Courtesy of Jonathan Buisson
The Medicines and Healthcare products Regulatory Agency (MHRA) has estimated that implementing the Falsified Medicines Directive (FMD) in the UK could cost almost half a billion pounds to implement over the next ten years, depending on how the directive is introduced.
But there is no assessment of the potential costs to community pharmacy of FMD adherence in its consultation on implementing the directive, which comes into force on 9 February 2019.
The MHRA said this absence is owing to the fact that the consultation focuses on areas of FMD where the UK has the legal flexibility to make changes to the delegated regulation. There is no flexibility on how community pharmacies implement FMD. Instead, the consultation concentrates on the impact of FMD on wholesalers, parallel distributors and the so-called ‘Article 23 institutions’: non-healthcare institutions who supply medicine to the public, such as care homes, opticians and prisons.
The Pharmaceutical Services Negotiating Committee (PSNC) told The Pharmaceutical Journal that, as part of the UK FMD Working Group for Community Pharmacy, it was continuing to work on an assessment of the costs of implementing and operating FMD for pharmacy contractors. The assessment would, they said, be used in forthcoming negotiations with the Department of Health and Social Care and NHS England. In February 2018, Alastair Buxton, head of NHS Services at the PSNC, said that the body would “work to ensure that contractors’ FMD-related costs are recognised in future NHS funding settlements”.
A large part of the consultation considers whether wholesalers should be required to verify and decommission medicines on behalf of all Article 23 institutions, or whether some or all of these institutions should take on this responsibility themselves. An impact assessment estimates the ten-year cost of the former option at £25.7m, and the latter option at £473.2m.
The MHRA says the first option would present the best value for money.
The consultation also invites views on possible sanctions for non-compliance within the supply chain. The MHRA said the government is “minded to move to an approach that would use a mixture of both criminal and civil sanctions”, with non-compliant bodies or persons initially being faced with civil sanctions including written warnings and civil fines, and only the most serious, intentionally fraudulent, breaches being subject to criminal sanctions.
Respondents are asked for their views on the most effective way of enforcing FMD across the supply chain.
The Royal Pharmaceutical Society (RPS) will be responding to the consultation and has invited its members to contribute to the response.
Gino Martini, chief scientist at the RPS, said: “We would urge people to get actively involved in this conversation, because it will affect a significant part of the supply chain.
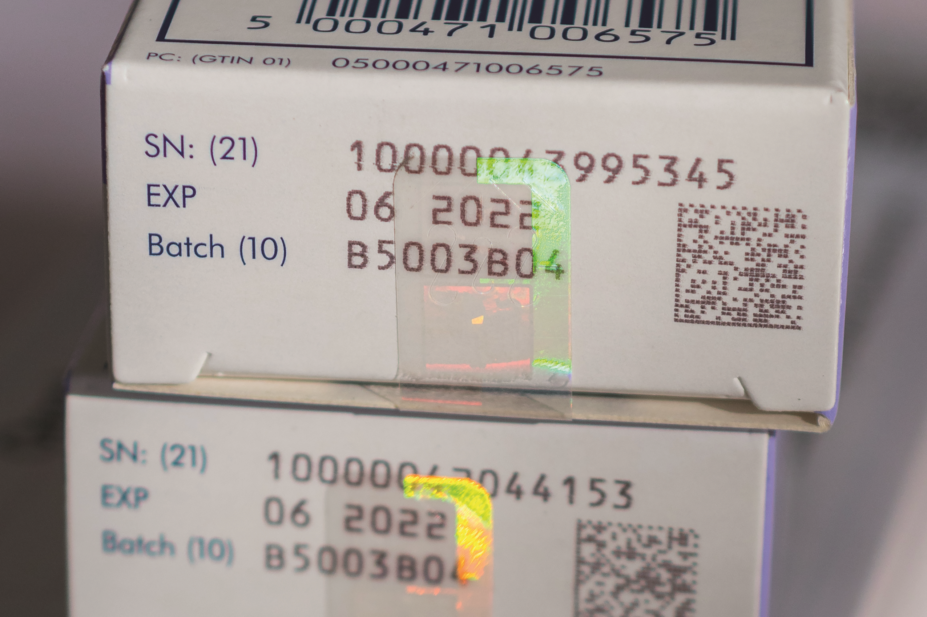
“Globally, counterfeit medicine levels reached their highest ever levels during 2017. Anything that prevents counterfeit medicine coming into the UK is a good thing.”
The consultation documents are available to download from the MHRA website. The consultation closes at 15:00 on 23 September 2018.


