Shutterstock.com
Juvenile idiopathic arthritis (JIA) is an autoimmune disease whereby the body’s immune system fails to distinguish between self and non-self. The cells of the synovium — connective soft-tissue membrane that lines the inner surface of synovial joint capsules — are recognised as foreign, leading to an immune cell attack and inflammation, causing arthritis[1]. The impact of a JIA diagnosis can have a profound effect on the person and their family; it can affect emotional wellbeing and educational achievements, particularly in adolescence[2]. JIA is the leading cause of musculoskeletal disability in children and is distinct from adult rheumatoid arthritis[1]. JIA affects approximately 1 in 1,000 children in the UK and is defined as persistent joint inflammation that lasts for at least 6 weeks with onset before the age of 16 years[3]. As suggested by its name, JIA includes all types of arthritis with no apparent cause, with its aetiology not fully described[4]. Data suggest that 10–15% of children with JIA will also have uveitis[5].
The International League of Associations for Rheumatology (ILAR) has defined subtypes based on clinical presentations (including the type and number of joints involved in conjunction with symptoms) and biochemical markers, such as rheumatoid factor (see Table 1)[6–8].
The involvement of systemic inflammation makes systemic JIA (sJIA) distinct from other subtypes owing to its association with macrophage activation syndrome (MAS), a severe life-threatening complication[9]. MAS (sometimes called haemophagocytic lymphohistiocytosis [HLH]) is the resultant uncontrolled activation and proliferation of T lymphocytes and macrophages, which typically presents as fever, seizures, hypotension, purpura, hepatitis, splenomegaly and, occasionally, multi-system organ failure[4]. MAS occurs during active disease phases or at disease onset.
Advances in JIA treatments with novel agents, such as biologics, enable patients with JIA to live not only with suppressed symptoms but also with immunologically inactive disease. In one-third of patients, JIA symptoms can persist into adulthood[6]. The mortality rate is 0.3% to 1.0%, with 5.0% of patients having a physical disability of Class III (limited to few or no activities of the patient’s usual occupation) or Class IV (bedridden with little or no self-care), according to the four-level Stein-Brocker functional classification scale[6].
This article will cover classification of the different types of JIA, recognition and diagnosis and conventional pharmacological management of the condition, information on management of JIA with biologic disease modifying anti-rheumatic drugs can be found in ‘Juvenile idiopathic arthritis: biologic disease modifying anti-rheumatic drugs’.
Recognition and diagnosis
The aetiology of JIA is still poorly understood and has been associated with the influence of immunogenic mechanisms secondary to genetic, environmental and infection factors[8]. T-lymphocytes are found in the synovial fluid of JIA patients, causing the activation of macrophages to produce interleukin (IL)-1, IL-6 and tumour necrosis factor-alpha (TNF-ɑ)[10].
There is no diagnostic test for JIA and a clinical diagnosis is made based on history and examination. The British Society for Rheumatology (BSR) provides a statement of the standards of care for children and young people with JIA[2]. Paediatric musculoskeletal assessment tools like the Gait Arms Legs Spine (pGALS), ultrasound, X-rays and MRI are commonly used to help diagnose and detect early inflammation and monitor subsequent joint diseases[11]. The Paediatric Musculoskeletal Matters website provides useful online learning information on the clinical assessment of children with musculoskeletal problems[12].
Laboratory results can aid the diagnosis of MAS. Laboratory features include hyperferritinemia, thrombocytopenia, anaemia, leukopenia, coagulopathy and elevated levels of C-reactive protein and D-dimer[6]. Regular specialist ophthalmology reviews reviews are also required because uveitis, despite often being asymptomatic, can be sight-threatening[5].
Management of JIA
The multidisciplinary team (MDT) is essential in managing a child in the children’s rheumatology service and enables holistic and equitable access to care. The team should comprise consultant paediatric rheumatologists and ophthalmologists, paediatric clinical nurse specialists, physiotherapists, occupational therapists, psychologists and colleagues in community care[1,2]. Pharmacists can provide advice on complex medicines, including funding and prescribing roles (in some cases). All members of the MDT should have received appropriate training and experience in paediatric rheumatology.
The MDT can help to manage and provide:
- Information on specialist medicines, which can include unlicensed medicines;
- Advice on procedural anxiety;
- Advice for people with needle phobia for both injectable medicines and blood monitoring;
- Advice on alternative formulations of medicines to improve patient concordance;
- Advice for techniques on administration of injectable and oral medicines;
- Lifestyle interventions for optimising disease control[1,2].
Drug management and best practice in JIA
The goals of medical management of JIA is to eliminate active disease, to normalise joint function, to preserve normal growth and to prevent long-term damage of joints[13,14]. In recent years, two major trends have emerged in the drug treatment of auto-inflammatory conditions. First, the concept of a ‘window of opportunity’ suggests that targeting the disease early and aggressively to ‘switch off’ the immune process can lead to better long-term outcomes[15]. Second, ‘treat-to-target’ is now being applied to the management of JIA. This approach states that tighter disease control can be achieved by formally measuring and tracking patient outcomes, looking to achieve not just clinical but also immunological remission. Immunological remission is becoming measurable using increasingly sensitive biochemical and radiological markers, even in the absence of clinically apparent disease[16].
Non-steroidal anti-inflammatory drugs
At initial diagnosis and at any point during a flare-up, non-steroidal anti-inflammatory drugs (NSAIDs) can be used to bridge the starting effect of other therapies, but they are no longer used alone to treat JIA[6]. NSAIDs can control inflammation if used regularly at optimised doses but will not induce remission in the long term. An individual may fail to respond to one type of NSAID but have a good therapeutic response to another[17]. Preparation, side effects and dosing frequency need to be taken into account when prescribing NSAIDs. For patients regularly taking NSAIDs, co-prescription of a gastro-protective agent should be considered, particularly if there is any history of indigestion, stomach ulcers or bleeding[18]. Active gastrointestinal bleeding is a contraindication for NSAID use[19]. Both NSAIDs and PPIs have the potential to interact with methotrexate reducing its clearance, which may increase the risk of methotrexate-related adverse drug events[18]. Concomitant use is not contraindicated but they should be used with caution alongside appropriate blood monitoring to detect methotrexate-related toxicity (see monitoring of methotrexate)[18].
Specific JIA recommended doses of NSAIDs should be prescribed[19]. For agents such as ibuprofen, the JIA recommended dose can be twice as much as an over-the-counter dose, so the patient and parent/carer education should include that caveat. Ibuprofen is the only NSAID of choice licensed for use in JIA in children aged under five years and it is also widely available as a liquid formulation[19,20]. Diclofenac is available as a liquid formulation unlicensed special[21]. Naproxen is licensed for children aged five years and older for JIA and is available as a liquid formulation, but it does contain significant amounts of sorbitol, which can cause diarrhoea [22]. While naproxen is expensive in comparison to ibuprofen, it offers the advantage of twice-daily dosing[22]. Slow-release preparations can help with morning pain and stiffness symptoms until other systemic therapies start affecting the disease course[17].
Intra-articular corticosteroids
Some cases of oligo-JIA can be controlled by intra-articular corticosteroids (IACs) on their own without the need to expose the patient to systemic immunosuppressants[23]. They can also be used for ‘bridging’ in extended oligo and poly-JIA flare ups, providing relief until the systemic treatment becomes fully effective[23]. The IAC of choice in JIA is triamcinolone hexacetonide, which can be used alongside intra-articular lidocaine 1% or normal saline (used to flush the needle track after the IAC injection to avoid skin changes caused by leakage) at different doses depending on the size of the joint[24]. The hexacetonide salt is less soluble than other salts, attaining synovial levels for a longer period of time. There is no stipulated maximum number of joints that can be injected in one visit with this product; however, from a practical point of view, consideration for systemic corticosteroids should take place if there are more than eight affected joints[25,26]. There has been a worldwide shortage of triamcinolone hexacetonide since early 2022[27]. If this product cannot be sourced, triamcinolone acetonide (not equipotent, so different doses will apply), which is the first line treatment for inflamed temporomandibular joints, can be considered[19].
Systemic corticosteroids
Given orally, intramuscularly or intravenously, systemic corticosteroids (SyC) have immediate, potent anti-inflammatory properties mediated by the inhibition of several cytokines. However, prolonged use should be avoided in children owing to their effects on bone homeostasis, growth, weight gain and neuropsychiatric symptoms[19,28]. Any child started on a course of SyC should be given a blue steroid card, which contains general advice for patients receiving steroids and can be used to record the current steroid treatment regime. It should be used for children receiving IV or IM methylprednisolone pulses (short, high-dose SyC therapy) but might not be necessary when sporadic IAC injections are used[29].
The UK Health Security Agency’s Green Book for immunisations, which has the latest information on vaccines and vaccination procedures, suggests that significant immunosuppression should be expected in children on doses of prednisolone equivalent to 2mg/kg/day for over 1 week, OR more than 40mg/day for over 1 week, OR 1mg/kg/day for over 2 weeks[30]. Live vaccines should be avoided in patients who have received any such courses in the past three months[29]. Prednisolone (available as 1mg, 5mg and 25mg tablets, oral solution and soluble tablets) is the usual oral SyC of choice in the UK. Once daily dosing (preferably in the morning to mimic physiological cortisol production) and a variety of available formulations can aid with patient treatment adherence[28]. The usual maximum oral dose used in JIA is 60mg once daily (if weight allows)[19]. IV methylprednisolone sodium succinate can be given as ‘pulsed therapy’. IV methylprednisolone pulses can range from 10–30mg/kg (ceiling dose of 1,000mg), given on three to five consecutive days, sometimes over one to two weeks. Monthly pulses are also sometimes recommended alongside biologic therapy[14,26]. Methylprednisolone administration may vary from centre to centre. The Medusa Guidelines can be used to recommend infusion strategies and suggested monitoring[31].
Despite SyC being used for decades in the management of childhood auto-immune rheumatological conditions, there is very little evidence with regards to the best SyC of choice or type of treatment regimens, including method of weaning high doses of SyC[32]. Many clinical trials have tried to address this evidence gap in recent years: the SIRJIA trial established a clear need for the development of a randomised controlled trial to compare different corticosteroid induction regimens in children and young people with JIA using a mixed methods approach (qualitative questionnaires alongside critical appraisal of the literature)[31]. The first randomised controlled clinical trial to compare IV methylprednisolone versus oral prednisolone for induction of remission in poly course JIA (STAR-JIA) has opened for recruitment in 2024[33].
Conventional disease modifying anti-rheumatic drugs
Methotrexate
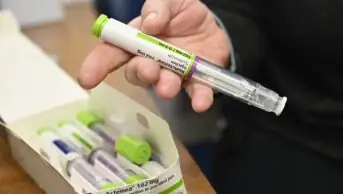
Methotrexate is the first-line disease modifying anti-rheumatic drugs (DMARD) for children with JIA. It is a cytotoxic agent with immunosuppressive properties that acts to antagonise folic acid in the body[34]. Dosing is based on body surface area and is usually 10-15mg/m2 by subcutaneous injection or mouth once a week. Low-dose once weekly methotrexate has been the subject of several drug safety alerts. Most recently in 2020, continuing reports of inadvertent overdose prompted a series of measures including recording the day of the week on which the dose is to be taken in an attempt to prevent fatal overdose[34]. Communication with families to prevent daily dosing is essential[35].
Optimal dosing of methotrexate for at least 12 weeks is needed before assessment of efficacy, although improvement in symptoms can occur sooner than this in some patients[36]. Most patients should trial methotrexate before consideration of a biologic therapy; however, patients with systemic JIA and associated HLH, those presenting with axial JIA or sacroiliitis do not need to trial methotrexate before starting a biologic[37].
Methotrexate is structurally very similar to folic acid and competes with folic acid for the synthesis of purine nucleotides essential for the synthesis of DNA and hence for cell division; the most rapidly dividing cells are the ones that are affected to the greatest extent[37,38]. These are the cells of the bone marrow, GI tract, skin and hair, hence the side effects of bone marrow suppression and consequent immunosuppression, nausea and vomiting, mouth ulcers and hair thinning. Hair loss has been reported with both high dose and low dose methotrexate; however, it is also possible that hair loss may be a consequence of untreated inflammation and so it may be possible to reassure patients and their families that any hair thinning is likely to reduce as the JIA becomes better controlled[33,39,40].
Nausea and vomiting may occur following and prior to methotrexate doses (anticipatory nausea)[3]. Various actions can help, including the addition of folic acid and giving ondansetron at least one hour before the methotrexate dose and regularly for the following 24-48 hours, if nausea persists. Giving the dose at night can be helpful. Psychological support may be needed for those suffering from anticipatory nausea[3].
Another principal side effect of methotrexate is hepatotoxicity and careful monitoring, including full blood count, liver and kidney function, is required[33]. There have been some reports of a significant reduction in hepatic dysfunction when methotrexate is supplemented with folic acid[41]. Folic acid has also been found to help with methotrexate induced mouth ulcers. Dosing varies widely but 5mg once a week or 1mg every day, other than the day of methotrexate, are common regimens and appear not to reduce the efficacy of methotrexate[41]. Some centres routinely use higher folic acid doses. Addition of folic acid or folinic acid to methotrexate has been shown to reduce the number of patients discontinuing treatment and is often started routinely alongside methotrexate[38,39]. Folic acid and folinic acid have both been found to be effective, however folic acid is a more cost-effective folate supplement[41].
Vaccination, both live and non-live, may be less effective when a patient is immunosuppressed. The immunosuppression associated with methotrexate does not require the avoidance of live vaccines if the dose is kept below 15mg/m2 per week[29]. Methotrexate is a known teratogen and must be avoided in pregnancy[42]. Caution around handling cytotoxic medications should be discussed with patients and their carers if they will be administering the medication[43].
Sulfasalazine
Used off-label, sulfasalazine can be a useful alternative DMARD for children who cannot tolerate methotrexate[44]. The disadvantages include a twice-daily dosage regimen and relatively large tablets or relatively large volume liquid preparations. Despite these issues most children appear to manage well on sulfasalazine and it is an effective drug for JIA[43].
Dosage is usually increased over a few weeks until a maintenance dose of 20–25mg/kg per day in two divided doses (maximum 1g twice daily) is reached. Sulfasalazine can cause profound bone marrow suppression and appropriate monitoring for haematological abnormalities should be undertaken. The risk is greatest in the first three to six months of treatment[19]. Patients and their families should be warned that sulfasalazine can cause tears, urine and other body secretions to be tinged orange. This may be of particular concern for contact lens wearers who may find that their contact lenses become stained[19].
Sulfasalazine is less immunosuppressive than methotrexate and children can receive live vaccines if they are receiving no other immunosuppression (and have not had immunosuppressive doses of steroid in the recent past). It does not usually need to be stopped during intercurrent illness; however, if a child is likely to be dehydrated (for example because of pyrexia or severe gastric upset), it is advised to withhold sulfasalazine until the child is better. Sulfasalazine causes crystalluria and kidney stone formation, which can be potentiated by inadequate hydration[45].
Sulfasalazine should not be used by patients with aspirin (or any other salicylate) or sulfonamide allergy[43].
Leflunomide
Leflunomide is not licensed for children. It has been shown to be effective in JIA, although methotrexate has shown a greater response when the two are directly compared[45–47]. It is an inhibitor of pyrimidine synthesis, which blocks lymphocyte activation and inflammatory response and is available as 10mg or 20mg tablets[19].
It is generally better tolerated than methotrexate and can be a useful alternative when patients have discontinued methotrexate because of side effects. The manufacturer recommends a loading dose over the first three days[48]; however, this has been found to be associated with more side effects, particularly gastrointestinal and liver effects, and many prescribers prefer to omit the loading doses.
Leflunomide has a very long elimination half-life (one to four weeks) and is suspected to cause birth defects if taken during pregnancy[19]. Women of childbearing potential are required to use effective contraception both during leflunomide use and for two years after stopping leflunomide. This is a conversation that should be had with young females before they start taking leflunomide and at regular intervals, and effective contraception arranged if necessary[19].
Live vaccines should not be given while on leflunomide[47].
Choice of conventional disease-modifying anti-rheumatic drugs
Methotrexate is the preferred first line cDMARD and is effective against both arthritis and uveitis[49]. Sulfasalazine although generally less effective than methotrexate for arthritis has been shown to reduce attacks of HLAB27 associated uveitis in adults and children[43,50]. Leflunomide, while having efficacy against JIA, appears to be less effective than methotrexate for JIA associated uveitis[45,46]. Leflunomide is associated with a higher flare rate compared to methotrexate in the treatment of chronic uveitis in juvenile idiopathic arthritis[51].
Monitoring of conventional disease-modifying anti-rheumatic drugs
Monitoring schedules for methotrexate, sulfasalazine and leflunomide have been recommended by the British Society of Rheumatology (BSR) for adult patients with rheumatoid arthritis[52]. Centres that treat children generally adapt these guidelines for the use in children[53]. The BSR recommends the following tests: full blood count, creatinine/calculated glomerular filtration rate, liver transaminases and albumin every two weeks until on stable dose for six weeks. The same tests should be carried out monthly for three months and then at least every twelve weeks for the duration of treatment. Additional monitoring is recommended when doses are increased[52].
Blood pressure and weight at each monitoring visit is additionally recommended for leflunomide. Sulfasalazine monitoring does not need to continue past 12 months if the patient’s previous results have not shown abnormalities[52].
In practice, children often find having blood tests traumatic and so regimens for monitoring may be pragmatically adjusted unless the child has significant comorbidity that pre-disposes them to liver or haematological abnormalities.
Patient advice and counselling
Patients and their families should be given clear advice about risks of infection when starting any immunomodulating therapy. This should include:
- What to do if they develop or are in contact with infectious diseases including specific advice about chicken pox, measles and COVID-19[54–56];
- Advice around live and non-live vaccines: this advice will depend on both the current medication and medication received in the recent past (e.g. a recent course of oral steroids may preclude live vaccine despite current medication being insufficiently immunosuppressive to warrant avoidance of live vaccines[29]);
- Travel advice: families may need letters to allow them to travel with medication in hand luggage and advice may be needed about travel vaccines;
- General advice about simple hygiene measures to reduce infection, such as hand washing may also be given;
- Patients should be given a contact number of their specialist team and should also carry any patient alert card issued by the manufacturer of their medication.
Useful resources
Guidelines
- Pediatric Rheumatology INternational Trials Organisation (PRINTO);
- Versus Arthriti: ‘Juvenile idiopathic arthritis‘;
- British Society for Rheumatology: (paediatric and adolescence sections).
Charities
- 1Scott C, Brice N. Juvenile idiopathic arthritis – an update on its diagnosis and management. S Afr Med J. 2015;105:1077. https://doi.org/10.7196/samj.2015.v105i12.10223
- 2Davies K, Cleary G, Foster H, et al. BSPAR Standards of Care for children and young people with juvenile idiopathic arthritis. Rheumatology. 2010;49:1406–8. https://doi.org/10.1093/rheumatology/kep460
- 3Foster HE, Brogan PA, editors. Paediatric Rheumatology. Oxford University Press 2018. https://doi.org/10.1093/med/9780198738756.001.0001
- 4Petty R, Southwood T, Manners P, et al. International League of Associations for Rheumatology classification of juvenile idiopathic arthritis: second revision, Edmonton, 2001. J Rheumatol. 2004;31:390–2.
- 5Rypdal V, Glerup M, Songstad NT, et al. Uveitis in Juvenile Idiopathic Arthritis. Ophthalmology. 2021;128:598–608. https://doi.org/10.1016/j.ophtha.2020.08.024
- 6Martini A, Ravelli A, Avcin T, et al. Toward New Classification Criteria for Juvenile Idiopathic Arthritis: First Steps, Pediatric Rheumatology International Trials Organization International Consensus. J Rheumatol. 2018;46:190–7. https://doi.org/10.3899/jrheum.180168
- 7Momah T, Ray L. Juvenile idiopathic arthritis: Old disease, new tactics. J Fam Pract. 2019;68:E8–13.
- 8Rigante D, Bosco A, Esposito S. The Etiology of Juvenile Idiopathic Arthritis. Clinic Rev Allerg Immunol. 2014;49:253–61. https://doi.org/10.1007/s12016-014-8460-9
- 9Bracaglia C, Prencipe G, De Benedetti F. Macrophage Activation Syndrome: different mechanisms leading to a one clinical syndrome. Pediatr Rheumatol. 2017;15. https://doi.org/10.1186/s12969-016-0130-4
- 10Zaripova LN, Midgley A, Christmas SE, et al. Juvenile idiopathic arthritis: from aetiopathogenesis to therapeutic approaches. Pediatr Rheumatol. 2021;19. https://doi.org/10.1186/s12969-021-00629-8
- 11Foster HE, Jandial S. pGALS – paediatric Gait Arms Legs and Spine: a simple examination of the musculoskeletal system. Pediatr Rheumatol. 2013;11. https://doi.org/10.1186/1546-0096-11-44
- 12Clinical assessment. Paediatric Musculoskeletal Matters Online. 2024. https://www.pmmonline.org/doctor/clinical-assessment (accessed April 2024)
- 13Hayward K, Wallace CA. Recent developments in anti-rheumatic drugs in pediatrics: treatment of juvenile idiopathic arthritis. Arthritis Res Ther. 2009;11:216. https://doi.org/10.1186/ar2619
- 14James RA, Wedderburn LR. Modern management of juvenile idiopathic arthritis. Prescriber. 2016;27:37–43. https://doi.org/10.1002/psb.1472
- 15Wallace CA, Giannini EH, Spalding SJ, et al. Trial of early aggressive therapy in polyarticular juvenile idiopathic arthritis. Arthritis & Rheumatism. 2012;64:2012–21. https://doi.org/10.1002/art.34343
- 16Consolaro A, Negro G, Lanni S, et al. Toward a treat-to-target approach in the management of juvenile idiopathic arthritis. Clin Exp Rheumatol. 2012;30:S157-62.
- 17Ardoin SP, Sundy JS. Update on nonsteriodal anti-inflammatory drugs. Current Opinion in Rheumatology. 2006;18:221–6. https://doi.org/10.1097/01.bor.0000218940.04613.cc
- 18Dowd JE, Cimaz R, Fink CW. Nonsteroidal antiinflammatory drug‐induced gastroduodenal injury in children. Arthritis & Rheumatism. 1995;38:1225–31. https://doi.org/10.1002/art.1780380908
- 19Paediatric Formulary Committee. BNF for Children . Medicines Complete. http://www.medicinescomplete.com (accessed April 2024)
- 20Pinewood Healthcare. Ibuprofen 100mg/5mL Oral Suspension SmPC. Electronic Medicines Compendium. 2023. https://www.medicines.org.uk/emc/product/4560/smpc#gref (accessed April 2024)
- 21Diclofenac sodium. BNF-C. https://bnfc.nice.org.uk/drugs/diclofenac-sodium/ (accessed April 2024)
- 22Thornton & Ross Ltd. Naproxen 50mg/1mL Oral Suspension SmPC. Electronic Medicines Compendium. 2022. https://www.medicines.org.uk/emc/product/11105/smpc#gref (accessed April 2024)
- 23Cleary AG. Intra-articular corticosteroid injections in juvenile idiopathic arthritis. Archives of Disease in Childhood. 2003;88:192–6. https://doi.org/10.1136/adc.88.3.192
- 24Job-Deslandre C, Menkes C. Complications of intra-articular injections of triamcinolone hexacetonide in chronic arthritis in children. Clin Exp Rheumatol. 1990;8:413–6.
- 25Sherry DD, Stein LD, Reed AM, et al. Prevention of leg length discrepancy in young children with pauciarticular juvenile rheumatoid arthritis by treatment with intraarticular steroids. Arthritis & Rheumatism. 1999;42:2330–4.26Zulian F. Triamcinolone acetonide and hexacetonide intra-articular treatment of symmetrical joints in juvenile idiopathic arthritis: a double-blind trial. Rheumatology. 2004;43:1288–91. https://doi.org/10.1093/rheumatology/keh31327UK drug shortages list. Clinigen Direct UK. 2024. https://www.clinigengroup.com/direct/en/shortages-list/?parentId=&page=3&countryCode=en&sortType=0&prodName= (accessed April 2024)28Prieur A. The place of corticosteroid therapy in juvenile chronic arthritis in 1992. J Rheumatol Suppl. 1993;37:32–4.29Position statement 2021-02 Use of Steroid Medication Warning Cards for Children and Young People. Neonatal and Paediatric Pharmacist Group. 2021. https://nppg.org.uk/wp-content/uploads/2021/12/Position-Statement-Steroid-Cards-V1.pdf (accessed April 2024)30Contraindications and special considerations. UK Health Security Agency. 2017. https://www.gov.uk/government/publications/contraindications-and-special-considerations-the-green-book-chapter-6 (accessed April 2024)31Medusa – the Injectable Medicines Guide. Medusa – the Injectable Medicines Guide. https://www.medusaimg.nhs.uk (accessed April 2024)32Jones AP, Clayton D, Nkhoma G, et al. Different corticosteroid induction regimens in children and young people with juvenile idiopathic arthritis: the SIRJIA mixed-methods feasibility study. Health Technol Assess. 2020;24:1–152. https://doi.org/10.3310/hta2436033Steroid TreAtment TRial in JIA (STAR-JIA): a randomised trial to compare effectiveness, safety and cost-effectiveness of intravenous versus oral corticosteroid induction regimens for children and young people with juvenile idiopathic arthritis. National Institute for Health and Care Research. 2023. https://fundingawards.nihr.ac.uk/award/NIHR134350 (accessed April 2024)34Martindale, the complete drug reference. Pharmaceutical Press. 2017. https://www.pharmaceuticalpress.com/products/martindale-the-complete-drug-reference (accessed April 2024)35Cronstein BN, Aune TM. Methotrexate and its mechanisms of action in inflammatory arthritis. Nat Rev Rheumatol. 2020;16:145–54. https://doi.org/10.1038/s41584-020-0373-936Ringold S, Angeles‐Han ST, Beukelman T, et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Treatment of Juvenile Idiopathic Arthritis: Therapeutic Approaches for Non‐Systemic Polyarthritis, Sacroiliitis, and Enthesitis. Arthritis & Rheumatology. 2019;71:846–63. https://doi.org/10.1002/art.4088437NHS England Clinical commissioning policy statement: biologic therapies for the treatment of juvenile idiopathic arthritis. NHS England. 2015. https://www.england.nhs.uk/commissioning/wp-content/uploads/sites/12/2015/10/e03pd-bio-therapies-jia-oct15.pdf (accessed April 2024)38Rang H. Rang & Dale’s pharmacology. 8th ed. Philadelphia : Elsevier Churchill Livingstone 2016. https://search.worldcat.org/title/Rang-and-Dale’s-pharmacology/oclc/904420215 (accessed April 2024)39Methotrexate once-weekly for autoimmune diseases: new measures to reduce risk of fatal overdose due to inadvertent daily instead of weekly dosing. Medicines and Healthcare products Regulatory Agency. 2020. https://www.gov.uk/drug-safety-update/methotrexate-once-weekly-for-autoimmune-diseases-new-measures-to-reduce-risk-of-fatal-overdose-due-to-inadvertent-daily-instead-of-weekly-dosing (accessed April 2024)40Harrison S, Bergfeld W. Diffuse hair loss: Its triggers and management. CCJM. 2009;76:361–7. https://doi.org/10.3949/ccjm.76a.0808041Shea B, Swinden MV, Ghogomu ET, et al. Folic Acid and Folinic Acid for Reducing Side Effects in Patients Receiving Methotrexate for Rheumatoid Arthritis. J Rheumatol. 2014;41:1049–60. https://doi.org/10.3899/jrheum.13073842Russell MD, Dey M, Flint J, et al. British Society for Rheumatology guideline on prescribing drugs in pregnancy and breastfeeding: immunomodulatory anti-rheumatic drugs and corticosteroids. Rheumatology. 2022;62:e48–88. https://doi.org/10.1093/rheumatology/keac55143Administering subcutaneous methotrexate for inflammatory arthritis. Royal College of Nursing . 2021. https://www.rcn.org.uk/-/media/Royal-College-Of-Nursing/Documents/Publications/2021/October/009-675.pdf (accessed April 2024)44Brooks C. Sulfasalazine for the management of juvenile rheumatoid arthritis. J Rheumatol. 2001;28:845–53.45Rosemont Pharmaceuticals limited Sulfasalazine 250mg/5ml Oral SmPC. Electronic Medicines Compendium. 2023. https://www.medicines.org.uk/emc/product/413/smpc (accessed April 2024)46Bichler J, Benseler S, Krumrey-Langkammerer M, et al. Leflunomide is associated with a higher flare rate compared to methotrexate in the treatment of chronic uveitis in juvenile idiopathic arthritis. Scandinavian Journal of Rheumatology. 2015;44:280–3. https://doi.org/10.3109/03009742.2015.101398347FOELDVARI I, WIERK A. Effectiveness of Leflunomide in Patients with Juvenile Idiopathic Arthritis in Clinical Practice. J Rheumatol. 2010;37:1763–7. https://doi.org/10.3899/jrheum.09087448Sanofi. Arava 10mg tablets SmPC. Electronic Medicines Compendium. 2022. https://www.medicines.org.uk/emc/product/4056/smpc (accessed April 2024)49Constantin T, Foeldvari I, Anton J, et al. Consensus-based recommendations for the management of uveitis associated with juvenile idiopathic arthritis: the SHARE initiative. Ann Rheum Dis. 2018;annrheumdis-2018-213131. https://doi.org/10.1136/annrheumdis-2018-21313150Heiligenhaus A, Minden K, Tappeiner C, et al. Update of the evidence based, interdisciplinary guideline for anti-inflammatory treatment of uveitis associated with juvenile idiopathic arthritis. Seminars in Arthritis and Rheumatism. 2019;49:43–55. https://doi.org/10.1016/j.semarthrit.2018.11.00451Silverman E, Mouy R, Spiegel L, et al. Leflunomide or Methotrexate for Juvenile Rheumatoid Arthritis. N Engl J Med. 2005;352:1655–66. https://doi.org/10.1056/nejmoa04181052Ledingham J, Gullick N, Irving K, et al. BSR and BHPR guideline for the prescription and monitoring of non-biologic disease-modifying anti-rheumatic drugs. Rheumatology. 2017;56:865–8. https://doi.org/10.1093/rheumatology/kew47953Paediatric and adolescent guidance. British Society for Rheumatology. 2022. https://www.rheumatology.org.uk/practice-quality/guidelines/paediatric-adolescent-guidance (accessed April 2024)54Guidelines on post exposure prophylaxis (PEP) for varicella or shingles. UK Health Secure Agency. 2023. https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/1134812/UKHSA-guidelines-on-VZ-post-exposure-prophylaxis-january-2023.pdf (accessed April 2024)55Guidelines on Post-Exposure Prophylaxis for measles. Public Health England. . 2019. https://www.gov.uk/government/publications/measles-post-exposure-prophylaxis (accessed April 2024)56COVID-19: guidance for people whose immune system means they are at higher risk. Department of Health and Social Care, UK Health Security Agency. 2023. https://www.gov.uk/government/publications/covid-19-guidance-for-people-whose-immune-system-means-they-are-at-higher-risk/covid-19-guidance-for-people-whose-immune-system-means-they-are-at-higher-risk (accessed April 2024)