Shutterstock.com
An investigational gene therapy has been found to be highly effective in improving the overall survival of children with a rare and life-threatening primary immunodeficiency, an analysis in the New England Journal of Medicine has suggested.
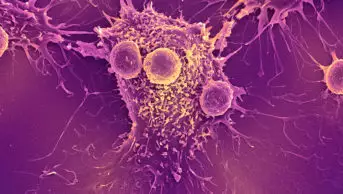
Severe combined immunodeficiency owing to adenosine deaminase (ADA) deficiency (ADA-SCID) is characterised by an impaired immune function and, without treatment, individuals with the condition will often die from infections by the age of two years.
Current guidelines recommend that patients initially receive enzyme-replacement therapy, but haematopoietic stem-cell transplantation (HSCT) or haematopoietic stem-cell gene therapy is recommended as a more definitive treatment.
In the study, researchers investigated the use of an investigational gene therapy which involves taking the patients’ own haematopoietic stem and progenitor cells and, using a viral vector, inserting the functioning gene for the human ADA enzyme. The cells are then reinfused back into the patient, in the hope that they then go on to produce ADA as normal, correcting the immunodeficiency.
The researchers carried out an integrated analysis of data from two prospective, non-randomised phase I to II clinical studies in the United States, and a separate analysis of a prospective, non-randomised phase I to II clinical study in the UK, to assess the safety and efficacy of the gene therapy in patients with ADA-SCID.
In total, 50 patients with ADA-SCID were treated with the gene therapy across the three studies — 30 in the United States (median age, 10.0 months; range, 4 to 51) and 20 in the UK (median age, 11.6 months; range, 4 to 193). All patients in the US studies and 19 of the 20 patients in the UK study were receiving enzyme-replacement therapy at the time of treatment, and all patients were receiving prophylactic antimicrobials at screening.
Across all studies, overall survival was 100% at 12 months and 24 months, and remained at 100% at 36 months for patients in the UK study. In addition, at 12 months, event-free survival was at 97% and 100% in the US and UK patients, respectively, and 97% and 95%, respectively, at 24 months. Just two patients — one in the US and one in the UK — had to have their enzyme-replacement therapy reinitiated, after the treatment failed.
At the final follow-up visit, lymphocyte counts in most patients had reached or come close to reaching the expected normal ranges for age for most lymphocyte populations.
“The high overall survival and event-free survival observed at 24 and 36 months compare favourably with survival that has been observed previously with HSCT, the current standard of care for the treatment of ADA-SCID,” the authors concluded.
Susan Walsh, chief executive of Immunodeficiency UK, welcomed the data from the trial.
“The impact of having a child affected by ADA-SCID is massive for families,” she said. “Parents live in constant fear and anxiety of their child getting a life-threatening infection, with all aspects of life, for both child and family, affected in a negative way; so we welcome the extremely positive data from this ADA-SCID gene therapy trial.
“We know, first-hand, from families that having gene therapy can be life-saving and life-changing, and these results will be hugely reassuring and informative for newly diagnosed families who are considering this treatment option.”