The liver is the largest internal organ of the human body and has a dual blood supply. The hepatic portal vein delivers blood from the intestine to be processed before being returned to the general circulation while the hepatic artery, which branches from the aorta, supplies the liver with oxygen. The individual functional units of the liver are called lobules. These are hexagonal arrangements of tissue formed around a central vein. A branch of the hepatic artery, a branch of the hepatic portal vein and a bile duct are situated at each edge of these lobules. Blood from each lobule flows into large capillary spaces (sinusoids), which are connected to the central vein.
The liver performs numerous essential functions of metabolism, synthesis and storage, including:
- Detoxifying waste products (eg, nitrogenous waste), hormones, drugs and other
- xenobiotics
- Producing plasma proteins (eg, albumin)
- and clotting factors
- Storing glycogen, fats, iron and vitamins
However, despite these numerous functions, there is little cellular specialisation — hepatocytes perform a wide variety of metabolic and secretory roles, and phagocytic activities are carried out by Kupffer cells. When the liver comes into contact with toxins or viruses, it undergoes inflammatory (hepatitis) or fatty (steatosis) changes, or both (steatohepatitis). These changes are usually reversible — the liver can regenerate — but if the cause of the initial insult is not addressed damage can progress to fibrosis (scarring and thickening of the smooth liver tissue) and cirrhosis of the liver (see Definitions panel), which result in complications, such as ascites (fluid in the abdomen), portal hypertension and oesophageal varices. Varices form when blood from the intestine cannot flow through the hardened liver and can result in internal bleeding (indicated by vomiting blood or tarry stools) if they burst.
Cirrhosis of the liver also increases the chances of a patient developing hepatocellular carcinoma, a condition with a life expectancy of no more than six months.
Use of the term “hepatitis” needs to be qualified because numerous factors can trigger inflammation, including:
- Alcohol
- Viruses (A-E)
- Drugs (including herbal remedies)
- Auto-antibodies
- Insulin resistance
Diagnostic tests
A number of blood tests are used to assess liver function, but tests cannot be used to quantify this in the way that serum creatinine is used to assess renal function.The term “liver function tests” (LFTs) may be viewed as a misnomer because some of the markers reflect liver damage rather than the ability of the liver to perform its usual functions. Further tests that may be requested during the investigation of liver dysfunction include ultrasound and biopsy.
Blood tests
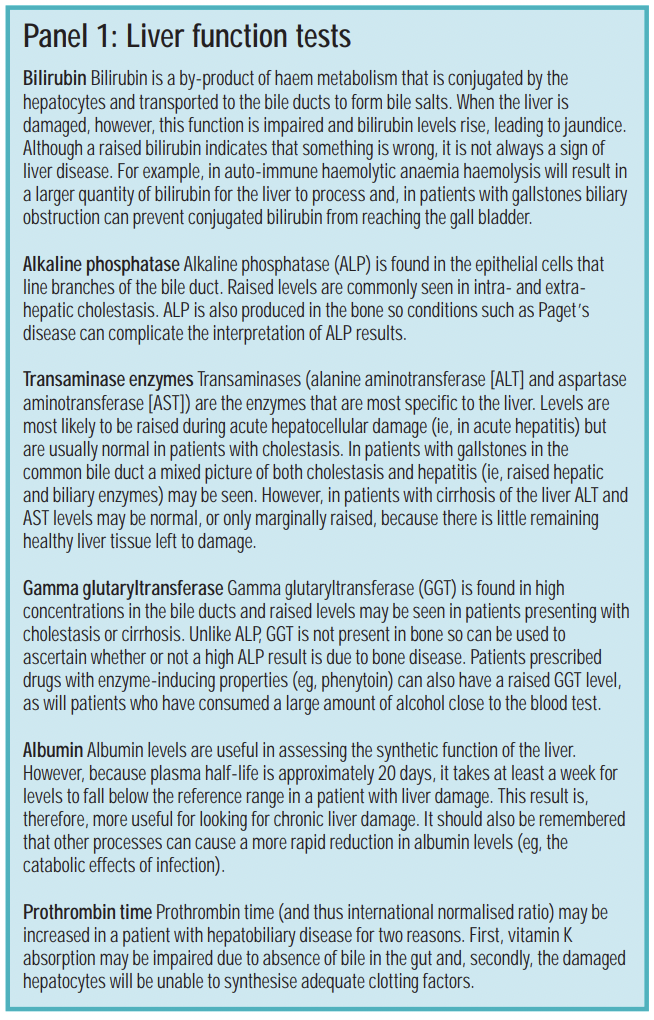
The tests that are commonly referred to as LFTs include measuring bilirubin, alkaline phosphatase (ALP) and albumin (see Panel 1). These help paint a picture of the type and cause of liver damage.
A “full liver screen” is also performed to help find the cause of liver disease. This will include looking for viruses, auto-antibodies (indicative of autoimmune hepatitis) and alfa feta protein (a tumour marker).
Biopsy
Liver biopsy may be used to diagnose the cause of liver disease and assess the
damage (eg, to differentiate between hepatitis and cirrhosis). The procedure is usually performed as a day case, under local anaesthetic. The most common complications are bile leaks and bleeding.
Ultrasound
A liver ultrasound scan will identify extrahepatic duct dilation and can identify abnormalities, such as cysts and tumours. It can also help describe the appearance of the liver — for example, if a patient has a fatty liver, the echo is bright — and will establish whether a patient presenting with abdominal swelling has ascites.
Acute hepatitis
The manner in which a patient presents with acute hepatitis depends on the cause. In addition, some patients with acute hepatitis may be asymptomatic. However, in all cases the potential exists for a patient to develop acute liver failure, which can result in:
- Jaundice
- Hypoglycaemia
- Hepatic encephalopathy (characterised by disturbance of consciousness that may progress to coma, psychiatric changes, flapping tremor and breath odour, and caused by the accumulation of waste products that the liver would normally remove)
- Haemorrhage
Acute liver failure can be life-threatening and a liver transplant may be required. This article looks at some of the non-viral causes of acute hepatitis, however, it is beyond the scope of this article to discuss the management of chronic liver disease.
Alcoholic hepatitis
Excessive alcohol consumption — an increasing problem in the UK — can lead to a spectrum of histopathological changes, ranging from steatosis and steatohepatitis to fibrosis and cirrhosis of the liver.
Between 20 and 40 per cent of heavy drinkers will develop serious liver disease. Some of them will present with acute alcoholic hepatitis, characterised by fever, tender enlarged liver and leukocytosis in association with other clinical and laboratory features of liver failure. Serum transaminases, gamma glutaryltransferase, ALP, bilirubin and prothrombin time can all be raised in patients with alcoholic hepatitis. In others, the first sign of a problem will be symptoms of either liver cirrhosis or hepatocellular carcinoma because, up until presentation, the patient has had compensated liver disease.
Alcoholic hepatitis is thought to involve a complex interaction between ethanol metabolism, and inflammatory and immune processes. Ethanol oxidation generates free radicals, resulting in oxidative stress. Tumour necrosis factor-α levels have been reported to be raised in these patients and the biological activities of this cytokine are altered in alcoholic liver disease, favouring inflammation and apoptosis rather than hepatocyte proliferation.
Hyperbilirubinaemia and prolongation of prothrombin time (PT) have a prognostic value in alcoholic hepatitis. The following formula (Maddrey’s discriminant function; DF) has been used to assess the severity of the condition and has been validated in several studies:1
DF = 4.6 [PTpatient – PTcontrol(s) + Serum bilirubin]/17.1
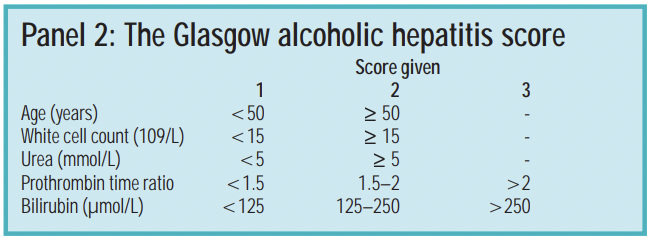
A value greater than 32 effectively predicts a one-month mortality of 50 per cent. However, more recently, another tool, the Glasgow alcoholic hepatitis score (GAHS), has been developed to identify patients at greatest risk of death during hospital admission and is described in Panel 2. Patients with a score less than 9 on day 1 were shown to have a 28-day survival of 87 per cent, whereas if GAHS is greater than or equal to 9, survival was reduced to 46 per cent.2
The mainstay of treatment is abstinence from alcohol and supportive care. However, in patients with jaundice or a DF greater than 32, or both, or in those with a GAHS greater than or equal to 9, intensive clinical management should start from admission to hospital. Specific treatments include nutritional therapy and corticosteroids.
Nutritional therapy
Malnutrition in patients with alcoholic hepatitis has been shown to correlate closely with mortality. Nutritional support by mouth or by nasogastric tube (at least 25kcal/kg/day) should be started as soon as possible to support the metabolic functioning of the liver.
Corticosteroids
Corticosteroids are used for their anti-inflammatory and immunosuppressant properties. However, studies have produced conflicting results — three meta-analyses have shown a beneficial role in alcoholic hepatitis, whereas one has questioned their efficacy.3,4
It should be noted, however, that some of the initial trials, which showed no benefit, may have included patients without alcoholic hepatitis and all the trials preceded the validation of the GAHS. Two trials containing patients with the worst prognosis (a DF>32 or encephalopathy, or both) showed a survival benefit in steroid-treated patients.5,6 It should also be noted, when looking at studies, that patients with alcoholic hepatitis form a heterogeneous population and it can be difficult to differentiate between severe acute alcoholic hepatitis and decompensated liver disease on a background of cirrhosis.
For patients with severe alcoholic hepatitis (DF>32), the American College of Gastroenterology recommends prednisolone 40mg daily for four weeks, followed by a gradual reduction to zero.
Patients with concomitant pancreatitis, gastrointestinal bleeding, renal failure or active infection were excluded from the trials and steroids should be avoided in these patients.
Pentoxifylline
Pentoxifylline is a TNF-α inhibitor. In one study, 101 patients with severe alcoholic hepatitis were randomised to receive either pentoxifylline 400mg tds or placebo for four weeks. Pentoxifylline was
associated with improved short-term survival. The benefit appeared to be related to the reduced risk of developing hepatorenal syndrome (a condition where renal failure develops secondary to liver disease).7
Autoimmune hepatitis
Mainly affecting young females, autoimmune hepatitis is a relatively uncommon condition where patients present with fatigue, right upper quadrant pain, polymyalgia or arthralgia and abnormal LFT results. Approximately 20 per cent of patients will have another form of autoimmune disease, such as rheumatoid arthritis. Detection of antinuclear antibodies, antismooth muscle antibodies and high titres of immunoglobulins aids diagnosis. If the condition remains untreated, patients may develop cirrhosis of the liver.
Initial treatment involves prednisolone 50mg daily, which is reduced to a maintenance dose. This is followed by the introduction of azathioprine (1.5–2mg/kg/day), used for its steroid-sparing effects — it allows the dose of the steroid and, therefore, associated side effects to be reduced. Patients may also require ciclosporin.
Because many patients require long-term corticosteroid therapy, bone scans and measures to prevent osteoporosis should be implemented.
Drug-induced hepatitis
Various drugs, (eg, carbamazepine, statins and ibuprofen), can cause hepatitis. Patients who develop drug-induced hepatitis often experience symptoms similar to those seen in acute viral hepatitis (see Part 2 [to be published on 19 April]) but incidence is rare. Patients can have abnormal
LFT results with no clinically significant adverse effects when prescribed drugs such as isoniazid and anticonvulsants.
Although adverse drug reactions are a relatively uncommon cause of hepatitis, they should always be considered as a possibility until tests reveal another cause. Enzyme inducers, such as alcohol and rifampicin, increase the risk of hepatotoxicity with other drugs. For example, alcohol depletes glutathione stores, so that if paracetamol is taken N-acetyl-p-benzoquinoneimine (a product of
paracetamol metabolism that causes hepatocellular necrosis) accumulates.
Penicillins, especially flucloxacillin, can cause a mixed cholestatic hepatitis and this adverse drug reaction may not be seen until a few weeks after the course of antibiotic has been completed.
Pharmacists should also be aware of hepatitis induced by herbal products. For example, in 2002, kava was banned after reports of hepatotoxicity.
The treatment of patients who present with drug-induced hepatitis requires withdrawal of the drug and supportive therapy.
Specific antidotes are only available for paracetamol and iron. Once the patient has recovered, the condition that the offending drug was being used to treat usually needs to be re-addressed. However, there is potential for cross-sensitivity between drugs with similar chemical structures so, for example, patients who develop jaundice due to chlorpromazine should avoid all phenothiazines.
Non-alcoholic fatty liver disease and steatohepatitis
Non-alcoholic fatty liver disease (NAFLD) encompasses a spectrum of liver diseases where patients have steatosis that occurs in the absence of excessive alcohol consumption. It is now considered to be the most common liver problem in the western world, where it is estimated to affect up to 30 per cent of the population.
NAFLD includes non-alcoholic steatohepatitis (NASH), in which the accumulation of excess fat in the liver cells is associated with inflammation. A liver biopsy is required to make a definitive diagnosis and to distinguish between NAFLD and NASH.
Insulin resistance has been observed in up to 98 per cent of patients who have NAFLD. People with metabolic syndrome (characterised by obesity, type 2 diabetes, hypertension and hypertriglyceridaemia) are at risk of developing a fatty liver, which may progress to steatohepatitis and, ultimately, cirrhosis.
A diagnosis is usually made after other common causes (eg, viruses, autoimmune disease and alcoholism) are excluded. Many patients are asymptomatic and the disease is only discovered when abnormal LFTs are detected during routine tests. Some are not diagnosed until they present with the complications of hepatic cirrhosis, such as ascites or variceal bleeding.
There is no established pharmacological therapy for NAFLD or NASH. Insulin sensitising therapy (in the form of metformin and thiazolidinediones) has been investigated in several phase II and III studies. In one study,8 metformin resulted in normalisation of LFT results, but the effect on liver histology was not assessed.
A large phase III study of metformin for NASH is currently in progress. A number of small studies have shown that thiazolidinediones improve histological data in patients with NAFLD. However, in two of these studies there was at least one case of hepatotoxicity necessitating the discontinuation of the drug.
The pharmacist’s role
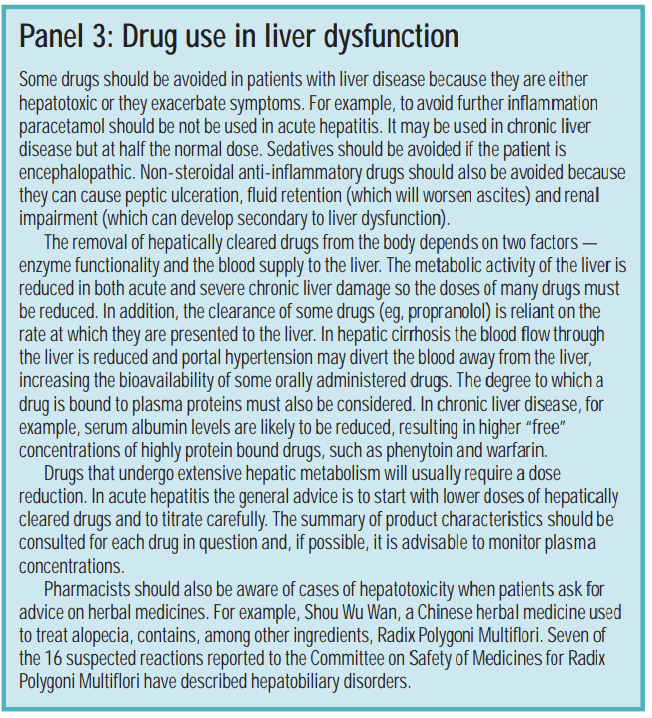
Numerous factors may result in liver dysfunction, which ranges from acute hepatitis to cirrhosis of the liver. Pharmacists are suitably placed to advise on drug use in such patients (see Panel 2). They should ensure that an accurate medication history is obtained when patients present with acute liver disease.
References
- Sougioultzis S, Dalakas E, Hayes PC, Plevris JN. Alcoholic hepatitis: from pathogenesis to treatment. Current Medical Research and Opinion 2005;21:1337–46.
- Forrest EH, Evans CDJ, Stewart S, Phillips M, Oo YH, McAvoy NC, et al. Analysis of factors predictive of mortality in alcoholic hepatitis and derivation and validation of the Glasgow alcoholic hepatitis score. Gut 2005;54:1174–9.
- Imperiale TF, McCullough AJ. Do corticosteroids reduce mortality from alcoholic hepatitis? A meta-analysis of the randomised trials. Annals of Internal Medicine 1990;113:299–307.
- Mathurin P, Mendenhall CL, Carithers RL, Ramond MJ, Maddrey WC, Garstide P, et al. Corticosteroids improve shortterm survival in patients with severe alcoholic hepatitis (AH): individual data analysis of the last three randomised placebo controlled double blind trials of corticosteroids in severe AH. Journal of Hepatology 2002;36:480–7.
- Ramond MJ, Poynard T, Rueff B, Mathurin P, Theodore C, Chpaut JC, et al. A randomised trial of prednisolone in patients with severe alcoholic hepatitis. New England Journal of Medicine 1992;326:507–12.
- Carithers RL, Herlong HF, Diehl AM, Shaw EW, Combes B, Fallon HJ, et al. Methylprednisolone therapy in patients with severe alcoholic hepatitis. A randomised multicenter trial. Annals of Internal Med 1989; 110: 685–90.
- Akriviadis E, Botla R, Briggs W, Han S, Reynold T, Shakil O. Pentoxifylline improves short-term survival in severe acute alcoholic hepatitis: a double-blind, placebo-controlled trial. Gastroenterology 2000;199:1637–48.
- Ramesh S, Sanyal AJ. Evaluation and management of nonalcoholic steatohepatitis. Journal of Hepatology 2005;42:S2–S12.
You might also be interested in…

Genomics surveillance programme for hepatitis C launched by UK Health Security Agency

How we treated more than 100 hepatitis C patients at pharmacist-led clinics in North Wales
