DR P. MARAZZI/SCIENCE PHOTO LIBRARY
After reading this article, you should be able to:
- Know which biologics are available for the treatment of juvenile idiopathic arthritis and when each is indicated;
- Understand the pre-screening assessment criteria that are required prior to initiating a biologic and any ongoing monitoring requirements;
- Identify any adverse reactions related to biologics and counsel patients on how these reactions can be avoided.
Juvenile idiopathic arthritis (JIA) is the most common chronic childhood rheumatic disease. It is an autoimmune inflammatory disease affecting the joints[1]. Additional information on classification of the different types of JIA, recognition, diagnosis and conventional pharmacological management of the condition can be found in ‘Juvenile idiopathic arthritis: recognition, diagnosis and conventional pharmacological management’.
This article will cover considerations for the management of JIA with biologic disease modifying anti-rheumatic drugs (bDMARDs). bDMARDs have greatly changed the treatment and outcomes of JIA. These molecules include monoclonal antibodies, soluble cytokine receptors and recombinant receptor antagonists targeting immune response regulators, such as pro-inflammatory cytokines, cell surface receptors and signalling molecules involved in the regulation of B-cell and T-cell lymphocyte responses[2,3].
The general pathway for accessibility of biological agents in the management of JIA in England is governed by the ‘Clinical commissioning policy statement: Biologic therapies for the treatment of juvenile idiopathic arthritis’[4]. Alongside this statement, access to biologics in England and Wales is restricted by the need to obtain BlueTeq approval prior to treatment initiation[5]. Relevant clinicians of the paediatric rheumatology multidisciplinary team will have different levels of access to the platform. The BlueTeq form will highlight the exact clinical criteria needed for access to these high-cost medications[5]. In some instances, even when there is no specific paediatric National Institute for Health and Care Excellence (NICE) technical appraisal or NHS England commissioning policy available, the ‘Medicines for children’ policy may be used to access high-cost treatments in post-pubertal children when the paediatric disease has an adult equivalent[6]. With respect to this, it is important to note that JIA is not considered equivalent to adult rheumatoid arthritis, so the usefulness of the ‘Medicines for Children’ policy is somewhat restricted in JIA. The only exception to this rule is systemic JIA (Still’s disease) and psoriatic JIA (psoriatic arthritis), where both paediatric conditions are considered equivalent to their adult counterparts. The policy statement includes a treatment pathway, detailing criteria needed for access, such as disease sub-type, level of activity and previous therapy[4]. The pathway is undergoing review, as new biological treatments and different formulations have become available since its publication.
Table 1 summarises the additional available commissioned treatments in England not currently listed in the pathway[7–9]. With regards to the other devolved nations, Wales are in the process of developing their own BlueTeq platform; while this is ongoing, if a Welsh patient is receiving high-cost treatment from a specialised treatment centre in a different devolved nation, Welsh BlueTeq officers should be contacted to clarify funding status. Scotland and Northern Ireland have their own approval mechanisms[10].
Monitoring of biologic disease modifying anti-rheumatic drugs
Patients commenced on biological DMARDs must undergo strict safety monitoring (see Box 1)[11–15], although specific guidance on how often to perform the monitoring, or when to act on a deranged blood result, is lacking.
An agreement between the clinician and the patient/parent/carer needs to take place during discussions about medicines to ensure blood monitoring is adhered to. For units with significant numbers of patients receiving these treatments, the role of a ‘blood clerk’, whose responsibilities include maintaining an up-to-date database of current blood monitoring status, can be invaluable[16]. Studies looking into early use of biologics focusing on the ‘window of opportunity’ model are currently under development for some of these molecules[17].
Box 1: Monitoring of biological disease modifying anti-rheumatic drugs[11–15,18–21]
Screening pre-commencement
- All patients who are biologic naïve should be screened for active or latent tuberculosis;
- Varicella and measles immune status should be checked in patients due to start immunosuppressants (if the result is not available this is not a reason for delaying the start of therapy);
- Hepatitis B/C testing should be carried out and vaccination status checked, depending on risk in particular areas/particular patient;
- Live vaccinations are contraindicated and should be avoided until a patient has been off immunosuppressant therapy for three to six months (depending on treatment). If vaccinating before starting therapy, there is usually a four-week wait between the live vaccine and starting a biologic immunosuppressant;
- Pregnancy test if appropriate. For advice on the management of biologics in pregnancy, follow British Society for Rheumatology advice[2,40].
General principles of monitoring for biologic DMARDs
- Frequency standard: different specialist units may follow different monitoring regimes;
- Regularly check full blood count (e.g. neutrophils, platelets), and conduct liver function tests and urea and electrolytes (U&Es [renal markers]);
- Most specialist units will monitor to the highest practical standard. This general approach (see Table 2) has been extrapolated from methotrexate monitoring and applies to all drugs, with the exception of tocilizumab and tofacitinib (which have their own recommendations guided by the summary of product characteristics [SPC]).
Examples of the blood safety monitoring schedule can be seen in Table 2. Note that some deranged results may be associated with the patient’s disease rather than being drug related.
TNF-alpha inhibitors
The biologics for which there is the most efficacy and safety data in JIA are TNF-alpha inhibitors. Etanercept, adalimumab and infliximab are all licensed and approved for use in the treatment of methotrexate refractory extended oligoarticular-JIA and polyarticular-JIA in the UK[4,22]. General safety concerns with TNF-alpha inhibitors include increased risk of infection and subcutaneous injection site reactions[23,24]. Suggested strategies for the management of injection site reactions (including during the switch to biosimilar therapies) are summarised in Box 2[25]. Other potential adverse effects include an increased risk of developing demyelinating disease, leukocytoclastic vasculitis and drug-induced lupus[15]. The potential increased risk of malignancy has been hotly debated over the years. A study showed there was no relationship between medication use in JIA and development of cancer, and it has been widely recognised that children with JIA, irrespective of treatment, carry an increased likelihood of malignancy development[26].
Infliximab is used off label for JIA[27]. Etanercept and adalimumab are both licensed treatments for children aged two years and above with JIA. For this reason, they are usually chosen as a first-line biological agent in methotrexate refractory patients over infliximab (unless there is a significant subcutaneous needle aversion in the patient or concerns about adherence)[4]. Patients and their carers are usually given a choice between both agents. Since the advent of biosimilar medicines, adalimumab is often the most cost-effective option, especially in younger patients (since biosimilar paediatric formulations of etanercept do not exist)[28]. Adalimumab is also the TNF-alpha inhibitor of choice in patients with JIA-associated uveitis[29]. Concomitant use of methotrexate is often indicated for patients on infliximab and adalimumab to prevent antibody formation against the drug[30–32]. The evidence of the role of methotrexate in preventing antibody formation in patients on etanercept is less clear, and trials comparing etanercept monotherapy versus combination of methotrexate and etanercept have failed to show statistically significant differences[33]. In UK practice, adding methotrexate to a TNF-alpha inhibitor in patients who have clinical improvement but no improvement of inflammatory markers, or in patients who, based on symptoms and biochemical markers, show signs of flare is still common and may have a role in preserving biological therapies later on in the child or young person’s life[17,34].
Box 2: Suggested strategies for management of injection site reactions with subcutaneous injections of bDMARDS[24]
Non-pharmacological treatment suggestions
- Medication temperature — take medicine out of the fridge 30 minutes before use and place on flat surface to allow it to come up to room temperature. This helps reduce pain. Do not warm the medicine in any other way;
- Cold compress — try a cold pack applied to the site before and after injection. This may help to numb the area. Do not use a warm compress or heating pad as this will increase blood flow and may cause more pain;
- Rotation of injection sites — make sure the injection is given in fatty areas by pinching the skin. Change the area the injection is given in each time. Preferred sites are the thighs and lower abdomen;
- Avoid sensitive locations — avoid injection in areas with a bruise, scar, visible vein or areas with redness, swelling, hard or broken skin.
Pharmacological treatment suggestions
- Antihistamines — cetirizine and/or chlorphenamine (follow over-the-counter dosing recommendations);
- Steroid cream — hydrocortisone cream 1%. This should be considered if the reaction has not responded to the antihistamines recommended above. Apply a pea-sized amount to affected area twice daily while symptoms are still present, for no more than seven days;
- Analgesia — mild discomfort/pain at the injection site can be treated with paracetamol or ibuprofen (follow over-the-counter dosing recommendations).
Interleukin inhibitors
Interleukin (IL) inhibitors have become available more recently for the management of different subtypes of JIA. The IL-1 inhibitor anakinra and the IL-1-beta inhibitor canakinumab are both licensed for the treatment of systemic JIA[4]. Tocilizumab, an IL-6 inhibitor, is licensed both for the management of systemic-JIA, extended oligoarticular-JIA and polyarticular-JIA. However, only anakinra and tocilizumab are commissioned for the management of s-JIA[4,35].
In 2022, NHS England published a new canakinumab commissioning policy detailing that, although there is “sufficient evidence to commission this treatment for systemic onset JIA”, when balanced against other drug commissioning priorities, NHS England was not in a position to fund it[36]. This prevents patients in England from accessing a medication that is licensed for their condition. Anakinra has proven efficacy in treating s-JIA alone, as well as in combination with methotrexate in clinical trials, and it is the treatment of choice in the presence of macrophage activation syndrome[4,37]. However, its major drawback is the need for daily subcutaneous injections.
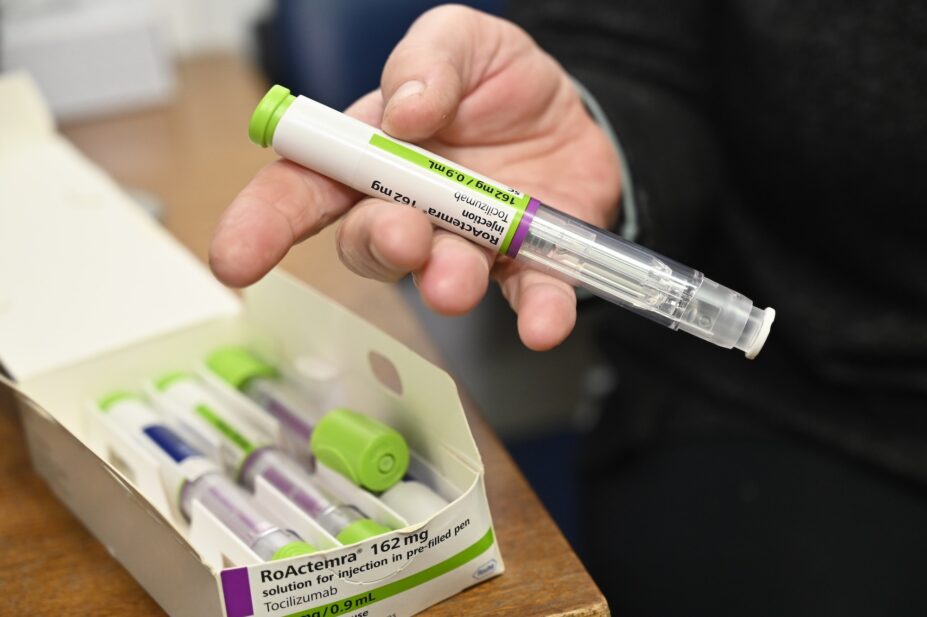
Tocilizumab offers the advantage of weekly, fortnightly or every three-week subcutaneous injections (depending on age and weight and subtype of JIA). Tocilizumab has shown a higher propensity in causing neutropenia and increased rates of infections compared with TNF-alpha inhibitors, especially when used in combination with methotrexate[21]. As a result, blood safety monitoring for patients on tocilizumab tends to be stricter compared to adalimumab or etanercept monotherapy. The SPC for tocilizumab details the suggested frequency of monitoring and how and when to adjust therapy in the presence of blood dyscrasias or elevated liver function tests[21]. Tocilizumab is also a second- or third-line biological treatment option in patients with extended oligoarticular- and polyarticular-JIA[4]. Initially, only the intravenous (IV) route was available for paediatric patients. However, in 2017, pharmacokinetic and clinical data were released on using subcutaneous preparations in children from two years of age with positive findings[38]. Subcutaneous tocilizumab has proven to be as effective as IV tocilizumab and it allows for home administration; VAT savings, using homecare solutions; and reduced hospital visits[39]. On the other hand, incidental reports suggest that the subcutaneous formulation stings and the pen formulation is only licensed for children aged 12 years and above[21]. Off-label use of the pen formulation could be considered in cases of needle aversion against the pre-filled syringe form.
Abatacept
Available as a second- or third-line biologic in the management of extended oligoarticular- and polyarticular-JIA[4]. Abatacept works by T-lymphocyte activation modulation[40]. Like tocilizumab, it was only available as an IV formulation until recently, but unlike tocilizumab, subcutaneous administration of abatacept is weekly for all patients[40]. There are three subcutaneous strengths: 50mg, 87.5mg (available only as pre-filled syringes) and 125mg (available as pre-filled syringes and pens). The 125mg pen is only licensed in children aged 12 years and over who weigh 50kg or more. As with tocilizumab, off-label use of the pen in children who meet the weight criteria with needle aversions can be considered. However, owing to production restrictions in the UK, the 50mg and 87.5mg injections are only available as an import; this hinders their use via homecare providers and renders this treatment choice much less cost-effective compared with tocilizumab[41].
Rituximab
Rituximab is a monoclonal antibody that binds to CD20 on lymphocyte B cells, achieving a depletion of B cells from plasma[42]. Treatment with rituximab is off label and, in England, it is exclusively recommended for rheumatoid factor positive JIA refractory over TNF-alpha inhibitor treatment[4]. The initial evidence for use was extrapolated from adult RA studies, and rheumatoid factor positive poly[articular] JIA is the only paediatric subtype of JIA considered to be analogous to RA[43]. Further studies in JIA have confirmed the role of rituximab in the treatment of severe refractory disease[44]. Rituximab is now available as a biosimilar, meaning the drug cost for this therapy has considerably lowered. Teams may decide to use it off label, outside of commissioning recommendations, when all other treatments have failed[17,34].
Secukinumab
A fully human monoclonal antibody that targets IL-17A, the licence for secukinumab was extended in the UK in November 2022 to cover two new paediatric rheumatology indications: psoriatic JIA and enthesitis-related JIA refractory to TNF-alpha inhibitor treatment[45,46]. The drug is only commissioned in England via the ‘Medicines for children’ policy[6]. Since enthesitis-related JIA does not have an adult equivalent disease, the drug is only commissioned in England for children with psoriatic JIA, leaving paediatric rheumatology patients with enthesitis-related JIA unable to access this treatment.
After five initial weekly doses, the frequency of administration goes down to every four weeks[9]. Compared with the administration frequency of other drugs licensed for this indication, this could prove to be an advantage when it comes to patient choice if all treatments are available for them. As with tocilizumab and abatacept, the pen formulation is only available in the higher strength (150mg) for children weighing 50kg and over. Off-label use of the pen in children with needle aversion who meet the weight criteria could be considered[45].
Tofacitinib
Targeted synthetic DMARDs are oral, small-molecule drugs: The first Janus-associated tyrosine kinase (JAK) inhibitor tofacitinib was approved for use in the UK in patients with extended oligoarticular- and polyarticular-JIA from 2 years of age in 2022[20]. It works by blocking JAK-STAT (signal transducer and activator of transcription) pathways, interrupting the transduction of extracellular pro-inflammatory signals into the nucleus. The efficacy of first-generation JAK inhibitors (namely tofacitinib and baricitinib) was first explored in adults with RA and then in other immune-mediated inflammatory diseases[17,34]. Following a successful phase 1 trial, the subsequent phase 3 randomised trial demonstrated the safety and effectiveness of tofacitinib in JIA, resulting in reduced flares and disease activity[47,48].
Tofacitinib is not considered a biologic medicine and has different monitoring requirements compared with biologics. There are strict criteria for starting the drug and safety monitoring, including lymphocyte and haemoglobin checks[20]. The risk of deep vein thrombosis has been recorded in adult studies; however, deeper analysis has shown no paediatric patients suffered this potential adverse effect, and of the adult patients, only older patients with several comorbidities developed coagulation issues[20]. The most obvious advantage of this treatment is that it is the first targeted synthetic DMARD that can be offered to paediatric patients via the oral route[7]. The drug is available as a liquid and tablet (dosage dependent on weight), offering a lifeline to children unable to tolerate subcutaneous treatments owing to needle aversion or other factors. It is important to consider that the patient will still need to undergo safety blood monitoring; therefore, complete avoidance of needles is not possible[20].
Biosimilars
The effects of biological DMARDs in inducing and maintaining remission have been significant and often superior to the conventional DMARD counterparts. Owing to the balance of long-term safety and the high cost associated with these treatments, health economy plays a role in deciding the place of biologics in the treatment of JIA[13]. Consequently, many developing nations may struggle to access these costly medicines. The introduction of rheumatology biosimilars in 2013 (by definition, molecules ‘very similar’ to already approved biological drugs) was hailed as a potential solution to increase access to these medicines[49]. There were initial concerns with regards to comparable clinical efficacy in paediatric patients and risk of immunogenicity caused by switching agents, but additional research has laid these fears to rest[50,51]. However, there can be important practical differences between biosimilar medicines and originator molecules; for example, differences in formulation, administration device and the excipients contained in them[13]. Citrate-free formulations of adalimumab are used first-line in paediatric patients as they are considered to cause less pain/stinging on administration. Manufacturers have not developed a biosimilar version of paediatric etanercept preparations, so patients on lower doses of etanercept have to remain on the originator product[13]. See Box 3 for general tips on prescribing biologic and biosimilar medicines[52].
Box 3: Tips for prescribing biologics, biosimilars and JAK inhibitors[52,53]
- Prescribing and documenting of biologics and biosimilars should follow commissioning guidelines, and be by brand and active drug name, in particular when there is a biosimilar in use;
- All patients must be counselled by a rheumatology nurse specialist or pharmacist prior to commencing treatment;
- Dose (preferably in mg/weight or mg/surface area), frequency of administration, formulation, brand and route of administration should be documented clearly in all relevant patient communication;
- Biologic, biosimilar and synthetic DMARD drugs for English and Welsh patients must be registered on the BlueTeq platform for approval at the time of initiation of therapy. Drugs that do not have BlueTeq approval cannot be prescribed without prior discussion with the trust’s medicines management committee. The paediatric clinical affairs branch of the British Society for Rheumatology has devised a helpful resource to navigate current commissioning rules in England and Wales. This resource can be made available by request to any of the authors of this text;
- Consider enrolment of the patient in one of the available biologics registers. The UK JIA biologics register was set up to collect real-world, long-term safety and effectiveness data on biologics and biosimilar medicines used to treat JIA;
- Homecare provision is recommended for subcutaneous treatments and JAK inhibitors to increase cost effectiveness, once families are trained (they may be trained at home by community nurses) and happy with administration.
Test yourself
- 1Scott C, Brice N. Juvenile idiopathic arthritis – an update on its diagnosis and management. S Afr Med J. 2015;105:1077. https://doi.org/10.7196/samj.2015.v105i12.10223
- 2Hayward K, Wallace CA. Recent developments in anti-rheumatic drugs in pediatrics: treatment of juvenile idiopathic arthritis. Arthritis Res Ther. 2009;11:216. https://doi.org/10.1186/ar2619
- 3Harris JG, Kessler EA, Verbsky JW. Update on the Treatment of Juvenile Idiopathic Arthritis. Curr Allergy Asthma Rep. 2013;13:337–46. https://doi.org/10.1007/s11882-013-0351-2
- 4Clinical Commissioning Policy Statement: Biologic Therapies for the treatment of Juvenile Idiopathic Arthritis (JIA). NHS England. 2015. https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/10/e03pd-bio-therapies-jia-oct15.pdf (accessed April 2024)
- 5Commissioner High Cost Drugs System. BlueTeq. 2024. https://www.blueteq.com/commhcd.html (accessed April 2024)
- 6Commissioning medicines for children in specialised services. NHS England. 2024. https://www.england.nhs.uk/publication/commissioning-medicines-for-children-specialised-services/ (accessed April 2024)
- 7Tofacitinib for treating juvenile idiopathic arthritis. National Institute for Health and Care Excellence. 2021. https://www.nice.org.uk/guidance/ta735 (accessed April 2024)
- 8Clinical Commissioning Policy: Adalimumab (Humira) and Infliximab (Remicade) as Anti-TNF Alpha Treatment Options for Paediatric Patients with Severe Refractory Uveitis. NHS England. 2015. https://www.engage.england.nhs.uk/consultation/specialised-services-consultation/user_uploads/uveitis-paediatrics-policy.pdf (accessed April 2024)
- 9Certolizumab pegol and secukinumab for treating active psoriatic arthritis after inadequate response to DMARDs. National Institute for Health and Care Excellence. 2017. https://www.nice.org.uk/guidance/ta445/chapter/1-recommendations (accessed April 2024)
- 10Blueteq High Cost Drug System. All Wales Therapeutics and Toxicology Centre. 2023. https://awttc.nhs.wales/pages/blueteq-high-cost-drug-system/#:~:text=How%20will%20Blueteq%20HCD%20forms,used%20to%20develop%20the%20forms (accessed April 2024)
- 11Warrier KC. A practical guide to using biologics in juvenile idiopathic arthritis. Paediatrics and Child Health. 2022;32:229–35. https://doi.org/10.1016/j.paed.2022.03.005
- 12JIA medication. National Rheumatoid Arthritis Society. 2021. https://jia.org.uk/resource/medications/ (accessed April 2024)
- 13Paediatric and adolescent guidance. British Society for Rheumatology. 2022. https://www.rheumatology.org.uk/practice-quality/guidelines/paediatric-adolescent-guidance (accessed April 2024)
- 14Cuevas OA, Webb A. P51 A service evaluation into the reduction of blood monitoring frequency during the COVID-19 pandemic. Rheumatology Advances in Practice. 2022;6. https://doi.org/10.1093/rap/rkac067.051
- 15Beukelman T, Patkar NM, Saag KG, et al. 2011 American College of Rheumatology recommendations for the treatment of juvenile idiopathic arthritis: Initiation and safety monitoring of therapeutic agents for the treatment of arthritis and systemic features. Arthritis Care & Research. 2011;63:465–82. https://doi.org/10.1002/acr.20460
- 16Hunter E, Cuevas OA. P58 A re-audit on the adherence to blood monitoring guidelines in paediatric rheumatology patients on methotrexate, etanercept and adalimumab after the introduction of a blood clerk in the team. Rheumatology. 2019;58. https://doi.org/10.1093/rheumatology/kez416.025
- 17James RA, Wedderburn LR. Modern management of juvenile idiopathic arthritis. Prescriber. 2016;27:37–43. https://doi.org/10.1002/psb.1472
- 18Russell MD, Dey M, Flint J, et al. British Society for Rheumatology guideline on prescribing drugs in pregnancy and breastfeeding: immunomodulatory anti-rheumatic drugs and corticosteroids. Rheumatology. 2022;62:e48–88. https://doi.org/10.1093/rheumatology/keac551
- 19Flint J, Panchal S, Hurrell A, et al. BSR and BHPR guideline on prescribing drugs in pregnancy and breastfeeding—Part I: standard and biologic disease modifying anti-rheumatic drugs and corticosteroids: Table 1. Rheumatology. 2016;55:1693–7. https://doi.org/10.1093/rheumatology/kev404
- 20XELJANZ 5 mg film-coated tablets. Electronic Medicines Compendium. 2023. https://www.medicines.org.uk/emc/product/2500/smpc#gref (accessed April 2024)
- 21RoActemra 20mg/ml Concentrate for Solution for Infusion. Electronic Medicines Compendium. 2022. https://www.medicines.org.uk/emc/product/6673/smpc#gref (accessed April 2024)
- 22Abatacept, adalimumab, etanercept and tocilizumab for treating juvenile idiopathic arthritis. National Institute for Health and Care Excellence. 2015. https://www.nice.org.uk/guidance/ta373 (accessed April 2024)
- 23Thomaidou E, Ramot Y. Injection site reactions with the use of biological agents. Dermatologic Therapy. 2019;32:e12817. https://doi.org/10.1111/dth.12817
- 24Patel SV, Khan DA. Adverse Reactions to Biologic Therapy. Immunology and Allergy Clinics of North America. 2017;37:397–412. https://doi.org/10.1016/j.iac.2017.01.012
- 25Hartley K. Management of Injection Site Reactions Associated with Subcutaneous Biologic Injection. Newcastle upon Tyne Hospitals NHS Foundation Trust Pharmacy Department 2021.
- 26Beukelman T, Haynes K, Curtis JR, et al. Rates of malignancy associated with juvenile idiopathic arthritis and its treatment. Arthritis & Rheumatism. 2012;64:1263–71. https://doi.org/10.1002/art.34348
- 27Remicade 100mg powder for concentrate for solution for infusion. Electronic Medicines Compendium. 2024. https://www.medicines.org.uk/emc/product/3831/smpc#gref (accessed April 2024)
- 28Aragon Cuevas O, Hedrich CM. Biosimilars in pediatric rheumatology and their introduction into routine care. Clinical Immunology. 2020;216:108447. https://doi.org/10.1016/j.clim.2020.108447
- 29Humira 40 mg solution for injection in pre-filled syringe. Electronic Medicines Compendium. 2021. https://www.medicines.org.uk/emc/product/2150/smpc#gref (accessed April 2024)
- 30Bots S, Vande Casteele N, Brandse JF, et al. Antibody development against biologic agents used for the treatment of inflammatory bowel disease and antibody prevention with immunosuppressives. Cochrane Database of Systematic Reviews. 2016. https://doi.org/10.1002/14651858.cd012147
- 31Cronstein BN. Methotrexate BAFFles anti-drug antibodies. Nat Rev Rheumatol. 2018;14:505–6. https://doi.org/10.1038/s41584-018-0064-y
- 32Hsu L, Armstrong AW. Anti-drug antibodies in psoriasis: a critical evaluation of clinical significance and impact on treatment response. Expert Review of Clinical Immunology. 2013;9:949–58. https://doi.org/10.1586/1744666x.2013.836060
- 33Lovell DJ, Ruperto N, Goodman S, et al. Adalimumab with or without Methotrexate in Juvenile Rheumatoid Arthritis. N Engl J Med. 2008;359:810–20. https://doi.org/10.1056/nejmoa0706290
- 34Holroyd CR, Seth R, Bukhari M, et al. The British Society for Rheumatology biologic DMARD safety guidelines in inflammatory arthritis. Rheumatology. 2018;58:e3–42. https://doi.org/10.1093/rheumatology/key208
- 35De Benedetti F, Brunner HI, Ruperto N, et al. Randomized Trial of Tocilizumab in Systemic Juvenile Idiopathic Arthritis. N Engl J Med. 2012;367:2385–95. https://doi.org/10.1056/nejmoa1112802
- 36Clinical Commissioning Policy Canakinumab for patients with Still’s disease refractory to anakinra and tocilizumab (adults and children 2 years and over) 2002 . NHS England. 2002. https://www.england.nhs.uk/wp-content/uploads/2022/10/2002-cc-policy-cnakinumab-updated.pdf (accessed April 2024)
- 37Quartier P, Allantaz F, Cimaz R, et al. A multicentre, randomised, double-blind, placebo-controlled trial with the interleukin-1 receptor antagonist anakinra in patients with systemic-onset juvenile idiopathic arthritis (ANAJIS trial). Annals of the Rheumatic Diseases. 2010;70:747–54. https://doi.org/10.1136/ard.2010.134254
- 38Benedetti FD, Ruperto N, Lovell D, et al. THU0503 Identification of optimal subcutaneous (SC) doses of tocilizumab in children with polyarticular-course juvenile idiopathic arthritis (PCJIA). Poster Presentations. 2017. https://doi.org/10.1136/annrheumdis-2017-eular.2483
- 39Lauper K, Mongin D, Iannone F, et al. Comparative effectiveness of subcutaneous tocilizumab versus intravenous tocilizumab in a pan-European collaboration of registries. RMD Open. 2018;4:e000809. https://doi.org/10.1136/rmdopen-2018-000809
- 40ORENCIA 250 mg powder for concentrate for solution for infusion. Electronic Medicines Compendium. 2021. https://www.medicines.org.uk/emc/product/334/smpc#gref (accessed April 2024)
- 41BNF for Children. MedicinesComplete. 2024. http://www.medicinescomplete.com (accessed April 2024)
- 42Truxima 500 mg concentrate for solution for infusion {equilateral_black_triangle}. Electronic Medicines Compendium. 2022. https://www.medicines.org.uk/emc/product/9701/smpc (accessed April 2024)
- 43Cohen SB, Emery P, Greenwald MW, et al. Rituximab for rheumatoid arthritis refractory to anti–tumor necrosis factor therapy: Results of a multicenter, randomized, double‐blind, placebo‐controlled, phase III trial evaluating primary efficacy and safety at twenty‐four weeks. Arthritis & Rheumatism. 2006;54:2793–806. https://doi.org/10.1002/art.22025
- 44Alexeeva EI, Valieva SI, Bzarova TM, et al. Efficacy and safety of repeat courses of rituximab treatment in patients with severe refractory juvenile idiopathic arthritis. Clin Rheumatol. 2011;30:1163–72. https://doi.org/10.1007/s10067-011-1720-7
- 45Cosentyx 150mg solution for injection in pre-filled pen. Electronic Medicines Compendium. 2023. https://www.medicines.org.uk/emc/product/3669/smpc (accessed April 2024)
- 46Brunner HI, Foeldvari I, Alexeeva E, et al. Secukinumab in enthesitis-related arthritis and juvenile psoriatic arthritis: a randomised, double-blind, placebo-controlled, treatment withdrawal, phase 3 trial. Ann Rheum Dis. 2022;82:154–60. https://doi.org/10.1136/ard-2022-222849
- 47Ruperto N, Brunner HI, et al. Pharmacokinetic and safety profile of tofacitinib in children with polyarticular course juvenile idiopathic arthritis: results of a phase 1, open-label, multicenter study. Pediatr Rheumatol. 2017;15. https://doi.org/10.1186/s12969-017-0212-y
- 48Ruperto N, Brunner HI, Synoverska O, et al. Tofacitinib in juvenile idiopathic arthritis: a double-blind, placebo-controlled, withdrawal phase 3 randomised trial. The Lancet. 2021;398:1984–96. https://doi.org/10.1016/s0140-6736(21)01255-1
- 49Aragon C, Hedrich C. Biosimilars in pediatric rheumatology and their introduction into routine care. Clin Immunol. 2020;216:108447.
- 50Moots R, Azevedo V, Dörner T, et al. Switching to Biosimilars in Rheumatology: Evidence-Based Practice. American College of Rheumatology. 2016. https://acrabstracts.org/abstract/switching-to-biosimilars-in-rheumatology-evidence-based-practice/ (accessed April 2024)
- 51Lauret A, Moltó A, Abitbol V, et al. OP0227 EFFECTS OF SUCCESSIVE SWITCHES TO DIFFERENT BIOSIMILARS INFLIXIMAB ON IMMUNOGENICITY IN CHRONIC INFLAMMATORY DISEASES IN DAILY CLINICAL PRACTICE. Oral Presentations. 2019. https://doi.org/10.1136/annrheumdis-2019-eular.3702
- 52Biosimilar medicines. National Institute for Health and Care Excellence. 2018. https://www.nice.org.uk/advice/ktt15 (accessed April 2024)
- 53UK JIA Biologics Register. British Society for Rheumatology. 2024. https://www.rheumatology.org.uk/improving-care/registers/juvenile-idiopathic-arthritis (accessed April 2024)


