Jim Holden / Alamy Stock Photo
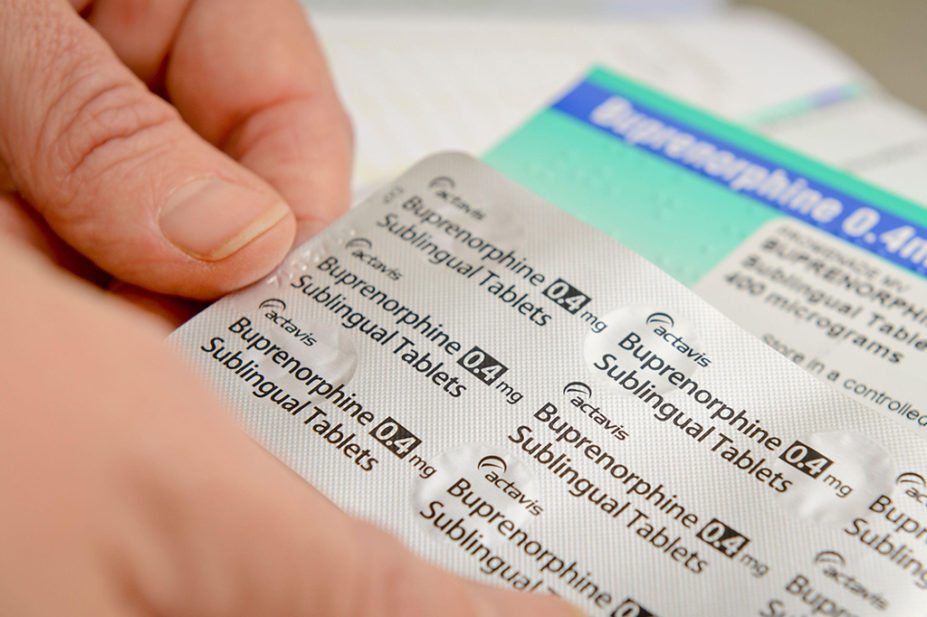
Providing a buprenorphine programme through community pharmacists could widen access to treatment for opioid withdrawal, a US ‘feasibility pilot trial’ has found.
In a small study, published as a research letter in the New England Journal of Medicine on 12 January 2023, 100 people were recruited through participating pharmacies and local hospital services in Rhode Island.
Community pharmacists at six pharmacies were trained to take the patients’ histories and opioid withdrawal symptoms, confirm the buprenorphine regimen with the study’s addiction medicine doctor, and then initiate treatment.
The study was conducted between February 2021 and April 2022. Participants were given doses for three to seven days to start with, then weekly or two-weekly thereafter.
Of the 100 patients, 58 could be stabilised on a maintenance dose. These patients were randomised and 28 were assigned to pharmacy care, while 30 were assigned to usual care (with a physician at a clinic or office).
Of the 28 patients receiving maintenance care in pharmacies, 25 continued to attend visits one month after randomisation, compared to just 5 of the 30 receiving usual care. The researchers noted that retention in pharmacy care was “substantially higher than retention in usual care”.
However, the researchers said that larger and longer trials were needed to fully determine the clinical risks and benefits of buprenorphine treatment via community pharmacy or conventional care.
In June 2022, NHS data analysed by The Pharmaceutical Journal showed that the number of adults prescribed an opioid for more than three months in England increased sharply during the COVID-19 pandemic.
Since 1 April 2022, primary care networks in England have been paid for delivering structured medicine reviews to patients in priority cohorts, such as those prescribed an oral or transdermal opioid with more than 120mg oral morphine equivalent.
Roya Vaziri, executive medical director of Humankind, a UK charity that specialises in treatment of people with drug and alcohol problems, said that community pharmacy could be “an important and engaging model to have different pathways for people to be initiated with buprenorphine”.
She added that pharmacists who were independent prescribers could theoretically take on such services.
However, Vaziri said: “There is no mechanical reason why this couldn’t apply in England, but there are challenges of service level provision.
“It would be amazing for an individual to have all their care in their local pharmacy, rather than having to travel to a hub,” she said, noting that places such as Cumbria and Devon posed geographical challenges for treatment.
However, she added that community pharmacists in the UK are currently struggling with workload and funding, which makes it hard to provide more basic harm reduction services, such as naloxone, needle and syringe exchange, and supervised consumption.
Mark Donaghy, professional development manager for multiple pharmacy chain Kamsons Pharmacy, said two of its community pharmacists have been subcontracted to a local substance misuse service for a few hours each week.
“They have been prescribing methadone and buprenorphine from our pharmacies on blue FP10 (MDA) prescriptions for about ten years,” he said.