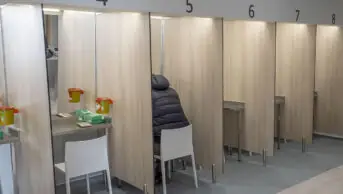
Supervising drug use
A big part of British Columbia’s response was to dramatically increase the number of supervised drug consumption facilities — safe spaces designed to reduce the spread of blood-borne viruses and related infections, reduce overdose and promote health. In these facilities, trained staff supervise the consumption of illicitly purchased drugs, and high-risk drug users are supported to engage with health and social services.
These cost-effective services have been established across Europe for more than 30 years, but there are none in the UK, despite a wealth of evidence to support them[7]
. In 2016, the Advisory Council on the Misuse of Drugs recommended introducing drug consumption rooms, but the UK government dismissed its expert advice[8]
.
Glasgow has built a very strong case for drug consumption rooms
Glasgow, however, has built a strong case for drug consumption rooms[9]
. In evidence given to the Scottish Affairs Committee inquiry into problem drug use in May 2019, Andrew McAuley, senior research fellow in addiction at Glasgow Caledonian University, described the case as “arguably the most compelling Europe has seen”.
Healthcare is devolved to Scotland, but the Misuse of Drugs Act, along with all medicines regulation, is the reserve of Westminster. Glasgow City Council and the Scottish Parliament support drug consumption rooms, but the UK government remains firmly opposed to piloting them. Scotland’s drug deaths must not be allowed to continue while there are untapped means of reducing them. The government must, as a matter of urgency, either amend or devolve to Scotland the relevant legislation to permit these life-saving initiatives.
Scaling up what we know works
After declaring a public health emergency, British Columbia implemented take-home naloxone kits, overdose prevention and supervised consumption sites, and increased uptake of opioid agonist therapy. Irvine et al. investigated the impact of the measures[10]
, finding that between 2,900 and 3,240 lives are estimated to have been saved.
British Columbia’s action group recognised that they were “not going to stop every overdose, eliminate the drivers of addiction, or restore the dignity of everyone who has been traumatised”, but they understood that a lot can be achieved “by scaling up the interventions that we know work[2]”
. This approach should be at the core of Scotland’s initial response to its current drug-death crisis.
A drug plan for Scotland
There are some efforts we can make immediately, including reducing any real or perceived barriers to treatment and recovery services, providing low-threshold access to the full range of opioid substitution therapy treatment options (in line with evidence-based clinical guidelines), scaling up the provision of naloxone, working across all sectors to reduce the stigma experienced by service users and treatment service providers, and maximising the role of primary care.
Alongside the interventions that do not require changes to legislation, we must continue to lobby for services that have, in other parts of the world, demonstrated positive outcomes, and adapt them for Scotland. We must introduce safe drug consumption facilities, drug possession for personal use must be decriminalised, and users must have access to drug-checking facilities that allow them to find out the content of the substances they intend to use.
But these immediate or longer-term actions will not make a difference on their own — we need a system-wide approach that incorporates evidence-based elements to promote safer drug use, reduce harm and save lives.
References
[1] National Records of Scotland. 2019. Available at: https://www.nrscotland.gov.uk/statistics-and-data/statistics/statistics-by-theme/vital-events/deaths/drug-related-deaths-in-scotland/2018 (accessed September 2019)
[2] British Columbia Overdose Action Exchange. 2016. Available at: http://www.bccdc.ca/resource-gallery/Documents/BCOAE-Meeting-Report.pdf (accessed September 2019)
[3] Drugs Research Network Scotland. The Steeple, Dundee, 14 May 2019
[4] World Health Organization. 2014. Available at: https://apps.who.int/iris/bitstream/handle/10665/137462/9789241548816_eng.pdf?sequence=1 (accessed September 2019)
[5] Scottish government. 2016. Available at: https://www.gov.scot/publications/public-attitudes-towards-people-drug-dependence-people-recovery-research-findings/ (accessed September 2019)
[6] Burns C. Pharm J 2019. Available at: https://www.pharmaceutical-journal.com/opinion/catriona-matheson-i-support-decriminalisation-of-illegal-drugs-for-personal-use/20206899.fullarticle (accessed September 2019)
[7] European Monitoring Centre for Drugs and Drug Addiction. 2018. Available at: http://www.emcdda.europa.eu/topics/pods/drug-consumption-rooms_en#intro (accessed September 2019)
[8] Rhodes D. 2017. BBC News. Available at: https://www.bbc.co.uk/news/uk-england-40674453 (accessed September 2019)
[9] Tweed EJ, Rodgers M, Priyadarshi S et al. BMC Public Health 18:829. doi: 10.1186/s12889-018-5718-9
[10] Irvine MA, Kuo M, Buxton JA et al. Addiction 2019:114(9):1602–1613. doi: 10.1111/add.14664
You may also be interested in

Voice of the Voiceless: co-produced materials to help reduce stigma for people receiving opioid substitution treatment in pharmacies
PJ view: The government’s approach to illegal street drugs should focus on treatment and prevention
