London Joint Working Group on Substance Use and Hepatitis C
Results of a four-month pilot project have found that more than half (53%) of patients using pharmacy-based needle exchange services tested positive for hepatitis C (HCV) antibodies. Of these, 47% were previously unaware that they were HCV antibody-positive.
The London Joint Working Group (LJWG) on Substance Use and Hepatitis C pilot took place across nine London community pharmacies from October 2017 to March 2018. Those found to be HCV antibody positive (95 out of 178 patients tested) were referred to secondary care services for further assessment and treatment.
Of those referred for secondary care treatment, 84% said they would in future prefer to receive treatment through a community pharmacy.
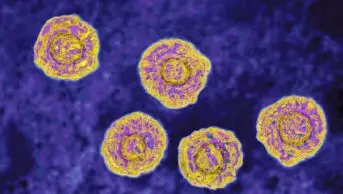
Public Health England (PHE) estimates that around 160,000 people live with hepatitis C across the country, and that around half of these may be unaware that they carry the virus. Around a quarter (41,500) of those living with the virus are in London. According to PHE, around half of people who inject drugs in London carry the virus.
Pharmacy minister Steve Brine joined representatives of the LJWG at Portmans Pharmacy in Pimlico, central London, one of the pharmacies involved in the pilot, to highlight the project’s findings. “We are working hard to eliminate hepatitis C as a public health issue by 2025, five years ahead of the World Health Organization target,” he said.
“Innovative testing initiatives in the community are essential if we are going to diagnose and treat everyone who has hepatitis C, a virus that disproportionately affects some of the poorest and most marginalised groups in society.”
The LJWG is a multidisciplinary team of clinician and patients working towards the elimination of hepatitis C in drug users, and those engaged in drug services, in London. Suman Verma, consultant hepatologist at Chelsea and Westminster Hospital and co-chair of the LJWG said, that the UK now has the treatments needed to eliminate hepatitis C as a serious public health concern across the nation.
“Offering free, accessible hepatitis C testing in community pharmacies is a more patient-centric way of engaging with a group of vulnerable, young people where hepatitis C prevalence and risk of transmission is high but, due to personal and social circumstances, engagement with community drugs services or healthcare services in general is poor and sporadic,” Verma said.
“By offering hepatitis C testing in community pharmacies, we will be transforming and saving lives, as well as preventing further virus transmissions. This pilot project has the potential to be developed further to encompass the provision of hepatitis C antiviral treatment directly in the community pharmacies for this vulnerable, socially marginalised, at-risk population.”
The full report is available from the LJWG website.
You may also be interested in

How we treated more than 100 hepatitis C patients at pharmacist-led clinics in North Wales

Community pharmacies have an essential role in sustaining the elimination of hepatitis C in England