
SHUTTERSTOCK / THE PHARMACEUTICAL JOURNAL
After reading this article, you will be able to:
- Integrate prescribing-related activities into the overall training plan to maximise the use of the 90 hours of prescribing practice;
- Identify learning experiences during foundation training that can be translated into prescribing activities, such as medication reconciliation, clinical reviews and patient consultations;
- Recognise the significance of choosing an appropriate nominated prescribing area that enables the trainee to demonstrate their prescribing competencies;
- Utilise the prescribing development plan to set expectations, plan activities, and track progress throughout the foundation training year;
- Consider the role of designated prescribing practitioner and the wider multidisciplinary team in supporting and supervising the trainee’s prescribing development.
Trainee pharmacists entering the 2025/2026 foundation training year are assessed against the full spectrum of learning outcomes, including independent prescribing — marking a significant milestone in the progression of pharmacy education. This change applies to most trainees, excluding those graduating under the old learning outcomes or through the Overseas Pharmacists’ Assessment Programme1.
A critical element of this new framework is the requirement for 90 hours of dedicated prescribing practice, designed to help trainees develop and demonstrate the competencies required for safe and effective prescribing. These hours provide an opportunity to build core skills, such as communication, clinical reasoning, decision-making, and diagnostic reasoning — all essential for practising as an independent prescriber2,3.
This article offers practical guidance for designated supervisors (DS) and designated prescribing practitioners (DPPs) on how to maximise the value of this critical learning period. By leveraging structured planning and targeted activities, this roadmap aims to ensure the 90 hours are utilised to their fullest potential.
This article focuses on the approach to completing the 90-hour period of supervised prescribing-related learning as it applies to foundation trainee pharmacists undertaking their training in England, where programmes are managed by NHS England Workforce, Training and Education (NHSE WTE). Different arrangements and requirements exist in the other UK nations, where foundation training is overseen by their respective education bodies:
- Scotland: NHS Education for Scotland | NES
- Wales: Health Education and Improvement Wales
- Northern Ireland: Northern Ireland Centre for Pharmacy Learning and Development (NICPLD)
Trainees in these nations should refer to their national guidance for details specific to foundation training and assessment.
This article is part of a short series focused on the role of designated prescribing practitioner. It is recommended that you read this article in conjunction with:
- ‘How to be an effective designated prescribing practitioner‘
- ‘Entrustable professional activities: a new approach to supervising trainee pharmacists on clinical placements‘
- ‘How to be an effective mentor‘
Nominating a prescribing area
The selection of a nominated prescribing area is an important element of the foundation training year. By identifying a clearly defined clinical area, the trainee pharmacist can narrow their focus and more effectively develop and demonstrate their generic prescribing skills. Having a nominated prescribing area also prevents the trainee from feeling overwhelmed and directly facilitates some of the prescribing assessment activities, specifically those requiring the trainee to demonstrate clinical decision-making during a prescribing consultation (see Box 1)2.
Box 1: Prescribing assessment activities
- History taking;
- Physical and clinical examination skills;
- Prescribing consultation*;
- Prescription writing*;
- Log of 90 hours.
*Activity must be completed within the nominated prescribing area
A nominated prescribing area is distinctly different from and separate to the concept of scope of practice4. A nominated prescribing area is simply a defined clinical area that gives the trainee pharmacist a context from which they can demonstrate their prescribing skills. While the clinical and prescribing experience they gain from this period of training will indirectly contribute to the development of their scope of practice, this should be seen as an added advantage rather than the primary purpose of the nominated prescribing area.
There is no list of recommended nominated prescribing areas for trainee pharmacists[2]. NHS England provide some examples on what newly qualified prescribing might look like, which can inform nominated prescribing area selection5.
However, it needs to be agreed by the DSs and DPP and recorded on the e-portfolio when the trainee pharmacist starts2. The decision of the nominated prescribing area will be influenced by the expertise of available DPPs at the training place and the specific context of the setting. Nevertheless, DSs and DPPs should consider how much prescribing exposure the selected nominated prescribing area will provide to the trainee pharmacist and ensure that it is adequate. The discussion may include consideration of the following:
- The nominated prescribing area should be relevant to the sector in which the trainee pharmacist is carrying out their foundation year. For example, trainee pharmacists are less likely to be involved in prescribing decisions relating to management of minor ailments in secondary care than they would do in community pharmacy settings. Also, trainee pharmacists are less likely to be involved in management of surgical patients in community pharmacy or primary care than they would in secondary care setting;
- A DPP should also have the necessary skills and knowledge to be able to support, supervise and assess the trainee within the chosen nominated prescribing area including good knowledge of the relevant therapeutic approaches and required prescribing skills;
- The trainee pharmacist should have plenty of access to patients in order to be able to complete the consultation and prescribing activities, both of which need to be conducted within the nominated prescribing area (see Box 1)2.
Support from the wider multidisciplinary team (MDT) may be necessary and has the added benefit of providing a well-rounded and potentially collaborative learning experience.
Case example 1: Benefiting from multidisciplinary support
A nominated prescribing area of heart failure management has been selected for a trainee pharmacist completing their foundation training in a general practice. There is only a single clinician running a heart failure clinic every two weeks at the general practice.
In this situation, the trainee pharmacist is likely to have limited opportunities to gain a diverse range of patient exposure and learning experiences to support the development of prescribing skills. It may also take longer for them to complete prescribing activities and demonstrate the prescribing competencies.
However, if multiple members of the MDT are involved in the management of patients with heart failure — such as pharmacists, advanced care practitioners, specialist nurses and doctors/general practitioners — the trainee will more likely have regular opportunities to collaborate with and learn from suitably qualified clinicians who specialise in the trainee’s nominated prescribing area. Approaching the practice hours in this way would provide a well-rounded learning experience and make the prescribing assessments easier to achieve.
The nominated prescribing area should be of appropriate clinical complexity. Trainee pharmacists are not expected to manage complex patients and therefore the chosen nominated prescribing area should reflect their status as a foundation trainee working within a narrow scope of practice. For example, choosing hypertension as a nominated prescribing area with a DPP running hypertension clinics may be more appropriate than choosing a nominated prescribing area with a DPP running immunotherapy toxicity clinics for oncology patients.
Where possible, a nominated prescribing area should provide prescribing supervision and assessment opportunities in multiple sectors. For example, long-term condition management is likely to provide a wide range of development opportunities for prescribing.
Case example 2: Nominated prescribing area spanning multiple sectors
A nominated prescribing area of respiratory tract infections has been selected for a trainee pharmacist completing a community pharmacy and secondary care multisector foundation training programme. In community pharmacy, the prescribing development plan (PxDP) includes exposure to upper respiratory tract infection presentations. The trainee pharmacist will be involved in minor ailment consultations and management of coughs and colds. They will also have opportunities to be involved in assessment and management of sore throat presentations as part of the Pharmacy First service6.
In secondary care, the PxDP includes exposure to lower respiratory tract infection presentations. The trainee pharmacist will be clinically reviewing patients admitted with lower respiratory tract infections (e.g. community-acquired pneumonia) and will be involved in antimicrobial stewardship. They will have opportunities to work with prescribers, including antimicrobial pharmacists and doctors, during assessment, diagnosis and prescribing decision-making. In both sectors, the trainee pharmacist will have access to patients with respiratory tract infections.
Value of learning contracts and proactive planning
In addition to regular supervision meetings with their DS, trainees are also advised to have regular prescribing development meetings. It is an established expectation that foundation trainees will complete a learning needs analysis (LNA) and learning agreement with their DS at the start of their training year, and this process can naturally be extended to also include a prescribing LNA and the development of a PxDP2. The PxDP can be used to set expectations and agree activities for both trainee pharmacists and DPPs. This also could serve as a guide for the prescribing activities required to meet the prescribing competencies. Lack of a clear plan at the start of the programme was highlighted as the biggest challenge by both trainee pharmacists and DPPs in the NHS England Independent prescribing pilot programme delivered by Universities of Bradford and Huddersfield7.
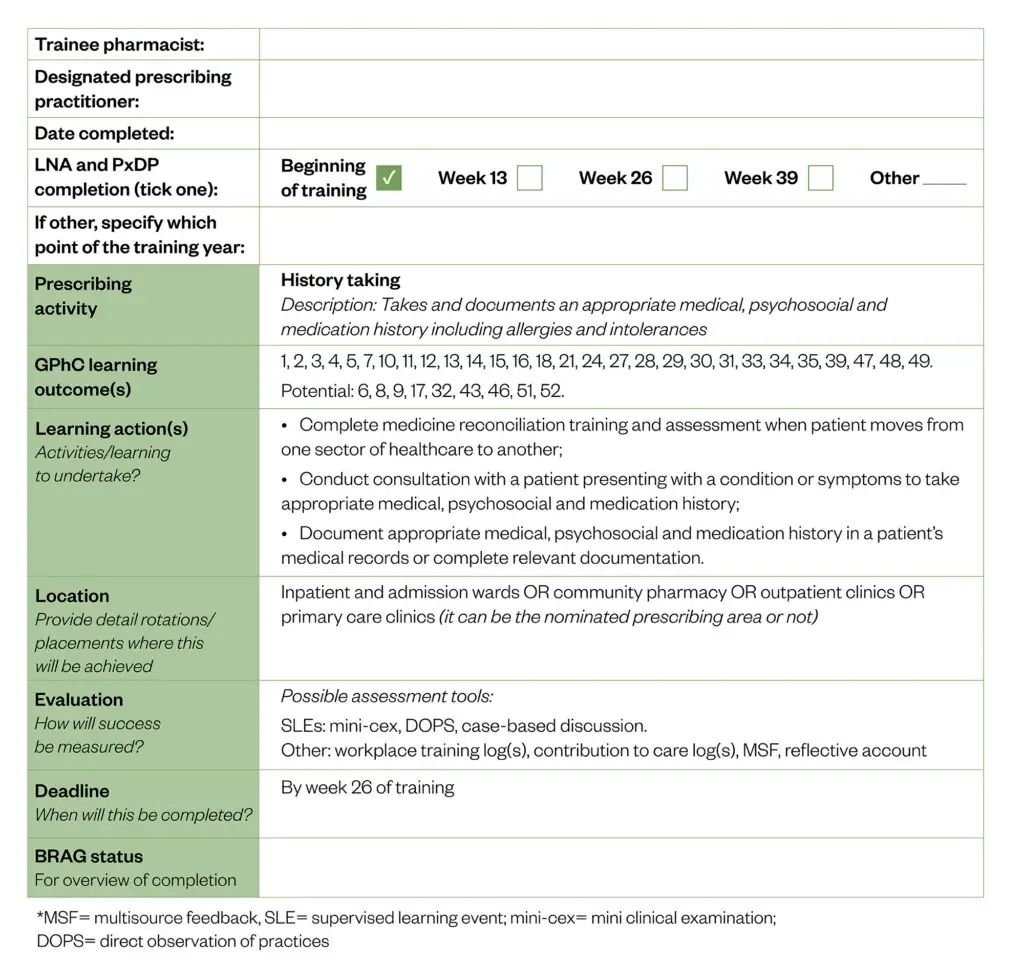
The PxDP should be linked to the prescribing assessment activities and may include2:
- Learning actions: specific activities or learning objectives to be undertaken;
- Detailed rotation/placements: specifying where, when and how the learning actions will be achieved;
- Evaluation: criteria for measuring success;
- Deadline: timelines for completing each activity;
- BRAG status: a colour-coded system (Blue, Red, Amber, Green) for tracking the completion of learning activities.
The PxDP should be reviewed and updated regularly. At a minimum, this should be done at the progress review meetings that trainees will undertake at week 13, 26, 39 and again towards the end of the foundation training year. Regular reviews allow for early identification of areas that require more development; thus, actions can be put in place in a planned and timely manner8.
An example of PxDP is provided in the Figure below, which can be adapted to meet the needs of the training programme or tailored to a specific nominated prescribing area8,9.
Allocation of the 90 hours
The structure of the 90 hours is flexible and does not need to be completed in a single block. Hours can be adapted to fit the specifics of the training programme and agreed between both the DPP and trainee. NHS England has suggested some possible ways to structure prescribing time, including2:
- 0.5 days each day over a five- to six-week period;
- One day per week over a 13-week rotation (aligning to a 13-week cross sector rotation or longitudinal placement)10;
- A dedicated four- to six-week prescribing placement in an appropriate setting.
DSs and DPPs should integrate prescribing-related activities into the training plan for the whole foundation training duration. The prescribing hours will include hours spent completing prescribing assessment activities (history taking, physical and clinical examination skills, prescribing consultation, prescription writing) or other planned learning activities.
Prescribing development hours should be planned in the PxDP (see Figure for an example). The use of PxDP and longitudinal planning would allow the required skills to build over the course of the foundation training, including the level of complexity and autonomy.
It is likely to be possible to translate existing activities completed by trainee pharmacists during their foundation year into prescribing activities eligible for the log of 90 hours7. Identifying this type of flexible learning activity can be time efficient and prevent the trainee from feeling overwhelmed by the need to complete separate activities for both the foundation assessment as well as the prescribing component. Table 1 provides some examples of how this can be done.
Case example 3: Medicines reconciliation
A pregnant woman with type 1 diabetes mellitus and hyperemesis gravidarum was admitted to hospital. During medicines reconciliation, it was noted that her aspirin 150mg daily prescription — recommended by National Institute for Health and Care Excellence (NICE) guidelines to prevent pre-eclampsia from week 12 to delivery — was omitted from her inpatient chart.
To rectify this, the trainee pharmacist:
- Reviewed the NICE guidelines to confirm aspirin’s suitability despite its unlicensed indication;
- Checked for contraindications or drug interactions;
- Discussed potential actions with practice supervisor;
- Consulted with a prescriber to reinstate the medication.
Outcome: The medication was prescribed during inpatient stay.
Foundation assessment activity: Medication reconciliation and medicines optimisation.
Prescribing activity: History taking, prescription writing, if within the nominated prescribing area.
Assessment tools: Mini-Cex, CBD or contribution to care log; MSF.
Case example 4: Medication adherence and review
An older patient with flare up of myasthenia gravis was admitted to the hospital. During medicines reconciliation, the trainee pharmacist identified that the patient had unintentional non-adherence of prescribed medicines owing to swallowing difficulties.
The trainee pharmacist reviewed prescribed medicines using available resources, such as NEWT guidelines, to identify more suitable formulations for patients with swallowing difficulties. They produced a list of recommendations, which was discussed with a practice supervisor and shared with the prescribing team. Where appropriate, liquid and soluble preparations of medicines were prescribed. When no appropriate alternative was available, instructions of crushing the tablets or opening capsules were documented. Advice was also communicated to the patient and their caregivers.
Outcome: Patient’s adherence to medicines improved during admission.
Foundation assessment activity: Medicine reconciliation and medicine optimisation.
Prescribing activity: History taking, prescribing consultation and prescription writing, if within the nominated prescribing area.
Assessment tools: Mini-Cex, CBD or contribution to care log; MSF; patient feedback.
There may be other learning experiences that trainee pharmacists are already involved in that can also be used to make up the 90 hours of learning experiences attributable to development as a prescriber in practice. These may be direct and indirect patient care.
Examples include:
- Completion of prescribing related audits, service evaluation and research projects;
- Counselling on new medication or discharge medicines, including minor ailments, discharge-medicine service and new medicine service consultations;
- Opportunities to be involved in prescribing governance related activities, such as reporting of adverse effects to the MHRA, root-cause analysis following prescribing significant events, or subsequent dissemination of learning to prescribers.
Prescribing supervision and assessment
The DPP does not need to directly supervise all the trainee pharmacist’s prescribing development time but must spend sufficient time directly assessing the trainee2. Some of the hours can involve activities under the supervision of other prescribers, which will broaden the trainee’s exposure to different prescribing practices and clinical decision-making scenarios and helps distribute the supervision load. Also, history taking and physical and clinical examination skills can be completed outside the nominated prescribing environment2. This flexibility can be utilised for multisector foundation training programme and incorporated in the PxPD (see Table 2 and Case example 2).
Additional activities linking to prescribing development time
Trainee pharmacists will have other assessment activities in addition to prescribing assessment activities to complete during their foundation training8. These additional activities can also be planned to contribute to prescribing development time2. These activities can include medication safety, public health intervention, responding to medication enquiries, service improvement, teaching and mentoring.
Table 3 provides examples of some of these activities (not an exhaustive list) and illustrates how it maps to the Royal Pharmaceutical Society prescribing competencies3.
Managing multiple priorities
Many trainee pharmacists describe their foundation training year as an exercise in ‘spinning plates’ where they need to strike a balance between completing the foundation training assessment, continuously learning and preparing for the General Pharmaceutical Council (GPhC) registration exam. Now from 2026, prescribing activities and the actions agreed with their DS and DPP can be added to this list. It is important that trainee pharmacists are supported to develop their time management and organisation skills and their wellbeing should be considered during supervision meetings.
Regular protected learning time (PLT) during foundation training should be provided to trainee pharmacists to consolidate their learning, build their portfolio and engage in professional development although the GPhC does not specify how much PLT should be allocated to trainee pharmacists in a workplace11. A campaign launched in February 2025 by the Guild of Healthcare Pharmacists called for pharmacists working in the NHS to have a minimum of 10% of their contracted hours as PLT and this could be used as starting point for deciding on the PLT for trainee pharmacists as well12.
Pharmacist Support and NHS England have also produced resources and guidance on how DSs and DPPs can support trainees that may encounter difficulties during their foundation training.
Summary
The foundation training of trainee pharmacists is an intensive period for both trainee pharmacists and training supervisors. By forward planning and tailoring existing activities incorporate prescribing assessment activities, the challenge of delivering 90 hours of high-quality practice learning for prescribing can be achieved. It is crucial to provide effective and sufficient supervision, including wellbeing support, to ensure trainees succeed and are ready for their first day of registered practice as a prescribing pharmacist.
- This article was amended on 11 July 2025 to clarify that it refers specifically to England
- 1.Standards for the initial education and training of pharmacists. General Pharmaceutical Council. 2021. Accessed July 2025. https://assets.pharmacyregulation.org/files/2024-01/Standards%20for%20the%20initial%20education%20and%20training%20of%20pharmacists%20January%202021%20final%20v1.4.pdf
- 2.Prescribing Supervision and Assessment in the Foundation Trainee Pharmacist Programme from 2025/26. NHS England. January 2024. Accessed July 2025. https://www.hee.nhs.uk/sites/default/files/documents/Prescribing%20Supervision%20and%20Assessment%20in%20the%20Foundation%20Trainee%20Pharmacist%20Programme%20JAN%202025%20V1.3.pdf
- 3.A Competency Framework for all Prescribers. Royal Pharmaceutical Society. September 2021. Accessed July 2025. https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Prescribing%20Competency%20Framework/RPS%20English%20Competency%20Framework%203.pdf?ver=mctnrKo4YaJDh2nA8N5G3A%3d%3d
- 4.Professional Guidance: Expanding Prescribing Scope of Practice. Royal Pharmaceutical Society. June 2022. Accessed July 2025. https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Prescribing%20Competency%20Framework/RPS%20-%20Scope%20of%20Practice-English-220601.pdf?ver=fNYC4O_ThDfE3AsC01HvFw%3d%3d
- 5.Emerging routes to early career prescribing in pharmacy. NHS England. 2024. Accessed July 2025. https://www.hee.nhs.uk/our-work/pharmacy/transforming-pharmacy-education-training/emerging-routes-early-career-prescribing-pharmacy
- 6.Pharmacy First . NHS England. 2024. Accessed July 2025. https://www.england.nhs.uk/primary-care/pharmacy/pharmacy-services/pharmacy-first/
- 7.Achi PI, Kavanagh S, Medlinskiene K, et al. Evaluation report: Independent Prescribing Pilot Programme during Foundation Training for Trainee Pharmacists. NHS England. December 2024. Accessed July 2025. https://www.hee.nhs.uk/sites/default/files/documents/NHSE%20WTE%20Independent%20Prescribing%20Pilot%20Evaluation%20Report.%20December%202024.pdf
- 8.Foundation Trainee Pharmacist Assessment Activities and Tools Guide. NHS England. July 2023. Accessed July 2025. https://www.hee.nhs.uk/sites/default/files/documents/Foundation%20Trainee%20Pharmacist%20Assessment%20Activities%20and%20Tools%20Guide.pdf
- 9.Visual mapping of the assessment activities. NHS England. 2023. Accessed July 2025. https://www.hee.nhs.uk/sites/default/files/documents/IETP%20Assessment%20Learning%20Outcome%20Mapping%20v2%20FINAL.xlsx
- 10.Kinsey H, Sokhi J, Christou M, Wright D. Longitudinal placements for trainee pharmacists: Learning whilst improving patient care. Medical Education. 2021;56(2):220-228. doi:10.1111/medu.14684
- 11.Foundation training manual 2024/25. General Pharmaceutical Council. 2024. Accessed July 2025. https://assets.pharmacyregulation.org/files/2024-06/GPhC-%20foundation-training-manual-2024-25.pdf
- 12.Campaign to give NHS pharmacists mandated protected learning time launched by the Guild of Healthcare Pharmacists. Pharmaceutical Journal. Published online 2025. doi:10.1211/pj.2025.1.346237
5 comments
You must be logged in to post a comment.



Please can you highlight that this approach to completing 90 hours period of learning relates to those undertaking their foundation training year in England only and that Scotland, Wales and Northern Ireland have programmes and approaches to meeting 90 hours period of learning in practice tailored to their requirements. Thank you.
Many thanks for your comment. I am senior editor, research and learning at the PJ. I agree this is an important clarification and will work with the article authors on a suitable amendment.
Thank you Alex, that is much appreciated.
Ailsa Macdonald, Principal lead prescribing and clinical skills,
NHS Education for Scotland
I’d like to echo Ailsa’s request for a clear acknowledgment that this useful article relates to the Foundation Training Year managed by NHSE and that the programmes managed by NES, HEIW and NICPLD have some separate arrangements.
Many thanks, Lisa Smith Postgraduate Pharmacy Dean, NICPLD
Many thanks for your comment. I am senior editor, research and learning at the PJ. I agree this is an important clarification and will work with the article authors on a suitable amendment.