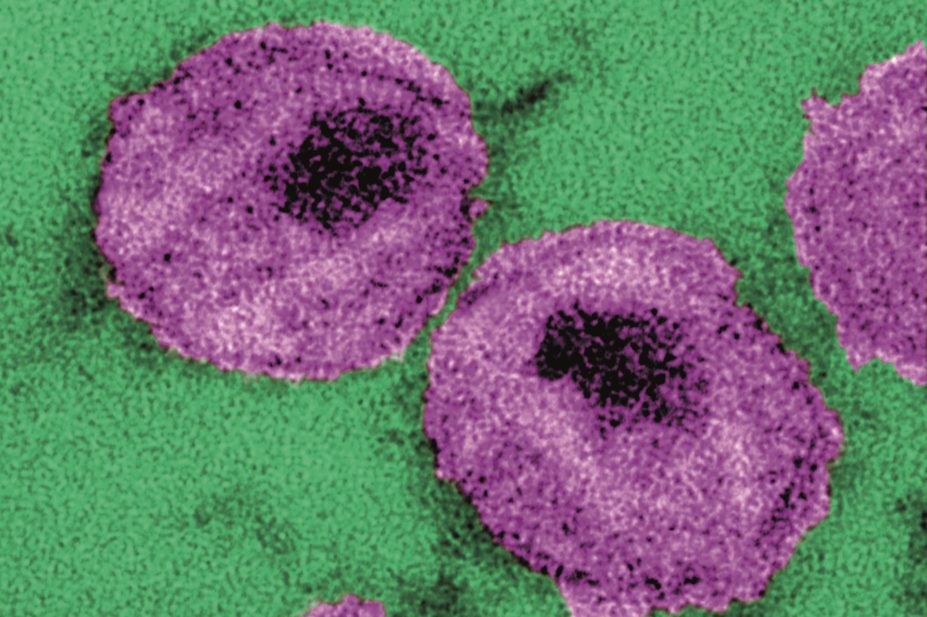
CDC / Dr. A. Harrison; Dr. P. Feorino
Treating men deemed at high risk of becoming HIV positive with daily antiretroviral medication is extremely effective at preventing new infections, according to the results of a trial carried out at 13 sexual health clinics in England.
Researchers at the Medical Research Council (MRC) clinical trials unit at University College London recruited 544 high-risk participants, defined as men who said they regularly had unprotected sex with men.
They were randomised to receive a daily tablet that contained tenofovir disoproxil fumarate (245mg) plus emtricitabine (200mg) (a combination known as Truvada; Gilead Sciences) either immediately or after a deferral period of one year.
The results of the study show that daily Truvada treatment was highly effective at preventing new HIV infections. Significantly, there was no increase in the occurrence of other sexually transmitted infections, ruling out the concern that some participants who took pre-exposure prophylaxis (PrEP) might adjust their behaviour based on confidence that their risk was lowered.
PrEP was already known to be effective when subjects were compliant. “But the findings are highly significant since this was the first real world study,” says Kenneth Mayer, director of HIV prevention research at the Beth Israel Deaconess Medical Center, Boston, Massachusetts.
The participants were men who have sex with men who accessed genito-urinary medicine services. They were randomised to receive PrEP immediately or be placed in a queue where they would receive all other prevention services (e.g. condoms, counselling, access to post-exposure prophylaxis) and were told they would have access to PrEP after a year if it was shown to be effective. The rate of HIV infection was decreased by 86% among those who received immediate access to PrEP.
“The data show that in the real world, high-risk people can be sufficiently adherent to PrEP to make it very effective in decreasing HIV risk,” says Mayer.
The participants in the PROUD study were much more likely to have had rectal infections and to have used post-exposure prophylaxis than was the overall population of men who have sex with men attending sexual health clinics. Nevertheless, the gap between HIV incidence was surprising.
According to researcher Sheena McCormack and colleagues: “The difference suggests that the PROUD study population was highly selective, despite broad eligibility, and that the offer of PrEP generally attracts those men who are most likely to benefit from it.
“This finding is highly encouraging for PrEP implementation, although quantifying the likely demand in the UK remains challenging,” she adds.
The impressive reduction in HIV incidence in people taking PrEP, without a measurable increase in other sexually transmitted infections, “is reassuring for clinical, community, and public health stakeholders”, argue McCormack and colleagues, whose findings were published in The Lancet
[1]
on 10 September 2015.
In February 2015 a similar trial in France, IPERGAY, reported the same 86% reduction in HIV incidence. “National health services are under financial constraints, but they cannot afford to ignore the results of PROUD and IPERGAY, which strongly support the addition of PrEP to the current standard of prevention for men who have sex with men at risk of HIV infection,” conclude the authors.
References
[1] McCormack S, Dunn DT, Desai M et al. Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet 2015. doi:http://dx.doi.org/10.1016/S0140-6736(15)00056-2 7.


