Abstract
Aim
To optimise the outcomes of medicines use reviews (MURs).
Design
A prospective analysis of community pharmacies’ asthma MUR interventions and service evaluation through questionnaire feedback.
Subjects and setting
47 community pharmacies in the Hampshire and Isle of Wight Local Pharmaceutical Committee area.
Outcome measures
Improved access to support, particularly for patients who tended not to attend asthma review clinics with their GP or practice nurse. Improved patient adherence to prescribed treatment resulting from a concordant consultation. Demonstrable benefits of the targeted MUR service.
Results
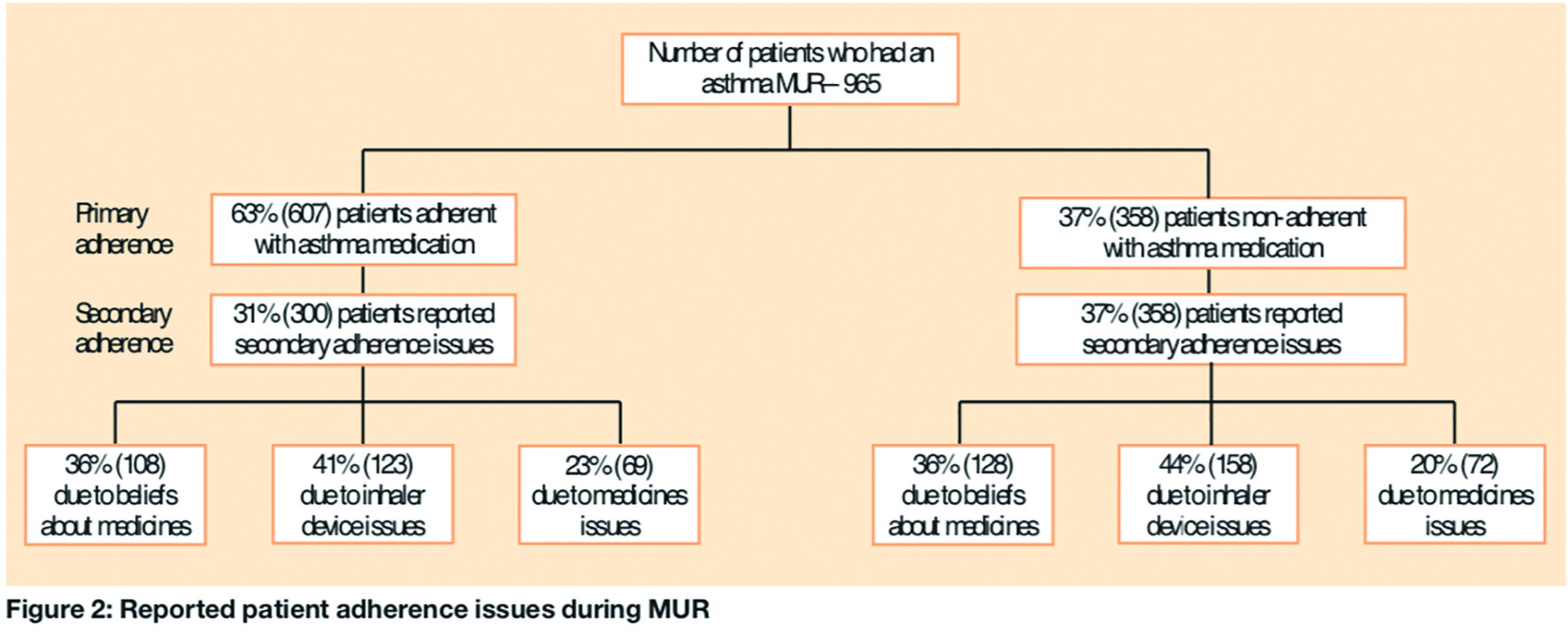
965 patients received an asthma MUR from 46 pharmacies, which each averaged 21 asthma MURs (range 1-67) between July and December 2007. 63 per cent of patients were primarily adherent to their asthma medication. Difficulty using the inhaler was the most common secondary adherence issue in primary adherent (41%, 123) and non-adherent (44%, 158) patients, followed by belief in their medicines. 30 per cent of patients who received an MUR had not seen their GP or practice nurse in the past 12 months. Pharmacists made a total of 1,787 interventions (average 1.8 per MUR consultation) with most being divided between patient education (49%) and device check and demonstration (41%). 230 patients provided requested feedback (24%). 33 per cent of patients who responded to the feedback questionnaire used the MUR service to gain more confidence about their asthma treatment and 19 per cent were seeking specific advice from the consultation.
Conclusions
Community pharmacists have an important role to play in the management of patients with asthma through a targeted MUR service.
More than five million people in the UK live with asthma. An average community pharmacy provides a service for more than 450 asthma sufferers. Research indicates that a large proportion of these patients are inadequately controlled.1–4 The Asthma Insights and Reality in Europe (AIRE) study showed that only 5.3 per cent of the population surveyed met all the goals of the Global Initiative for Asthma (GINA) asthma management guidelines.4
Adherence is the extent to which patients take as intended the medicines which are prescribed for them.5 It is recognised that a significant contributory factor to unsatisfactory asthma control is poor adherence to prescribed medication: up to 70 per cent of patients with asthma do not adhere to some aspect of their recommended treatment.6
Non-adherence can be categorised into two main types: primary and secondary. Primary non-adherence is when patients do not have their prescriptions dispensed. Secondary non-adherence is when patients do not take their medicines the way in which they are prescribed.5
In asthma, this typically involves the under-use of inhaled steroid treatments or inappropriate inhaler technique by patients.7–9 The consequences of each of these can be increased use of “reliever” inhalers leading to deterioration in the patient’s asthma, necessitating intervention by the GP or emergency hospital admission because of an acute exacerbation.9
Medicines use review (MUR) is an advanced service in the community pharmacy contractual framework. The aim of the MUR is to achieve a concordant consultation about medicine-taking by establishing the patient’s actual use, understanding and experience of taking their medicines. The ultimate aim is to improve the clinical and cost effectiveness of prescribed medicines thereby reducing medicines wastage and improving patient outcomes through improved adherence.10
MURs are often a stand-alone service and not integrated into the overall patient care pathway. However, community pharmacists have identified asthma as one of the areas in which they would like to offer a more clinical service.1 By targeting patients with asthma for an MUR, community pharmacists may be able to improve medicines management leading to improved inhaler technique, increased adherence with appropriate treatment and improved outcomes. This project evaluated the MUR interventions made by community pharmacists in the Hampshire and Isle of Wight area and the service through feedback from patients, community pharmacists, GPs and other healthcare professionals involved in the care of the patient.
Method
Subjects and setting
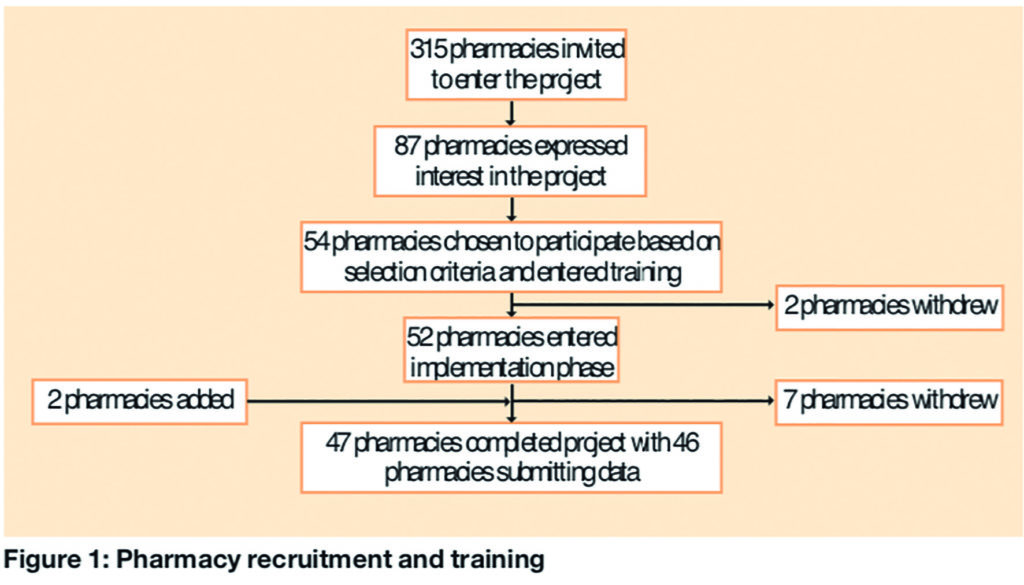
The project was conducted by community pharmacies in the Hampshire and IoW Local Pharmaceutical Committee area. The LPC invited declarations of interest from all 315 pharmacy contractors there. Interested pharmacies were chosen using LPC selection criteria based on MUR accreditation status, recent history of successful delivery of MURs, skill mix, established relationships with GP practices and commitment to the objectives of the service.
Developing the project
The project was developed from the established medicines use review advanced service within the community pharmacy contractual framework. The development process involved the LPC, respiratory consultants, nurses, GPs, primary care trust medicines management teams and support from GSK Plus, which agreed the project protocol and outcome measures involved.
Three training events were held in June and July 2007. Local respiratory consultants, supported by a GP with an interest in asthma and an asthma specialist nurse, delivered training on general asthma pharmacotherapy and patient management. Expectations of a successful asthma MUR and what steps could be taken to deliver one were covered. Pharmacists were allowed to familiarise themselves with the materials in the GSK Plus respiratory MUR resource pack as well as other asthma materials provided by the LPC, including the audit and evaluation process. The number of pharmacies recruited and completing the project is described in Figure 1. In total, 46 pharmacies (20 from national or large multiple groups and 26 independent or small local chains) submitted audit data.
Implementing the project
Following the initial training event, pharmacy staff not at the training evening were familiarised with the documentation and support tools provided. Community pharmacists were asked to make an appointment to meet their local GPs, practice managers and asthma nurses to brief them on the initiative and provide written information on the asthma MUR initiative and general information on MURs.
The objectives of this meeting were: to engage with the GP practice team to ensure an understanding of the aim of the initiative; to integrate MUR activities with the existing care pathway for asthma, in particular in supporting hard-to-reach patients who do not attend clinics or may be non-adherent with their therapy; and to agree protocols for referral and administration. A briefing document was part of the toolkit provided.
Community pharmacists identified and recruited suitable patients with asthma for an MUR. This could be achieved opportunistically at the point of dispensing the prescription, by searching the pharmacy patient database or by referral from a GP practice (although GPs would not be directing patients to a particular pharmacy). These patients were not limited by inhaler device or treatment.
An MUR consultation was performed on identified patients. Placebo inhalers were used to demonstrate appropriate use. The In-Check DIAL (Clement Clarke) was used to assess inspiratory flow during consultations.
Patients’ primary adherence was determined by prescription counting. Patients collecting less than 75 per cent of intended asthma prescriptions in the previous 12 months were deemed non-adherent.
At the end of the MUR, the pharmacist completed the MUR service form, sending the white copy of the action plan to the GP. Patients were referred to the GP or asthma nurse as appropriate and as agreed at the initial briefing. The patient was given a copy of the assessment form and the action plan, together with any patient information leaflets to support adherence and a copy of the patient feedback form to complete anonymously and return to the LPC for evaluation. The pharmacist completed an audit form that captured anonymised key outcomes of the MUR consultation: date, whether the patient had seen a GP or asthma nurse in the past 12 months, adherence status, adherence issues (beliefs, device, medicine) and pharmacist’s intervention (education, device technique check, referral to GP or nurse). A copy was posted or faxed to GSK for analysis and report generation.
At the completion of the project, GPs and asthma nurses were given a copy of the healthcare professional feedback form to complete anonymously and fax back to the LPC for evaluation. Finally, the pharmacist completed a feedback form for return to the LPC for evaluation.
Data collection forms
In addition to the standard MUR service form, four data collection forms were used: an audit form (see above) and feedback forms from patients, pharmacists and other healthcare professionals involved in the patient care pathway. These forms were designed and tested by the LPC with input from clinicians and academics based on desired outcome measures.
Support for pharmacists
Hampshire and IoW LPC commissioned a pharmacist experienced in the delivery of MURs for one day a week to provide support to the pharmacies involved. Support included troubleshooting and motivational coaching in person and by telephone. There was also telephone support from GSK Plus on the gathering and return of the anonymous patient data. The LPC wrote and distributed four newsletters for the pharmacy participants to provide ongoing hints, tips and updates.
Outcomes
The data and information outcomes were captured by GSK and the LPC and then analysed by academics at Portsmouth University under the guidance of one of the present authors (Jane Portlock).
MUR outcomes
The target for asthma pattient consultations over the period of July to December 2007 was a minimum of 1,250 (25 per participating pharmacy), with a more ambitious goal of 2,000 consultations (40 per pharmacy). There was no intention to limit the pharmacy’s MUR activity to patients with asthma since other MURs would also be beneficial to the broader patient population.
From the audit data submitted from 46 pharmacies, a total of 965 patients received an asthma MUR in the project period. These pharmacies averaged 21 asthma MURs (range 1–67). The reported primary and secondary patient adherence issues following the MUR are detailed in Figure 2.
Non-consulting asthma patients
Thirty per cent of patients who received an MUR had not seen their GP or practice nurse in the past 12 months. From these data a comparison of the time since last review and whether or not patients were considered to be adherent with their medication indicated that the level of adherence was significantly higher in the group who had received a review at their GP practice in the past 12 months (chi-squared, P= 0.003).
Pharmacist interventions
Pharmacists made a total of 1,787 interventions (average 1.8 per MUR consultation). Forty-one per cent (731/1,787) were device checks; 10 per cent (184/1,787) were GP or nurse referral and 49 per cent were educational.
Patient feedback
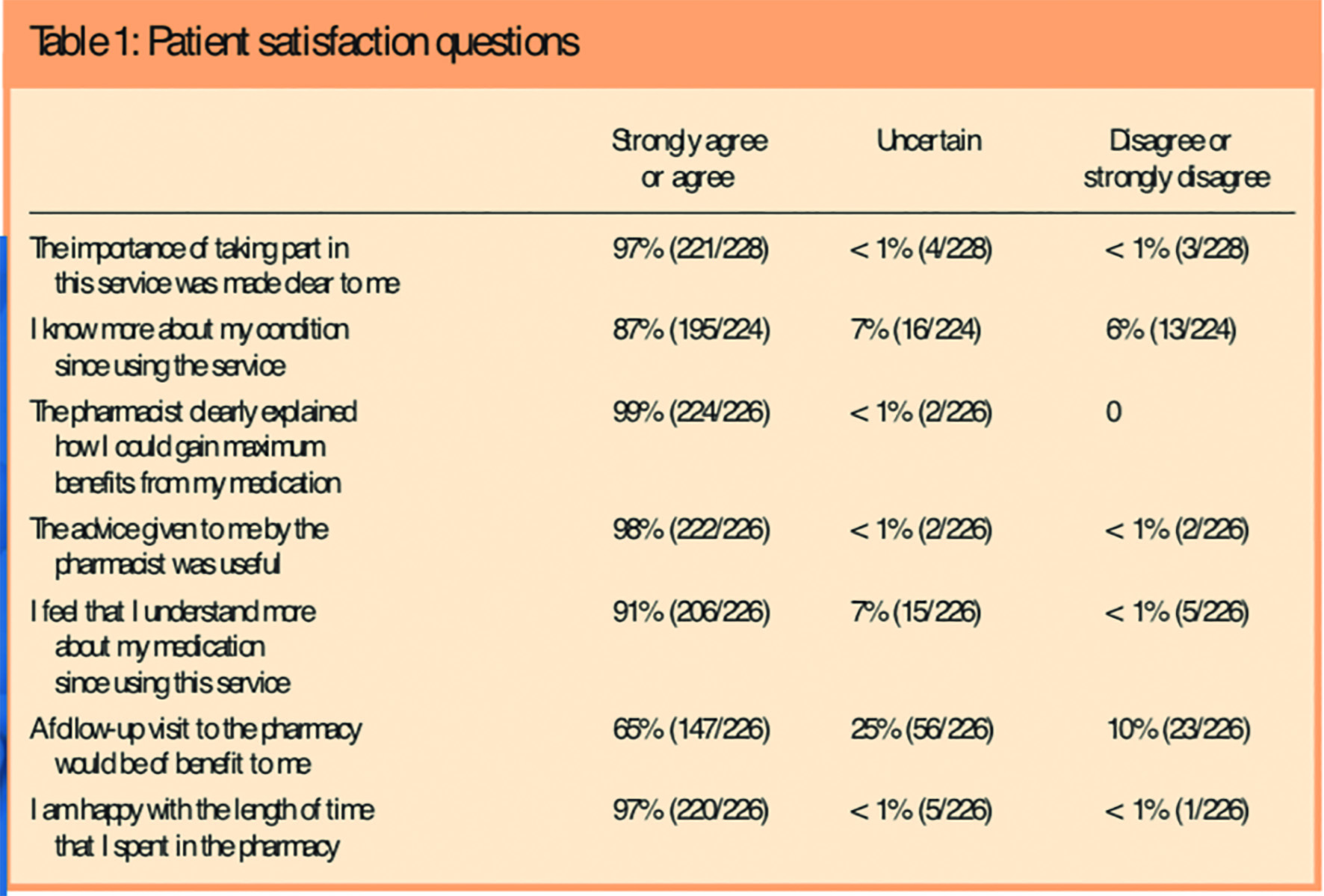
Twenty-four per cent (230) of the patient feedback forms handed out were returned, an average of five per pharmacy (range 1–17 forms). The reasons given for using the MUR service fell into five main areas: concern (7 per cent), advice (19 per cent), knowledge (25 per cent), confidence (33 per cent) and other (16 per cent). Table 1 details the analysis of the eight questions about the service. The responses were combined into three groups: strongly disagree or disagree, uncertain, and agree or strongly agree, because the numbers in some of the five response categories were low/zero.
Three open questions at the end of the questionnaire elicited a range of comments, which were grouped into themes with direct quotes in italics below. From 209 statements by patients about why they liked the service several key themes emerged: the overall impression of the service (friendly, polite, relaxed, courteous); privacy (one-to-one, private); demonstration (of the inhalers); explanation of the medicines and convenience (short MUR, local, convenient) and contact with the pharmacist. Some typical examples of the statements are:
Overall impression of the service
It was relaxed, relatively informal, yet very informative. The pharmacist took the time to ask about and understand the impact of asthma to my lifestyle and gave suggestions.
Privacy
I liked the friendly relaxed atmosphere and knowing it was confidential. I felt at ease and able to talk openly about symptoms and medication I am on.
Demonstration
I was using my inhaler the wrong way, the pharmacist demonstrated the correct way.
Explanation
I learned how to get the most benefit from my medications in a clear and informative fashion.
Convenience
Quick and easy, very worthwhile.
A total of 19 statements were made by patients about aspects of the service they did not like. These related to the length of time (too long) and the unexpected nature of the appointment, the lack of privacy, inconvenient location (upstairs) or interruption to the consultation. Other statements included:
Felt a bit under scrutiny and pressure to take part.
If there are any medical problems [there] may be a delay between the pharmacists having to send notes to the doctor then getting back in [to see their GP].
Finally, the patients were asked to provide any further comments. 128 comments were made, and no new themes emerged in addition to those originally identified.
Pharmacist feedback
Sixty-one per cent (28) of questionnaires were returned by participating community pharmacists. Responses indicated that most MURs had been initiated by the community pharmacists or other pharmacy staff (technicians, dispensing or pharmacy assistants). Only one MUR was initiated by a GP.
All community pharmacists agreed or strongly agreed that they have an important role to play in the management of patients with asthma. Eighty-nine per cent (25/28) agreed that the training provided enabled them to implement the service confidently. Seventy-one per cent (20/28) agreed or strongly agreed that they had received sufficient information and support, and found the meetings and updates of benefit in helping them provide the MUR service. Sixty-four per cent (18/28) of respondents agreed that participation in the MUR service had developed their professional working relationship with other healthcare professionals. All respondents agreed that they would welcome the opportunity to work more closely with other healthcare professionals on similar services. All but one respondent would like to participate in similar services in the future.
Healthcare professional feedback
Thirty-three per cent (15/46) of question-naires were returned from healthcare professionals (all GPs). Ninety-three per cent (13/14) of respondents were aware of the MUR initiative. Eighty-six per cent (12/14) of respondents agreed that the criteria and protocol for referral of patients were clearly agreed with the community pharmacist. Eighty-six per cent (12/14) of respondents agreed that community pharmacists have an important role to play in managing patients with asthma, Seventy-nine per cent (11/14) agreed that asthma MURs were of benefit to patients. Seventy-one per cent (10/14) agreed that this service supports the achievement of quality and outcomes framework (QOF) targets. Finally, 57 per cent (8/14) agreed that this programme should reduce their long-term workload.
Further comments related to the advantage of MURs to provide an opportunity for dialogue with local pharmacists and a forum for good communications between pharmacist and GP surgery. Four respondents suggested other areas for development of an MUR service including diabetes, chronic obstructive pulmonary disease and hypertension.
Discussion
The range in the number of MURs carried out was wide, indicating that the opportunities for carrying out an MUR seem to vary considerably between pharmacies. This could be due to different barriers that the pharmacy team need to overcome in delivering MURs, such as skill-mix differences in the pharmacies, approach to recruitment and referral for MUR, dispensing burden, confidence or incentives. These barriers have also been identified in previous research.11, 12
Prescription counting as a measure of primary non-adherence has limitations, such as the need for complete pharmacy records or patient recall of the number of prescriptions filled over the past 12 months. Despite patients reporting adherence to collecting their prescriptions as prescribed, further investigation by the pharmacist during the MUR elicited secondary adherence issues in 31 per cent of these patients. Data analysis of the audit data indicated that the level of adherence was significantly higher in the group that had received a review from their GP in the past 12 months (chi squared, P=0.003). It is recognised that frequent interactions with patients by healthcare professionals can benefit adherence,13 which reinforces the benefit that an MUR can have on patient adherence.
Pharmacists made an average of two interventions per consultation, with most being divided equally between patient education and device demonstrations. This compares well with a similar study of asthma medicines support in community pharmacies where nearly two thirds of patients received one or more significant intervention.14
A patient feedback response rate of 24 per cent means the opinions may not have been representative of the entire patient population. The main reason reported by patients for using the MUR service was to gain confidence about their asthma treatment followed by specific advice from the consultation. Through the MUR process pharmacists can provide an opportunity for patients to gain confidence about their medicines and, in turn, overall control of their disease. Another limitation on this project was that patients’ asthma control was not measured before and after the MUR intervention, and would warrant further investigation as to whether MURs do improve patients’ asthma control.
Several themes emerged from the comments from patients on why they liked the service: their overall impression of the service, privacy, demonstration (and the use of the In-check DIAL), the convenience and direct contact with the pharmacist.
The impressions of patients described in this project are important to the pharmacy profession because they could be used to promote MUR campaigns and form part of the education and support for pharmacists in new areas for MURs and other patient-centred services. The demonstration of inhaler technique was a successful feature of the MUR as perceived by patients, and perhaps other MURs could build on this success.
This project highlighted that the unexpected nature of an MUR consultation may not be the best strategy on every occasion. In these situations the ability for the patient to book an appointment or, at least, a clear indication of how long the consultation would take would be advantageous, so that the patient can make an informed choice and not feel they have been coerced into an activity that lasted longer than they were led to believe. However, in contrast to this, patients appreciated local, efficient and quick consultations. So there is merit in promoting easy access to such a service for the patient.
Community pharmacists found the initial training sessions, continued support and regular updates valuable. It would be useful to adopt a similar approach to similar projects in future. The model developed for this asthma MUR initiative is an appropriate one because community pharmacists would welcome the opportunity to work more closely with other healthcare professionals and would like to participate in similar services. Further work needs to be done on the relationship between pharmacists and GPs, since only 64 per cent thought their working relationship had improved. Future initiatives need to include a strategy for enhancing that relationship and encouraging GPs and other healthcare professionals to refer more people for MURs.
This project highlights that more work needs to be done on explaining the benefits of MURs to GPs and other healthcare professionals, in terms of support for QOF targets, reducing medicines waste, improving patient adherence and reducing workload. Future initiatives may need to include additional information for GP practices, as well as negotiation and influencing skills to support the pharmacist/GP relationship.
Conclusions
Community pharmacists have an important role to play in managing patients with asthma through a targeted MUR service, especially patients not routinely seen by their GP, and in managing non-adherence to asthma medication through concordant consultations.
Patient adherence was significantly higher in the group who had received a GP review in the previous 12 months than in the group that had not. Patient respondents used the MUR service to gain confidence and to seek advice about their asthma medication. They reported a high level of satisfaction following the MUR consultation. The benefits of a targeted asthma MUR service by community pharmacists should be incorporated into a locally commissioned multidisciplinary asthma patient care pathway.
Key findings
- 30 per cent of patients who received an asthma MUR had not been reviewed in the past 12 months by their general practice team.
- There were wide variations in the number of MURs completed in each participant pharmacy, indicating different constraints to delivering MURs in practice.
- A lack of understanding on how to use their inhaler correctly or dexterity issues was identified as the most frequent reason for non-adherence to medication.
- 33 per cent of patient respondents used an asthma MUR service to gain confidence about their asthma treatment.
- As a result of the consultation, 90 per cent understand more about their treatment, and 83 per cent know more about their condition.
Acknowledgements
The project was jointly funded by Hampshire and Isle of Wight Local Pharmaceutical Committee and GlaxoSmithKline UK Ltd (GSK), which also provided support materials for the project. The LPC thanks the participating pharmacies for their dedicated contribution to this project. We also thank Deborah Evans (LPC development lead), Lisa Martin (LPC MUR facilitator), Jo Addison (LPC office PA), Simon Kohler (GSK Plus key account manager) and Deborah Worthington (GSK Plus services manager) for input into project development, implementation and evaluation.
Conflicts of interest
There were no conflicts of interest in respect of LPC employees. The study was supported by GlaxoSmithKline UK Ltd within ABPI and LPC governance frameworks.
About the authors
Jane Portlock, PhD, MRPharmS, is principal lecturer in pharmacy practice in the School of Pharmacy and Biomedical Sciences at the University of Portsmouth. Michael Holden, MRPharmS, is chief officer, Hampshire and Isle of Wight Local Pharmaceutical Committee. Shailesh Patel, MSc, MRPharmS, is brand manager, GlaxoSmithKline UK Ltd.
Correspondence to: Michael Holden, Chief Officer, Hampshire and Isle of Wight Pharmaceutical Committee, 59 High Street, Odiham, Hampshire RG29 1LF (e-mail office@hampshirelpc.org.uk)
This paper was accepted for publication on 17 December 2008
References
- Colin-Thome D. Long-term conditions: integrating community. Executive summary. London: Royal Pharmaceutical Society and Webstar Health, 2006.
- National Asthma Campaign. Out in the open. A true picture of asthma in the United Kingdom today. Asthma Journal 2001;6(Suppl):1–14.
- Price DB, Ryan D, Pearce L, The AIRE study. Asthma Journal 1999;4:74–78.
- Rabe KF, Vermeire PA, Soriano JB, Maier WC. Clinical management of asthma in 1999: the Asthma Insights and Reality Europe (AIRE) study. The European Respiratory Journal 2000;16:802–7.
- Cox K, Mynors G. Project evaluation toolkit. London: Medicines Partnership, 2003.
- Bender B, Milgrom H, Rand C. Non-adherence in asthmatic patients: is there a solution to the problem? Annals of Allergy Asthma and Immunology 1997;79:177–85.
- Carter S, Taylor D, Levenson R. A question of choice — compliance in medicines taking. London: Medicines Partnership, 2005.
- Berg JS, Dischler J, Wagner DJ, Raia JJ, Palmer-Shevlin N. Medication compliance: a healthcare problem. Annals of Pharmacotherapy 1993;27:1–24.
- British Thoracic Society, Scottish Intercollegiate Guidelines Network (SIGN). British guideline on the management of asthma. Thorax 2003;58(Suppl I):i1–94.
- Pharmaceutical Services Negotiating Committee.Medicines use reviews service specification. Available at www.psnc.org.uk.
- Hall J, Smith I, Adams A. Why are pharmacists not doing MURs? Abstract presented at the HSRPP Conference 2006, Bath. 3–4 April 2006. Abstract no 61.
- Blenkinsopp A, Celino G, Bond C, Inch J. Medicines use reviews: the first year of a new community pharmacy service. Pharmaceutical Journal 2007;278:218–23.
- Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence. Cochrane Database of Systematic Reviews 2008, Issue 2. Art No.: CD000011. DOI: 10.1002/14651858.CD000011. pub3.
- Pharmaceutical Care Awards. Pharmaceutical Journal 2006;277:43.
