
Shutterstock.com
Open access article
The Royal Pharmaceutical Society has made this article free to access in order to help healthcare professionals stay informed about an issue of national importance.
To learn more about coronavirus, please visit: https://www.rpharms.com/coronavirus
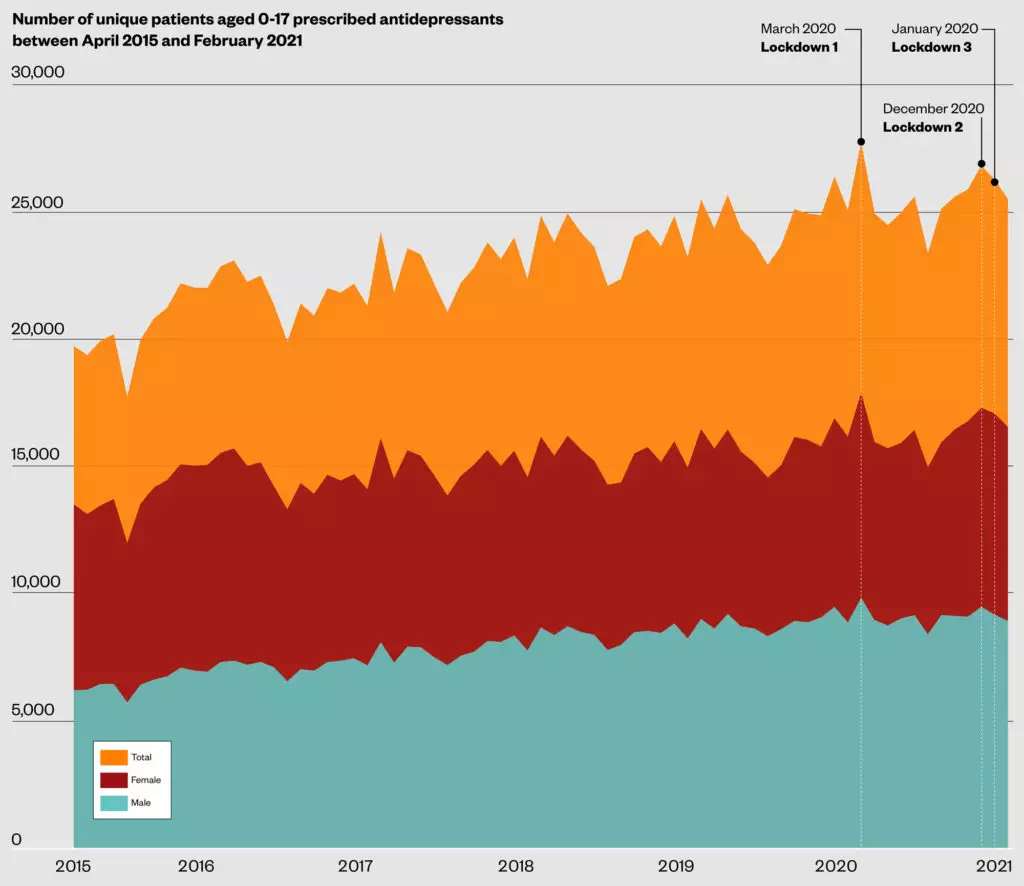
Peaks in the number of young people prescribed antidepressants in England have coincided with periods of lockdown during the COVID-19 pandemic, analysis by The Pharmaceutical Journal has found.
NHS data obtained exclusively via a freedom of information request showed a steady increase over the past five years in the number of unique patients in England aged 0-17 years who were prescribed antidepressants, which were dispensed in primary care settings.
Between April 2015 and April 2020, the number of unique patients prescribed antidepressants increased by 26%, from 19,739 to 24,957.
However, the analysis also showed that this trend appeared to accelerate during the COVID pandemic, with peaks occurring at the same time as national lockdown restrictions came into force in the UK.
In March 2020, when the first UK lockdown began, the number of unique patients prescribed antidepressants in England reached a peak, with 17,902 females and 9,855 males prescribed antidepressants; the first time the number of females prescribed antidepressants had surpassed 17,000 during the data period.
This represented an 8% increase on the number of unique females and males prescribed antidepressants in March 2019, and a 21% increase on the number seen in March 2016.
Two further peaks of 17,311 and 17,088 antidepressant prescriptions for female patients were seen around the time of the second and third lockdowns, in December 2020 and January 2021, respectively.
“These periods correspond approximately to the first, second and third lockdown periods and the reasons are wide-ranging, depending on your focus,” said Beryl Navti, an advanced mental health pharmacist at North East London NHS Foundation Trust.
“Antidepressants are prescribed for both depression and anxiety disorders, and if we are saying that levels of anxiety increased amongst some young people during these periods, it makes sense that there would have been a corresponding increase in prescribed medication.
“In patients already diagnosed with anxiety disorders or depression and prescribed medication, there could have been increase in demand for repeat prescriptions every time a lockdown was announced, and as community pharmacies remained open, it stands to reason that prescribing costs would reflect these spikes in demand.”
Graham Brown, lead children’s and younger people’s mental health pharmacist at Sussex Partnership NHS Foundation Trust, found a similar pattern in antidepressant prescribing in data collated in his area during the pandemic.
According to his analysis, the Sussex Children and Adolescent Mental Health Service (CAMHS) issued 22% more antidepressant prescriptions between March 2020 and March 2021 than it did between March 2019 and February 2020.
Hampshire CAMHS issued 32% more antidepressant prescriptions between March 2020 and March 2021, compared with the same period the previous year.
“Certainly within Worthing CAMHS, where I am clinically based, there has been an increase in pressure to prescribe antidepressants, partly due to seeing more patients with such concerns, but also there being insufficient resourcing of psychological therapy in this geographical area,” he explains.
Martin Marshall, chair of the Royal College of GPs, said that antidepressants were often “an effective treatment” to help patients manage mental illness, but that any decision to prescribe must take into account the individual circumstances of the patient and the benefits and risks of the treatment in comparison to alternative treatments, such as cognitive behavioural therapy.
“However, access to appropriate, alternative therapies in the community, that many younger patients with mental health conditions find beneficial, is patchy across the country,” he said.
“This needs to be addressed urgently to ensure younger patients can access these treatments quickly, particularly in view of the increased demand for these services due to the pandemic.”
Nick Harrop, head of external affairs at the children and young person’s mental health charity YoungMinds, said that many young people the charity worked with had struggled to cope with the changes brought on by the pandemic, with some experiencing social isolation, anxiety, disruption to education or fears about their future — particularly during the lockdowns.
“We know that some young people have dealt with multiple pressures, especially those who have been bereaved or experienced other trauma during this time. Young people who are already experiencing inequalities have often been disproportionately affected.
He added that, while antidepressants can play a role in supporting some young people’s mental health, it was “crucial” that they are never seen as a substitute for fast access to talking therapies.
“Research we have carried out with GPs shows that many lack confidence in referrals they make to CAMHS because of long waiting times and high thresholds for treatment. That’s why it’s crucial that we see extra investment in specialist mental health services, but also in early support for young people, so that they have somewhere to turn when problems first emerge.
“As we emerge from the pandemic, the government should invest in a national network of early support hubs across the country, so that any young person who needs help can get it as soon as they start to struggle.”


