Abstract
Introduction: Owing to high demand and staff recruitment challenges, child and adolescent mental health services (CAMHS) in England have struggled to meet expectations set by the NHS and Royal College of Psychiatrists Quality Network for Community CAMHS, leading to long waiting times and restriction of access to services. Although nurse and pharmacist independent prescriber roles are well established in the UK, there is limited literature on specialist or independent prescriber pharmacist involvement in CAMHS.
Aim: This evaluation aimed to explore the outcomes of integrating two pharmacist independent prescribers into community CAHMS and the acceptance of their roles as part of the multidisciplinary team (MDT).
Method: Two band 8a specialist pharmacists were recruited and trained to achieve independent prescriber status as part of a service improvement strategy within the community CAMHS team at Hertfordshire Partnership University NHS Foundation Trust. To evaluate the outcome of their integration, a purposeful documentation of the pharmacist’s clinical activities, self-administered surveys of the families of patients and the CAMHS MDT, and focus group discussions with the MDT were undertaken between July 2019 and March 2020. A descriptive analysis of quantitative data and content analysis for qualitative data was applied to provide a general view of the pharmacists’ contributions and others’ acceptance of their role.
Results: Three months post integration into the CAMHS team and prior to achieving independent prescriber status, the specialist pharmacists documented a total of 322 explicit contributions to care over a subsequent three-month period. These contributions included prescription transcribing, joint development and wellbeing assessment, monitoring of physical health parameters and provision of medicines-related advice to the MDT. As independent prescribers, the pharmacists’ involvement expanded to independently lead attention deficit hyperactive disorder (ADHD) clinics, with a designated caseload to manage. Responses from surveys and focus group discussions suggested an overwhelmingly positive reception to the pharmacist’s role. All respondents in the families’ survey (40% response rate; n=20/50) indicated that they strongly agreed that the pharmacist was a valuable member of the ADHD team within CAMHS. The need to normalise the integration of pharmacist independent prescribers as core members of the ADHD CAMHS team resonated in the MDT focus group discussions and MDT survey (62% response rate; n=13/21).
Conclusion: This evaluation identifies a clear role for pharmacists in the CAMHS setting, and demonstrates high acceptability by children, young people, their families and healthcare professionals. Pharmacists can successfully be recruited, trained and integrated into a community CAMHS team, thereby supporting the alleviation of pressures within CAMHS services.
Keywords: Child and adolescent mental health, independent prescriber, mental health, non-medical prescriber, pharmacist, psychiatry.
Original submitted: 17 October 2020; Revised submitted: 14 December 2020; Accepted for publication: 18 January 2021.
Key points
- There is limited literature on specialist or independent prescriber pharmacist involvement in child and adolescent mental health services (CAMHS);
- Over the past five years, the demand for CAMHS has increased significantly nationally, yet recruitment of medical staff has remained challenging;
- This evaluation shows that pharmacists can perform extended roles and do not have to limit their contributions to medicines-related issues if appropriately trained;
- Pharmacists were able to manage an ongoing caseload in an attention deficit and hyperactivity disorder clinic, and adjust medication, including starting, stopping and changing doses;
- Service user satisfaction was positive regarding pharmacist involvement and was reinforced during the focus group discussions with the multidisciplinary team.
Jump to:
Introduction
Since 2010, successive UK governments have pledged to improve the mental health support provided to children and young people in England[1–6]. In 2011, the mental health strategy ‘No health without mental health’ outlined the government’s pledge to provide early support for people with mental health problems[1]. Similarly, in 2014, the ‘Closing the gap: priorities for essential change in mental health’ strategy detailed ambitions to improve access to psychological therapies for children and young people[2]. In 2015, the Department of Health (now Department of Health and Social Care) and NHS England established the children and young people’s mental health and wellbeing taskforce that set out ambitions to improve care over the next five years[3]. In addition, the NHS ‘Five year forward view for mental health’ was launched and included specific objectives to improve treatment for children and young people[4]. In December 2017, a green paper on children and young people’s mental health set out measures to improve mental health support, particularly through schools and colleges[5]. It is important to note that treatment pathways across the country are not uniform as different commissioning and paediatric services exist.
Despite the pledges and objectives set out since 2010, child and adolescent mental health services (CAMHS) in England have struggled to meet expectations owing to high demand and staff recruitment challenges, which has led to long waiting times and restricted access to services[7,8]. The 2018 CAMHS NHS benchmarking network project reported sustained increases in demand for services, with a 15% increase in mean referral rates per 100,000 population (age 0–18 years) reported in 2018–2019 (n=3,658), compared to 2017–2018 (n=3,126)[7]. Although this report noted that referral acceptance rates had increased, along with rates of young people who access their first CAMHS clinical assessment and subsequently commence treatment, increases in young people on waiting lists to access CAMHS services remain widespread[7]. In addition to the increasing demand for CAMHS services, the Royal College of Psychiatrists 2019 workforce census for consultant and specialty doctor psychiatrists noted significant concerns regarding consultant vacancy rates within CAMHS; the pre-report summary showed this was 12.14%[9]. Increasing demand and medical recruitment challenges within CAMHS presents a significant challenge, and requires organisations to consider alternative and innovative ways of delivering a safe and effective service[8].
An important strategy used by NHS organisations in addressing workforce challenges and managing medical recruitment challenges is to review the skill mix of teams and, where possible, consider which healthcare professional is best placed to deliver aspects of care[6,10,11]. Pharmacists, nurses, paramedics and physiotherapists are examples of healthcare professionals now working as advanced clinical practitioners to meet the healthcare needs of their local population[6].
Supplementary prescribing for nurses and pharmacists was first introduced in 2003 and was rapidly followed by independent prescribing in 2006[12,13]. An evaluation of nurse and pharmacist independent prescribing commissioned by the Department of Health in 2010 reported that nurse and pharmacist independent prescribing is safe, clinically appropriate and highly accepted by other healthcare professionals and patients[12]. Nurse and pharmacist independent prescribers are now well established within general acute and primary care settings in the UK[14–17]. Nurse independent prescribers are already an established part of the community CAMHS multidisciplinary team (MDT) at Hertfordshire Partnership University NHS Foundation Trust (HPFT); however, recruitment and retention of nurses in this area has been an issue acknowledged by an Education Policy Institute Commission report, providing the opportunity to explore pharmacist independent prescribers in this project[18]. Complementary to the skill set of nurses, pharmacist prescribers can support cost-effective prescribing and the selection of the most appropriate formulations of medicines, and resolve shared care issues with primary care.
There is limited published literature on the role of pharmacists working as independent prescribers within mental health services and, in particular, CAMHS. A 2019 conference abstract reported the benefits of establishing a pharmacist-led attention deficit hyperactive disorder (ADHD) titration clinic to support a reduction in waiting times[19]. This six-month evaluation was created in response to patients having to wait up to seven months after diagnosis to commence medication. A pharmacist’s involvement led to 28 patients being initiated onto ADHD medication. The findings suggested that by utilising the pharmacist independent prescriber to initiate and titrate medication, time was freed up for the specialist nurse to focus on initial assessments and review clinics. As a result, the clinical group planned to provide permanent funding for the pharmacist role to continue to support the new model of ADHD clinic[19].
A 2016 evaluation conducted by Lyon and Brown focused on the deployment of a dedicated pharmacist to support CAMHS to optimise medicines use through working with medical staff and managers across nine teams[20]. The evaluation reported a reduction of around £133,000 in expenditure over 7 years (2007–2008 to 2014–2015) with a net saving of £97,000 through a variety of activities that included: auditing doctors’ prescribing to identify unusual prescribing patterns; promoting the use of stimulant ADHD medication only on school days; organising and reporting the results of audits against shared care guideline standards for ADHD treatment; and utilising evidence-based decisions to reduce the maximum dose of immediate-release melatonin prescribed for new patients from 12mg/day to 6mg/day[20]. While most of the activities reported contributed to positive outcomes, including cost savings, promoting the use of ADHD medication only on school days is still debatable, and dependent on agreed individualised therapy outcomes. The literature suggests that planned drug holidays in children and young people treated with ADHD medication are mainly family-led; some families initiate drug holidays on non-school days to limit the side effects of medication, while others continue on non-school days to maintain tranquillity in the home[21,22].
Aims and objectives
To explore the outcomes associated with the integration of two band 8a pharmacist independent prescribers into HPFT community CAHMS, and acceptance of their roles by service users and healthcare professionals as experts in medicines use as part of the multidisciplinary team. The evaluation was designed to:
- Understand the contributions to care made by specialist pharmacists integrated into the community CAMHS MDT;
- Identify pharmacist contributions within a pharmacist independent prescriber-led ADHD clinic;
- Understand the service user experience;
- Understand the acceptance of the specialist pharmacist and pharmacist independent prescriber role within CAMHS by other healthcare professionals.
Setting
In April 2019, two experienced clinical pharmacists were recruited and integrated into the HPFT community CAMHS MDT. Prior to this appointment, pharmacists were not integrated within community CAMHS in the organisation. Medicines management support was instead provided via the central pharmacy team that focused on answering medicines information-related queries.
The newly recruited pharmacists were line-managed and supervised by the consultant psychiatrist, with professional supervision provided by the trust’s chief pharmacist. The pharmacists began their independent prescribing qualification course in May 2019. For the purposes of the independent prescribing course, the pharmacists chose ADHD as their scope of practice under the guidance of their designated medical practitioner (DMP). This approach ensured they received the right guidance, training and acquisition of competencies to manage children and young people with ADHD. As there are a limited number of pharmacological treatment options for the management of ADHD, this allowed the pharmacists to build up their specialist competence in this focused area relatively quickly and implement the agreed shared care of ADHD medications with primary care.
Over a six-month period (June to November 2019), the pharmacists were trained by the consultant CAMHS psychiatrist in all CAMHS-related issues, in a similar fashion to a medical doctor first entering CAMHS. Following successful completion of their independent prescribing course in January 2020, the pharmacists established a pharmacist-led ADHD clinic. Children and young people who had an established diagnosis of ADHD, and had an agreed treatment plan, were referred to the pharmacist-led ADHD clinic by the consultant. In the clinic, the pharmacist provided ongoing review appointments, prescribed medication with any dose adjustments as necessary, initiated new medication or stopped medication with consultant approval, and undertook all associated patient and drug monitoring (e.g. height, weight, blood pressure and pulse).
A Health Education England grant of £10,000 was awarded for this project. The funds were used to support enrolment onto the IP course and continuing professional development. The posts were funded internally through medical vacancies.
Methodology
Mixed method approaches were used prospectively to understand the outcomes of integrating pharmacists into community CAHMS and the acceptance of their roles as part of the MDT. This evaluation had a specific focus on the management of ADHD for a variety of reasons, including increasing caseload numbers and long waiting times for ADHD assessment and commencement of therapy. The pharmacists were fully integrated into the HPFT community CAMHS MDT three months post-recruitment and their contributions to care were self-recorded on a pre-designed data collection form (using an Excel spreadsheet) between July and September 2019. Data recorded by the pharmacists included the type of service and advice provided, number of initial and follow-up consultations, number of prescriptions and clinical letters written, number of physical health assessments completed and number of patients switched to an alternative cost-effective medication preparation.
The child or young person (if appropriate) and their family or carer’s experience of the pharmacist’s consultation was obtained using a self-administered questionnaire (see supplementary file 1), inclusively issued to them from December 2019 to January 2020. The pharmacists provided the questionnaire after the consultation, but families were asked to complete it anonymously and return in a designated post box at the exit of the building. The questionnaire was developed from the literature, relevant to this evaluation, and then reviewed for practicality and clarity by the evaluation team[23,24]. A free text box was provided on the questionnaire for the child or young person to include any comments they wanted to share based on their experience of the consultation. To evaluate the pharmacist-led ADHD clinic, all prescriber-related clinical activities and outcome data were recorded on a pre-designed data collection form from the beginning of February to the end of March 2020. To understand the acceptance of the pharmacist’s role, including those undertaken as independent prescribers within community CAMHS by other healthcare professionals in the MDT, two focus group discussions were undertaken with members of the CAMHS MDT.
The focus group discussions took place on 16 and 31 January 2020, and were facilitated by a pharmacist researcher independent of the organisation[25]. Prior to the focus group discussions, a short electronic survey (see supplementary file 2) was also undertaken with MDT members in January 2020 to provide an opportunity for those who could not attend the focus group discussion to contribute. Survey questions asked respondents to indicate their role within CAMHS, and whether the introduction of a pharmacist within CAMHS had been beneficial on a Likert scale of 1 to 5, where 1 was ‘non-beneficial’ and 5 was ‘extremely beneficial’. Respondents were also asked if they had received any support from the pharmacists within CAMHS, requiring a ‘yes’ or ‘no’ response.
Quantitative data was analysed descriptively in order to categorise the different activities recorded by the pharmacists, and also to report responses obtained from both the service user and service provider surveys. Qualitative data from the focus group interviews was transcribed and analysed by the pharmacist researcher using a content analysis approach[26].
There was no requirement to obtain ethical approval for this service evaluation; however, the trust audit team were notified.
Results
The contributions made by the specialist pharmacists integrated into the community CAMHS MDT, and prior to achieving their independent prescriber status, are shown in Table 1. A total of 322 contributions were self-recorded and categorised by the pharmacists from July to September 2019. Conventional pharmacist contributions were noted in a third (34%) of recorded activities, such as provision of medicines-related advice and resolution of medicines-related queries. However, the majority of contributions (66%) could be considered as uncommon to a pharmacist’s role. These contributions included transcription of prescriptions, supporting children in their transition to adult services, and development and wellbeing assessment (DAWBA) consultations under the supervision of the consultant psychiatrist. The number and breadth of contributions reflected the varied duties and responsibilities that the pharmacists assumed.
Table 1: Specialist pharmacists’ contributions to care
| Contribution | Frequency (%) |
| Prescriptions transcribed | 87 (27) |
| Joint development and wellbeing assessment consultation and follow-up | 58 (18) |
| Monitoring of physical health parameters | 45 (14) |
| Provision of medicines-related advice to the multidisciplinary team | 45 (14) |
| Medication review consultations | 32 (10) |
| Pharmacist-led development and wellbeing assessment consultations | 19 (6) |
| Resolution of medicines-related queries | 19 (6) |
| Switching to cost-effective medication formulation/preparation | 13 (4) |
| Supporting transitioning to adult services | 4 (1) |
| Total | 322 (100) |
Table 2 illustrates the outcomes of the pharmacist-led ADHD clinics, where activity and outcome data were collected for 50 children and young people from February to March 2020. Time spent per appointment included face-to-face consultations.
Table 2: Pharmacist-led attention deficit hyperactivity disorder clinic activities and outcomes
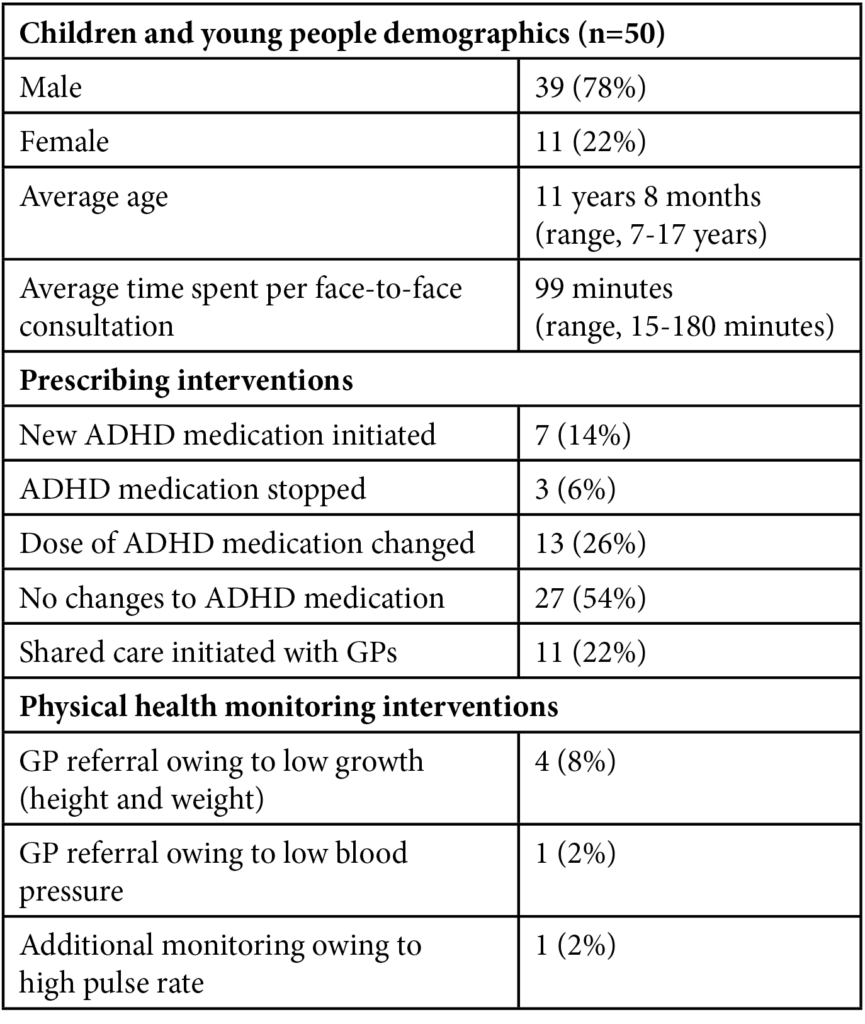
The pattern of prescribing interventions made was inconsistent; however, a dose increase accounted for 77% (10/13) of dose changes owing to suboptimal therapy. Four of the children and young people had growth-related issues, with low weight being a problem. One patient reported a high pulse but was below the threshold of 120 beats per minute for a referral to specialist services or dose reduction, and therefore was placed under additional monitoring. One patient was identified with low blood pressure and referred to the GP for further investigation.
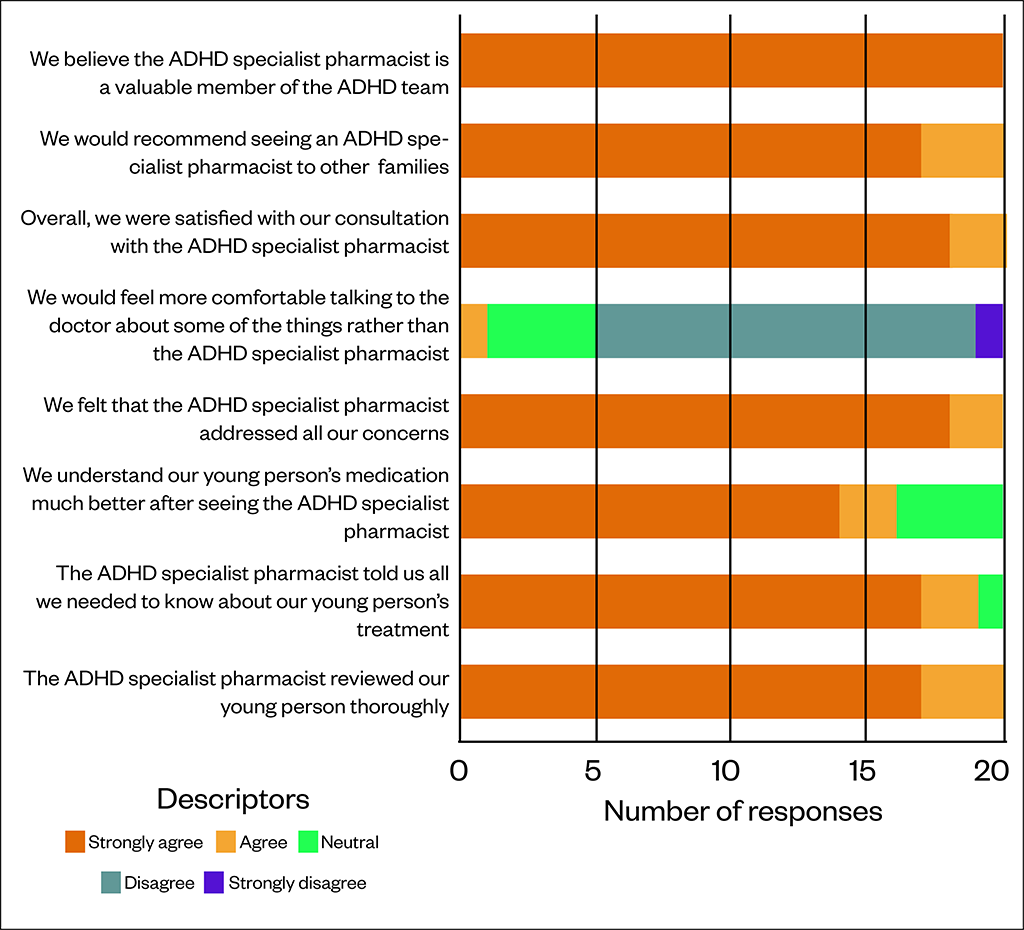
Figure illustrates the family and carer experience survey results for the pharmacist-led ADHD clinic. In total, 50 surveys were handed out, of which 20 were returned, resulting in a 40% response rate. In addition to the quantitative feedback displayed in Figure, the free text feedback was highly positive:
“The specialist pharmacist that we have seen has been incredibly helpful and supportive”.
“She had a lovely manner with my son, she listened to him and put him completely at ease”.
“We were initially a little concerned at not seeing a psychiatrist but our experience with the pharmacist has been excellent. She has listened and acted accordingly”.
“We have every confidence in the treatment our daughter has had”.
Figure: Family satisfaction survey of a pharmacist-led attention deficit hyperactivity disorder clinic
In total, 21 MDT staff were sent the survey to obtain feedback from healthcare professionals on the value of introducing the pharmacist role and 13 (62%; 4 psychiatrists, 3 psychologists, 3 administrative staff, 2 nurses and 1 social worker) responded to the electronic survey. Overall, 62% (n=8) indicated that the introduction of a pharmacist within the CAMHS team had been ‘extremely beneficial’, with 31% (n=4) indicating ‘very beneficial’ and one responder (7%) (n=1) indicating ‘beneficial’. All responders indicated that they had received support from the pharmacist within the CAMHS team.
While the full analysis of the two focus group discussions with the community CAMHS MDT has not been included in this report, a summary of the themes, summary notes and excerpts arising from the analysis is presented in Table 3.
Table 3: Summary outcome of focus group discussions with child and adolescent mental health services multidisciplinary team
| Themes | Summary notes | Excerpts |
| Staff burnout in CAMHS | Clinical participants reported that they undertook tasks which perhaps could be equally undertaken by another suitable member of staff (e.g. a pharmacist can provide specialist medical expertise where needed). | “At any point in time, we don’t have enough staff. We either have vacancies or we don’t have enough staff, even if every position was filled”. |
| Disparity in service provider and user expectations | Service users expected a smooth, progressive service following referral; however, they became frustrated when progression was lacking. Pharmacist consultations with service users provided an opportunity to discuss medicine choices. | “Its threshold of what’s urgent and what isn’t is probably very different in a clinician’s view compared to a parent who is sitting there really struggling”. |
| Invaluable contributions of independent prescribing pharmacists in CAMHS | Pharmacists within the team were described as reliable, accessible, competent, knowledgeable, friendly, adaptable, an asset and invaluable. Overall, the pharmacist’s contributions were not perceived as token, but rather a vital part of the CAMHS team. | “She has taken on some of the cases and doing assessments for ADHD client, so that helps the team as well for the doctor’s team”. |
| Mental health and wellbeing of service providers is equally important | The specialist pharmacists and, subsequently, independent pharmacist prescribers somewhat helped reduce the anxiety about workplace pressure post-integration into the CAMHS team. | “It was quite good when she arrived, writing prescriptions and that, with the intention that she can take over prescribing of the prescriptions which then takes the pressure off the doctors and administration staff”. |
Discussion
There has been limited experience in the UK of pharmacist independent prescribers working within the CAMHS setting. Over the past five years, the demand for CAMHS has increased significantly nationally, yet recruitment of medical staff has remained challenging[7,9]. To address the issue of rising demand and staff shortages in CAMHS, an innovative model to incorporate a specialist independent prescribing pharmacist into the community CAMHS team was developed, implemented and evaluated. The mixed method approach used in this evaluation facilitated triangulation of results. This study is the first to report service user experience of a specialist pharmacist within CAMHS.
The results in Tables 1 and 2 provide a suitable representation of the variety and breadth of duties, responsibilities, interventions and clinical outcomes that a dedicated pharmacist can undertake and deliver successfully, when appropriately trained and integrated into a community CAMHS team. Like the findings of Lyon and Brown, the results in this evaluation demonstrate that pharmacists can perform extended roles and do not have to limit their contributions to medicines-related issues if appropriately trained[20]. In this evaluation, the pharmacists undertook a DAWBA of the children and young people using a structured tool, which gathered psychiatric diagnostic data from families and teachers, and from young people themselves if aged 10 years or over[27]. Following children and young people’s DAWBA data gathering, a computerised summary was generated and reviewed by the psychiatrist to aid diagnosis. As noted in the results presented in this study, the pharmacist initially undertook this jointly then, subsequently, independently.
Evaluation of the pharmacist-led ADHD clinic showed that pharmacists were able to manage an ongoing caseload and adjust medication, which included starting, stopping and changing doses. In addition, pharmacists were able to monitor patient and drug parameters, and conduct necessary interventions either themselves or through referrals to other clinicians or services. This outcome supports the workforce model where skills within a healthcare team are harnessed and utilised resourcefully[6]. The responses from the family or carer survey of the pharmacist-led ADHD clinic were overwhelmingly positive, with 100% of respondents stating that they ‘strongly agreed’ that the pharmacist was a valuable member of the ADHD team. The 40% response rate achieved (20/50) from the family and carer survey could be considered low; however, this process was opportunistic with limited means of follow-up owing to the anonymous data collection approach employed[28]. For the purpose of this evaluation, this response rate was considered appropriate. In addition, analysis of the families and carer respondents’ characteristics was not feasible. Morton et al. suggests that rather than reviewing the response rate solely, consideration should also be given to the sampling strategy used, alongside contextual factors when critically assessing the response rate achieved[29].
All respondents expressed satisfaction with their clinic consultation and the pharmacist’s ability to address the issues discussed during the consultation. The free text responses in the survey commented positively on particular issues, such as resolution of queries; explanation of medicines; and liaising with other agencies or professionals, such as schools, community pharmacists and doctors in general practice. However, one family responded that they would have felt more comfortable consulting a medical professional rather than a pharmacist. It was not feasible to inquire further into this response to gain a better understanding. Simultaneous with the evolving roles of pharmacists within healthcare, the need to inform patients, other healthcare professionals and the public about the skills and expertise of pharmacists is vital to support efficiency in healthcare service delivery[6,14,15,30]. The positive findings from the satisfaction survey were reinforced during the focus group discussions with the MDT. Satisfaction following consultation with a specialist/independent prescribing pharmacist has also been reported elsewhere in other areas of healthcare[14–17,19,20,23,24].
The results from the electronic survey undertaken to identify the acceptance of MDT colleagues on the role of the pharmacist independent prescriber was extremely positive. In context, the 62% (n=13) response rate achieved was reasonable following a follow-up reminder email communication[28,29]. Overall, 92% (n=12) of the respondents thought that the introduction of the pharmacist role was either ‘very’ or ‘extremely beneficial’ for the team. The respondents cited a variety of support that they had received from the pharmacists in the focus group discussions, including advice relating to: prescribing; administration of medicines; legal and ethical issues; policy and guidance; and general clinical advice.
The positive impact of the pharmacist’s role was further affirmed by members of the community CAMHS MDT during the focus group discussions, in which they communicated specific descriptions of the pharmacists’ contributions and their value. The findings in this evaluation, such as support with specialist medicines used in ADHD, correspond to those detailed by O’Brian, where an independent prescribing pharmacist was integrated into the CAMHS ADHD team[19]. The findings from the focus group discussions indicated that MDT staff had experienced significant workload pressures for a long time and had complained of inadequate resources. Although the focus group discussions were undertaken across two different community CAMHS teams, interestingly, the themes around resources and workload pressures remained consistent. Discussions suggested that workplace pressure arises from an ever-increasing referral rate and a continuous loss in service provider capacity, leading to emotional stress and reduced morale within community CAMHS teams. MDT members highly valued their pharmacist colleague, with respect to their clinical input and as part of a supportive team, and indicated that pharmacist consultations with service users provided an opportunity to discuss medicine choices and respond to questions arising from an expert perspective.
An important theme from the focus group discussions was that the integration of the independent prescribing pharmacists had provided more capacity for the team to respond to the high referral rates, backlogs, and indirectly reduce the workload for individual team members, including doctors, psychologists, support workers and members of the administration team.
In addition to the clinical duties, inclusion of a pharmacist into the community CAMHS teams has provided additional benefits, including promoting cost-effective prescribing. For example, in one clinic base, a focus group participant reported that the pharmacist reviewed all children prescribed melatonin, which led to several prescribing changes, such as using a cheaper melatonin preparation and de-prescribing where appropriate. Other successes included resolving prescribing interface issues and supporting the implementation of the ADHD shared care protocol, thereby enabling GPs to prescribe ADHD medication as repeat medication. This supports seamless care across the interface, leading to improvements in the patient journey and in joint working between specialist services and primary care.
Since publication of the NHS England ‘Five Year Forward View’, the NHS has supported the development of several new clinical roles in response to increasing healthcare demand, and the recruitment and retention challenges of medical and nursing staff. Newly created roles for clinical pharmacists, physician associates, general practice assistants, nursing associates, mental health therapists and physiotherapists have been developed as a result [6,11,28,31]. In this project, extending the role of pharmacists in CAMHS utilises many of the principles being observed in other sectors of the NHS.
This evaluation demonstrates that pharmacists can be recruited, trained and integrated into an MDT CAMHS team. The model utilised shows that pharmacists can be managed and supervised by a consultant psychiatrist in a similar manner to a specialty doctor, although it should be noted that it is imperative to have dedicated and motivated consultant psychiatrists that are willing to invest their time in training, developing and supervising the pharmacist. Across healthcare it is becoming common to see non-medical prescribers working in strategic clinical areas[31].
Limitations
One of the limitations of this project is the sustainability of the model, based on the premise that if the pharmacist leaves their post, the process of recruiting and training as an independent prescriber in CAMHS would likely need to be repeated.
Limitations experienced in undertaking this evaluation included the limited capability to follow-up with non-responders of the survey. Most families were seen on one occasion during data collection, meaning there was limited opportunity to offer participation in the survey on a subsequent consultation. A longer duration of data collection may resolve this limitation. Lockdown restrictions as a result of the COVID-19 pandemic limited further data collection in pharmacist-led in-person ADHD clinics in March 2020. With limited knowledge about initial management of the pandemic, all secondary activities, including data collection, were halted.
Further work includes plans to extend the skills of the pharmacist to manage depression in children and young people, once their condition has stabilised. Studies have shown a pattern of increasing antidepressant prescription rates in children and young people in the UK[32,33]. A similar trend is observed in our local health economy. In the absence of shared care for managing depression in children and young people with primary care, it has led to an increased caseload and repeat prescribing workload for CAMHS psychiatrists. As the pharmacists gain more experience and competence, the complexity of cases may increase to include children and young people with comorbidities in addition to ADHD. There are also plans to develop a competency framework for a pharmacist-led ADHD clinic and to form a network of CAMHS pharmacists nationally.
Conclusion
This evaluation indicates that a pharmacist:
- can be recruited, trained and integrated into a multidisciplinary CAMHS team;
- can be managed and supervised by a consultant psychiatrist, in a similar manner to a speciality doctor;
- can develop a defined scope of practice that allows them to manage a delegated caseload of patients safely and effectively;
- can add value to the wider CAMHS MDT with their pharmaceutical expertise;
- can support medicines-related issues within the CAMHS pathway including interface problems;
- is highly accepted by other healthcare professionals;
- is highly accepted by children and young people and their families.
Important enablers for success in this project were: embedding the pharmacists into the community CAMHS establishment rather than the pharmacy structure — operationally managed by the consultant psychiatrist; undertaking the non-medical prescribing course while employed in this setting with the consultant psychiatrist acting as their DMP; and having motivated and dedicated pharmacists that were able to embrace challenge, yet understand and be aware of their scope of competence.
Acknowledgements
The lead author would like to acknowledge the late Ray Lyon, chief pharmacist at Sussex Partnership NHS Foundation Trust, for his support, advice and wisdom provided in this project and for his mentorship outside of the project.
Financial and conflicts of interest disclosure
A £10,000 grant was received from Health Education England to support any associated costs with education and training fees, network meetings and equipment. The authors have no other relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript.
No writing assistance was used in the production of this manuscript.
- 1Department of Health. No health without mental health: a cross-Government mental health outcomes strategy for people of all ages. Department of Health. 2011.https://www.gov.uk/government/publications/the-mental-health-strategy-for-england (accessed 3 Feb 2020).
- 2Department of Health. Closing the gap: priorities for essential change in mental health. Department of Health. 2014.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/281250/Closing_the_gap_V2_-_17_Feb_2014.pdf (accessed 17 Feb 2021).
- 3Department of Health. Future in mind. Promoting, protecting and improving our children and young people’s mental health and wellbeing. Department of Health. 2015.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/414024/Childrens_Mental_Health.pdf (accessed 17 Feb 2021).
- 4NHS England. The Five Year Forward View for Mental Health. NHS England. 2015.https://www.england.nhs.uk/wp-content/uploads/2016/02/Mental-Health-Taskforce-FYFV-final.pdf (accessed 17 Feb 2021).
- 5Department for Health and Social Care and Department of Education. Government Response to the Consultation on Transforming Children and Young People’s Mental Health Provision: a Green Paper and Next Steps. Department for Health and Social Care. 2018.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/728892/government-response-to-consultation-on-transforming-children-and-young-peoples-mental-health.pdf (accessed 17 Feb 2021).
- 6NHS England. NHS Long-term Plan. NHS England. 2019.https://www.longtermplan.nhs.uk/wp-content/uploads/2019/08/nhs-long-term-plan-version-1.2.pdf (accessed 17 Feb 2021).
- 7NHS Benchmarking Network. 2018 CAMHS benchmarking project report. NHS Benchmarking Network. 2018.https://www.nhsbenchmarking.nhs.uk/news/2018-camhs-project-results-published (accessed 17 Feb 2021).
- 8Frith E. Progress and challenges in the transformation of children and young people’s mental health care. Education Policy Institute. 2016.https://epi.org.uk/wp-content/uploads/2018/01/progress-and-challenges.pdf (accessed 17 Feb 2021).
- 9The Royal College of Psychiatrists. The Royal College of Psychiatrists’ pre-report summary of the 2019 Census. The Royal College of Psychiatrists. 2019.https://www.rcpsych.ac.uk/docs/default-source/news-and-features/media-centre/pre-report-census-summary-(2019)-final-mt2.pdf (accessed 17 Feb 2021).
- 10NHS England. General Practice Forward View. NHS England. 2016.https://www.england.nhs.uk/wp-content/uploads/2016/04/gpfv.pdf (accessed 17 Feb 2021).
- 11NHS England. Investment and evolution: A five-year framework for GP contract reform to implement The NHS Long Term Plan. NHS England. 2019.https://www.england.nhs.uk/wp-content/uploads/2019/01/gp-contract-2019.pdf (accessed 17 Feb 2021).
- 12Department of Health. Supplementary Prescribing by Nurses and Pharmacists within the NHS in England—a Guide for Implementation. Department of Health. 2003.https://webarchive.nationalarchives.gov.uk/+/http://www.dh.gov.uk/en/Publicationsandstatistics/Publications/PublicationsPolicyAndGuidance/DH_4009717 (accessed 17 Feb 2021).
- 13Latter S, Blenkinsopp A, Smith A et al. Evaluation of nurse and pharmacist independent prescribing. Department of Health Policy Research Programme Project 016 0108. University of Southampton. 2010.https://eprints.soton.ac.uk/184777/3/ENPIPfullreport.pdf (accessed 17 Feb 2021).
- 14Tinelli M, Blenkinsopp A, Latter S, et al. Survey of patients’ experiences and perceptions of care provided by nurse and pharmacist independent prescribers in primary care. Health Expect 2013;18:1241–55. doi:10.1111/hex.12099
- 15Stewart DC, George J, Bond CM, et al. Views of pharmacist prescribers, doctors and patients on pharmacist prescribing implementation. International Journal of Pharmacy Practice 2009;:89–94. doi:10.1211/ijpp.17.02.0003
- 16Hobson RJ, Scott J, Sutton J. Pharmacists and nurses as independent prescribers: exploring the patient’s perspective. Family Practice 2009;27:110–20. doi:10.1093/fampra/cmp070
- 17McCann LM, Haughey SL, Parsons C, et al. A patient perspective of pharmacist prescribing: ‘crossing the specialisms-crossing the illnesses’. Health Expect 2012;18:58–68. doi:10.1111/hex.12008
- 18Health Education England. Raising the Bar: Nurse Education Programme. End of Year Report April 2016 – March 2017. Health Education England. 2017.https://issuu.com/healtheducationengland/docs/nurse_education_programme_full_-_fi (accessed 17 Feb 2021).
- 19O’Brien C. O3 Developing a pharmacist prescribing role within child and adolescent mental health services (CAMHS). Arch Dis Child 2019;104:e2.23-e2. doi:10.1136/archdischild-2019-nppc.3
- 20Lyon R, Brown G. A naturalistic evaluation of the financial benefits of employing a mental health pharmacist to work with child and adolescent mental health services. Eur J Hosp Pharm 2017;25:48–52. doi:10.1136/ejhpharm-2016-001058
- 21Ibrahim K, Vogt C, Donyai P. Caught in the eye of the storm: a qualitative study of views and experiences of planned drug holidays from methylphenidate in child and adolescent ADHD treatment. Child Adolesc Ment Health 2016;21:192–200. doi:10.1111/camh.12156
- 22Ibrahim K, Donyai P. What stops practitioners discussing medication breaks in children and adolescents with ADHD? Identifying barriers through theory-driven qualitative research. ADHD Atten Def Hyp Disord 2018;10:273–83. doi:10.1007/s12402-018-0258-9
- 23Stewart D, George J, Bond C, et al. Developing and validating a tool for assessment of pharmacist prescribers’ consultations. Family Practice 2010;27:520–6. doi:10.1093/fampra/cmq034
- 24Stewart DC, George J, Bond CM, et al. Exploring patients’ perspectives of pharmacist supplementary prescribing in Scotland. Pharm World Sci 2008;30:892–7. doi:10.1007/s11096-008-9248-x
- 25Wong L. Focus group discussion: a tool for health and medical research. Singapore Med J 2008;49:256–60; quiz 261.https://www.ncbi.nlm.nih.gov/pubmed/18363011
- 26Hsieh H-F, Shannon SE. Three Approaches to Qualitative Content Analysis. Qual Health Res 2005;15:1277–88. doi:10.1177/1049732305276687
- 27Goodman R, Ford T, Richards H, et al. The Development and Well‐Being Assessment: Description and Initial Validation of an Integrated Assessment of Child and Adolescent Psychopathology. Journal of Child Psychology and Psychiatry 2000;41:645–55. doi:10.1111/j.1469-7610.2000.tb02345.x
- 28Fincham JE. Response Rates and Responsiveness for Surveys, Standards, and the Journal. AJPE 2008;72:43. doi:10.5688/aj720243
- 29Morton SMB, Bandara DK, Robinson EM, et al. In the 21stCentury, what is an acceptable response rate? Australian and New Zealand Journal of Public Health 2012;36:106–8. doi:10.1111/j.1753-6405.2012.00854.x
- 30Hindi AMK, Schafheutle EI, Jacobs S. Patient and public perspectives of community pharmacies in the United Kingdom: A systematic review. Health Expect 2017;21:409–28. doi:10.1111/hex.12639
- 31British Medical Association (BMA). New clinical roles in the NHS. British Medical Association. 2020.https://www.bma.org.uk/advice-and-support/nhs-delivery-and-workforce/workforce/new-clinical-roles-in-the-nhs (accessed 17 Feb 2021).
- 32Sarginson J, Webb RT, Stocks SJ, et al. Temporal trends in antidepressant prescribing to children in UK primary care, 2000–2015. Journal of Affective Disorders 2017;210:312–8. doi:10.1016/j.jad.2016.12.047
- 33John A, Marchant AL, Fone DL, et al. Recent trends in primary-care antidepressant prescribing to children and young people: an e-cohort study. Psychol Med 2016;46:3315–27. doi:10.1017/s0033291716002099
You may also be interested in

Specialist mental health pharmacist clinics in primary care: a service evaluation supporting integrated neighbourhood working

Stopping antidepressants in pregnancy linked to higher risk of mental health emergencies
