JL / The Pharmaceutical Journal
The summary care record (SCR) should be a community pharmacist’s best friend, so why are so many routinely ignoring it? This is the question that is plaguing NHS bosses as they press ahead with the digitisation of the health service in England.
The SCR, which could first be used by pharmacists as part of a pilot in 2014, is a vital part of NHS attempts to integrate care, break down barriers and ensure safer and more timely patient treatment. The record, which lists a patient’s medication history and any allergies or adverse events they have had in the past, has taken years to put in place, and is the first stage of the government’s aim to have fully transferable, ‘real-time’ electronic health records in every care setting by 2020[1]
.
The SCR is viewed on average once every four seconds; however, an analysis of data by The Pharmaceutical Journal shows that more than 85% of community pharmacies did not access the SCR at all over a typical week (see Figure), while just over 1 in 10 (1,261) of 11,659 pharmacies that are signed up to use the SCR accessed it more than twice. There were nine ‘super users’ — pharmacies that accessed the SCR more than 100 times during the same week.
A survey of more than 1,200 pharmacists carried by The Pharmaceutical Journal in the summer of 2018 supports these findings, and shows that 40% of pharmacists do not have access, or have never accessed, the SCR versus 34% accessing it once a week or more, 11% a few times per month and 15% once per month or less. This is concerning — particularly as lobbying continues to grant community pharmacy access to the full patient record.
Mohammed Hussain, a pharmacist and senior clinical lead at NHS Digital, the national provider of information, data and IT systems for commissioners, analysts and clinicians in health and social care in England, says: “The numbers do vary from month to month. You have a very long tail of people who have used the SCR once or twice each month, then you have those in the middle who are periodic users. Then you can see there are some who have really embedded it in their practice, using it 50—100 times a month.”
Hussain and his team have searched for patterns of which pharmacies are using the SCR most often, but he says those in the top ten are a mixed bag. They include independent pharmacies and multiples, those with city centre premises and those co-located with GP surgeries.
Data analysis shows that all types of pharmacies can benefit from access to the summary care record
Perhaps unsurprisingly, four of the top ten heaviest users are online distance-selling pharmacies. “What [this data analysis] shows is that all types of pharmacies can benefit,” he says.
But Hussain wants pharmacy to use SCR first rather than picking up the phone to call the GP surgery. “One of the myths is that pharmacists say they don’t need [the SCR] because they have worked without it, but if you ask them how often they phone the GP … you find a lot of these could be solved by looking at the SCR.”
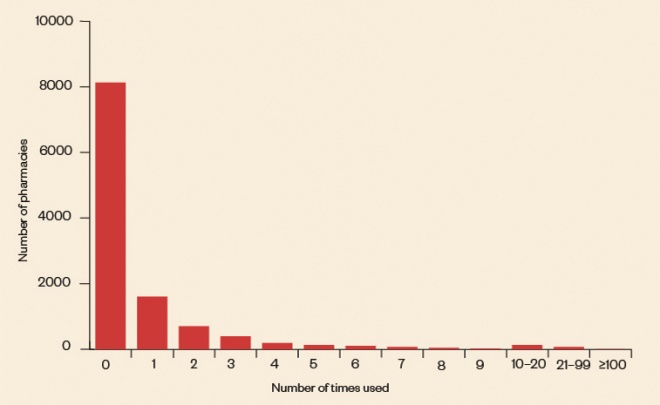
Figure: How often are pharmacists accessing the summary care record?
Source: NHS Digital, SCR in community pharmacy usage monitoring 2018/2019
More than 85% of community pharmacies did not access the SCR at all over a typical week, while just over 1 in 10 (1,261) of 11,659 pharmacies that are signed up to use the SCR accessed it more than twice, an analysis of NHS data by The Pharmaceutical Journal has revealed
Others have also identified a problem. Earlier in 2018, the Royal Pharmaceutical Society (RPS) surveyed members following a high number of calls to its professional support teams querying aspects of using the SCR. The respondents to the survey mostly said they did use the SCR, but only 56% said they accessed it in non-urgent cases, while 41% said they would still contact a GP rather than use the SCR.
As a result, the RPS has published updated guidance and a series of videos on possible scenarios where pharmacists might consider using the SCR in dealing with a patient to counter confusion and encourage its wider use.
Ivana Knyght, who leads the RPS professional development and support service, says: “This is an area where more clarity is needed, and we wanted to tackle the specific scenarios where members were most uncertain, such as consent by proxy or on an ongoing basis.”
Sibby Buckle, chair of the RPS Digital Forum Group, says one very common response from pharmacists when asked about use of the SCR is that it just does not contain enough information. “For some pharmacists, their personal medical records are almost as good, if not better, than the SCR,” she says.
“So they are only going in when they are doing emergency supplies as they have no need otherwise — they have the information in their own records.”
Fear of the unknown
Buckle adds that another common reason for low-level use could be that the “fear of God” was put into a lot of pharmacists about whether they actually had the right to access it when they were originally trained in its use.
In 2015, several national newspaper articles warned that supermarkets and the big multiples would be able to access patient data via the SCR and use it for marketing purposes. NHS England was forced to reassure the public that data protection legislation would not allow this to happen.
Hussain acknowledges this may have been a barrier at the start when the job of the SCR was to provide information in emergency scenarios, but he says much of the language of governance has now been altered to reflect its changing use.
I went to the summary care record training and it did leave you feeling ‘what am I letting myself in for?’
But the original approach does seem to have had a lasting effect. Nat Mitchell, a pharmacist at Allison & Sons Pharmacy in Cockermouth, Cumbria, agrees that the perception of risk has deterred some pharmacists from using it.
“I went to the training and it did leave you feeling ‘what am I letting myself in for?’ I would always use it if I need to but I can see why some people were put off.”

Source: Courtesy of Nat Mitchell
Nat Mitchell, a pharmacist at Allison & Sons Pharmacy in Cumbria, admits that he was skeptical of the summary care record when he did his training
Buckle says that where she works in a city centre pharmacy in Nottingham with roughly 50% new customers, she regularly uses the SCR but it would be so much more useful if it contained extra information.
Currently, the basic SCR is limited to allergies and adverse reactions (81% of those responding to the RPS survey said they would use it to check for penicillin allergy), acute medicines used in the past 12 months, repeat medicines and recently discontinued medicines.
However, advocates of greater patient access want to see blood test results, vaccination history and diagnoses made available on the SCR, as well as pharmacists’ ability to write on to the record.
Additional information
The introduction of the ‘summary care record with additional information’ (SCRAI) now means that GPs can ask a patient if they want to consent to have more of their record available to other healthcare professionals, including pharmacists. This extra information can include immunisations, significant medical history, end-of-life care information and reasons for the prescription of certain medicines.
From 1 July 2017, the GP General Medical Services contract required GPs to identify frail patients and promote inclusion of extra information on their SCRAI by seeking patient consent. But the rate at which extra information is added to the SCR varies between clinical commissioning groups (CCGs).
“In some areas there has been a real push from the CCG for some patients to have [the SCRAI],” says Hussain, whose local pharmaceutical committee (LPC) in West Yorkshire has been doing some work to promote it.
Nick Kaye, a pharmacist in Penryn, Cornwall, and a member of the National Pharmacy Association board, says the SCR was a great first step but pharmacists just want more information included.
“The biggest change we could have would be for pharmacists to have write access to the record. [The SCR] should be about connecting all of primary care,” he says.
“The one thing the SCR was very good at was that it was opt-out rather than opt-in. The additional information stuff hasn’t necessarily worked in the same way. I’ve not heard about it in my CCG.”
Kaye adds that working in a popular tourist spot means the SCR can be incredibly helpful but “sometimes the easiest option is just to ring the GP surgery”. He also points out that a real headache for community pharmacy in using the SCR is locum access.
If you could see blood test results on the SCR, you might do something different in the advice you give
David Broome, a member of the Pharmaceutical Services Negotiating Committee’s board and community pharmacy IT group, says he is a big advocate of the SCR but in his practice in Bramhope, West Yorkshire, he does not find the need to access it that often.
“I definitely think more pharmacists would use an enhanced version of the SCR that contained more information. For example, if [you] could see blood test results you might do something different in the advice you give and it would cut down on duplication.
“I had someone recently who came in asking for advice on travel vaccines and I had to contact the GP to find out what jabs they had had because they didn’t know.”
Promoting widespread use
So far, the implementation of the SCR has been a fantastic proof of concept, but as pharmacists move to more clinical and patient-focused work, it needs to keep pace across the board.
Hitesh Patel, chief officer of the City and Hackney LPC, says he has been pushing locally for additional information on the SCR but is getting very little buy-in with his local CCG or GPs. “They all agree it’s a good thing but nothing gets done about it,” he complains.
He adds that, by contrast, some CCGs have implemented a blanket switch-on of additional information.
“It would be great for management of long-term conditions because at the moment our hands are tied as we don’t [have access to find out] what the diagnosis of the patient is,” he says.
Some improvements have been made since the SCR was launched — shortcuts to access it, such as some IT providers working on one-click systems, and the NHS Urgent Medicine Supply Advanced Service has driven greater use, but it needs more champions and advocates to encourage more widespread uptake, says Hussain.
“We need pharmacists to embed it in their practice and to involve the whole pharmacy team in using it,” he says.
Hussain believes it will be inevitable that pharmacists will get full read/write access to full patient records at some point — whether through the SCR or a parallel system — and it is vital that pharmacy is a part of that discussion.
But, he says, “the business case for read/write access becomes more challenging to make if low numbers are using it overall”.
“In community pharmacy we haven’t got it quite right in terms of professional behaviour and looking at the SCR first,” adds Hussain.
Box 1: Do you use the summary care record regularly?
YES
We access high numbers of summary care records (SCRs) because we have high numbers of new patients. It is a tool to obtain clinical information about new patients without relying on the individual to provide exact information.
Jamie Urqhart, superintendent pharmacist, Now Pharmacy
YES
Being located in the city centre, not in close proximity to GP surgeries, we are often faced with challenges in locating prescriptions, confirming medication records and checking over-the-counter (OTC) queries at our busy OTC counter.
Qaisar Sheikh, pharmacist, Rimmington Pharmacy, Bradford
YES
We use SCR for the NHS Urgent Medicine Supply Advanced Service and other emergency supplies, clarifying current medication, checking for changes in medication and checking doses. It may be that we use it more than others because we are [in the] city centre and don’t have any GPs near us.
Martin Bennett, superintendent pharmacist, Wicker Pharmacy, Sheffield
NO
We tend to have quite regular patients and we have quite good records on the computer already — so we only use it if someone is new or they got their prescription elsewhere. And we do a lot of deliveries so it would be unusual that a patient would be in the shop to consent.
Amanda Smith, pharmacy manager, Heath Pharmacy, Halifax
Box 2: When will pharmacies get access to full patient records?
The Department of Health and Social Care (DHSC) has said there is a continued commitment to enable read/write access to patient primary care records.
NHS Digital is working on projects that will provide a system-wide method for pharmacists working in any clinical setting to be able to record information so that it can be seen by anyone providing primary medical care. But this will depend on different systems across the NHS working together.
A spokesperson for the DHSC said: “We are still committed to giving community pharmacies read/write access to patient primary care records, but this is a complex issue and we’re working to address a number of challenges.”
Jignesh Patel, pharmacist independent prescriber at Rohpharm Pharmacy in London, has been taking part in a pilot of EMIS Web for Pharmacy that allows him to write to the patient record and see a full history of medication and diagnostic results — something he describes as a “game changer”.
He recently presented the case for greater interoperability between GP and pharmacy IT systems to the Westminster Health Forum and is working with the Professional Records Standards Body, a collaborative body that works to define standards needed for good care records, to improve pharmacy access to patient records.
“What is the point of the SCR when you have that information in your personal medical record?” he says.
“Now I can look at investigations, diagnoses and I can pick up if people are not taking their medications.”
“We have got a long way to go with IT. But it would make such a massive difference — you wouldn’t have to write letters or fax information to the GP, there would be an audit trail and you could identify problems, find alternative treatments, dose adjustments. [It would make] such a big difference.”
References
[1] House of Commons Library. April 2016. A paperless NHS: electronic health records.


