Abstract
Non-ST-elevation acute coronary syndrome (NSTE-ACS) encompasses NSTE-myocardial infarction (NSTEMI) and unstable angina (UA). In the UK, the annual incidence of hospital admissions relating to NSTE-ACS is around 50,000. However, owing to the difficulty in diagnosing NSTE-ACS, it is hard to establish its true prevalence. There is emerging evidence that the long-term mortality of NSTEMI is equivalent to, or potentially higher than, that of STEMI.
The intensity of treatment and intervention in patients with NSTE-ACS is ultimately guided by risk of future adverse cardiovascular events. This article provides an overview of the pharmacotherapy of NSTE-ACS, with reference to recommendations from clinical guidelines from the United States, UK, Europe and Australia and New Zealand.
Keywords: guidelines; non-ST-elevation acute coronary syndrome; NSTEMI.
Original submitted: 18 July 2019; Revised submitted: 8 July 2021; Accepted for publication: 21 July 2021.
Key points
- The use of validated risk scoring systems to establish the future risk of adverse cardiovascular and bleeding events is recommended to inform risk/benefit decisions regarding treatment/intervention for NSTE-ACS patients;
- Coronary angiography and subsequent revascularisation is dependent on the ischaemic risks of the patient;
- Pharmacotherapy is guided by phase of treatment in relation to management strategy (i.e. pre-treatment, peri-procedural and post-treatment phase);
- All patients with NSTE-ACS should be offered treatment with dual antiplatelets. The duration of dual antiplatelet therapy is dependent on the relative thrombotic and bleeding risks of the patient;
- Other drugs used in the management of NSTE-ACS are statins, angiotensin-converting enzyme inhibitors inhibitors, beta-blockers, aldosterone antagonists and anticoagulants;
- Variations exist between the guidelines in relation to the following areas:
- Timing of administration of P2Y12 inhibitors in relation to coronary angiography;
- Choice of anticoagulants and P2Y12 inhibitors during the acute phase of NSTE-ACS;
- Duration of dual antiplatelet therapy;
- Duration of beta-blocker therapy.
- The main reason for the variation between guidelines is owing to the availability of more recent evidence, which affects the more recent guidelines (National Institute for Health and Care Excellence and European Society of Cardiology).
Introduction
The clinical presentations of unstable angina (UA) and non-ST-elevation myocardial infarction (NSTEMI) can be identical and they have recently been grouped together by the term non-ST-elevation acute coronary syndrome (NSTE-ACS)[1]. Patients presenting with NSTE-ACS on electrocardiogram (ECG) are classified as having UA or NSTEMI depending on the absence or presence of biochemical markers of myocardial necrosis, respectively[2].
UA is defined as myocardial ischaemia at rest or minimal exertion in the absence of cardiomyocyte necrosis[1]. NSTEMI is where cardiomyocyte necrosis exists[1]. Compared with patients with NSTEMI, individuals with UA have a substantially lower risk of death and appear to derive less benefit from intensified antiplatelet therapy as well as early invasive treatment[3]. Symptomatically, UA is differentiated from stable angina by specific clinical findings of prolonged angina at rest (>20 minutes); new onset of severe angina; angina that is increasing in frequency, longer in duration or lower in threshold; or angina that occurs after a recent episode of myocardial infarction (MI)[3].
NSTE-ACS is caused by a partially occluded coronary artery, as opposed to the complete occlusion found in STEMI, usually as the result of the formation of a non-occlusive thrombus, which often develop within a disrupted atherosclerotic plaque[4]. Other possible causes of NSTE-ACS are Prinzmetal’s angina, re-stenosis following percutaneous coronary intervention, recreational drug use or focal coronary artery spasm[1].
The clinical presentations of NSTE-ACS vary widely: some patients are asymptomatic at presentation, while others may experience ongoing ischaemia, haemodynamic instability or cardiac arrest[2].
This article discusses the pharmacotherapy of NSTE-ACS, from symptom onset to secondary prevention. The recommendations from four important clinical guidelines will be referred to and summarised:
- The American College of Cardiology (ACC)/American Heart Association (AHA) guideline[1];
- The National Institute for Health and Care Excellence (NICE) guideline[5];
- The National Heart Foundation of Australia & Cardiac Society of Australia and New Zealand (ANZ) guideline[6];
- European Society of Cardiology (ESC) guideline[3];
This article aims to provide readers with an international perspective on the management of NSTE-ACS, however the focus will be on UK-based management. An international perspective can provide an objective assessment of the key similarities and differences in the management of NSTE-ACS and highlight any gaps in evidence which may need to be addressed.
Epidemiology
The diagnosis of NSTEMI is more difficult to establish than STEMI and therefore its prevalence is harder to estimate. The difference between STEMI and NSTE-ACS is highlighted with an ECG, with STEMI having persistent (>20 minutes) ST-segment elevation; while NSTE-ACS may still present with ECG changes, but not in the form of persistent ST-segment elevation[3]. These changes may include transient ST-segment elevation, ST-segment depression and T-wave inversions[3].
The annual incidence of hospital admissions for ACS in the UK is more than 80,000, of which NSTE-ACS accounts for two-thirds[7]. The introduction of highly sensitive cardiac troponin (hs-cTn) measurements in place of standard troponin assays have resulted in an increase in the detection of NSTEMI, among those presenting with suspected NSTE-ACS, and a reciprocal decrease in the diagnosis of UA[8]. Epidemiological data show that the incidence for NSTEMI is rising compared with STEMI[9]. Data for 2017/2018 from the Myocardial Ischaemia National Audit Project (MINAP) show that there were 92,233 admissions to NHS hospitals in the UK with an acute MI; 39% were STEMI, and 61% were NSTEMI[10]. The rise in incidence of NSTEMI was largely owing to the refinement in operational diagnosis and the changes in patient characteristics, including the increased prevalence of diabetes, hypertension and obesity[11].
Prognosis
Patients who experience a MI will most likely experience other cardiovascular-related events in the future[12]. Prognosis depends on the timing and nature of intervention[13]. NSTEMI patients appear to have lower 30-day mortality rate compared with STEMI patients, while at one- or two-years follow-up the mortality rates become comparable[14,15].
Early revascularisation, as well as the use of antithrombotic agents and beta-blockers, have markedly reduced the incidence of life-threatening arrhythmias in the acute phase of NSTE-ACS to <3%[3,16]. The acute phase of NSTE-ACS includes the time from diagnosis to angiography to stent insertion. The acute phase is also referred to as pre- and peri-procedural periods in this article. Most arrhythmic events occur within 12 hours of NSTE-ACS symptom onset[16]. Patients with life-threatening arrhythmias are more likely to have prior heart failure, have left ventricular ejection fraction (LVEF) at <30%, and have multi-vessel coronary artery disease (CAD)[16]. Patients with a high ischaemic risk are at greater risk of a major adverse cardiac event than patients with a lower ischaemic risk[3]. Risk is highest at the time of presentation but remains elevated past the acute phase[3]. By six months, NSTE-ACS mortality rates may equal or exceed those of STEMI[17]. By 12 months, rates of death, MI and recurrent instability in large-scale patient registries are >10%[3]. While early events are related to ruptured coronary plaques and associated thrombosis, the majority of later events may be the result of coronary and systemic atherosclerosis progression[18].
In contrast to the treatment pathway for STEMI, which is based largely around evidence-based emergency provision of reperfusion therapy, the treatment pathway for NSTE-ACS is more diverse and dependent on local resource availability, such as staff and access to cardiac catheter laboratories[5,19]. In addition, NSTE-ACS patients tend to be older in age and have more co-morbidities (e.g. hypertension, diabetes, heart failure), therefore having a wider range of clinical risks, making them more challenging to diagnose and treat[19,20]. The intensity of treatment is ultimately guided by risk and therefore directly relates to the prognosis of the individual.
Risk stratification
All guidelines recommend that as soon as a diagnosis of NSTE-ACS is suspected and/or confirmed, patients should be formally assessed to establish their future risk of adverse cardiovascular and bleeding events using validated risk scoring systems[1,3,5,6]. Risk scores can inform risk/benefit decisions regarding treatment[1,3,5,6]. In NSTE-ACS, quantitative assessment of ischaemic risk by means of scores is superior to clinical assessment alone[3]. Examples of risk scoring systems that are validated in large populations and used internationally are:
- Thrombolysis in myocardial infarction (TIMI) risk score[21];
- Global registry of acute coronary events (GRACE) score[22];
- Platelet glycoprotein IIb/IIIa in unstable angina: receptor suppression using integrilin (eptifibatide) therapy (PURSUIT) score[23].
NICE, ESC and ANZ guidelines all advocate for the use of the GRACE tool to identify patients who will benefit from an invasive treatment strategy, however the US guideline is less prescriptive, with either TIMI or GRACE being recommended[1,3,5,6].
The GRACE scoring system was derived from a large registry of ACS patients (n=11,389) to predict in-hospital mortality at six months, one year and three years[22]. Prediction risk scores are based on variables such as age, heart rate, systolic blood pressure, creatinine levels, Killip classification of heart failure, ST-segment deviation, elevated cTn and the occurrence of cardiac arrest on admission[22].
Bleeding risk assessment
Major bleeding events are associated with increased mortality in people with NSTE-ACS[24]. Bleeding risk scores used in clinical practice include:
- Can rapid risk stratification of unstable angina patients suppress adverse outcomes with early implementation of the ACC/AHA guidelines (CRUSADE) bleeding risk score[25];
- Acute catheterisation and urgent intervention triage strategy (ACUITY) bleeding risk score[24].
Overall, both the CRUSADE and ACUITY scores have reasonable and comparable predictive value for major bleeding in ACS patients undergoing coronary angiography[26–28]. The predictive values of both scores have not been established in patients who are not undergoing coronary angiography or in those who are taking oral anticoagulants.
Acute pharmacotherapy management in suspected NSTE-ACS
General supportive measures, such as the initiation of nitrates and beta-blockers, should be provided when emergency services arrive (and before ACS is confirmed), with the goal to decrease myocardial oxygen demand or increase myocardial oxygen supply[1,3,6]. Oxygen should only be administrated in patients with NSTE-ACS if oxygen saturation is <90% or if the patient is in respiratory distress, as some evidence suggests that routine use of supplemental oxygen in cardiac patients may have untoward effects, such as increased coronary vascular resistance and increased mortality risk[1,29].
For patients who are unresponsive to nitrates and beta-blockers or where contraindications are present, opiate administration is reasonable, with the caveat that morphine may slow intestinal absorption of oral antiplatelets (i.e. P2Y12 inhibitors)[30]. Non-steroidal anti-inflammatory drugs (NSAIDs, except aspirin) should not be initiated for analgesia during the acute phase, and any ongoing treatment with NSAIDs should be discontinued during hospitalisation owing to the increased risk of major adverse cardiovascular events (MACE) associated with their use[31].
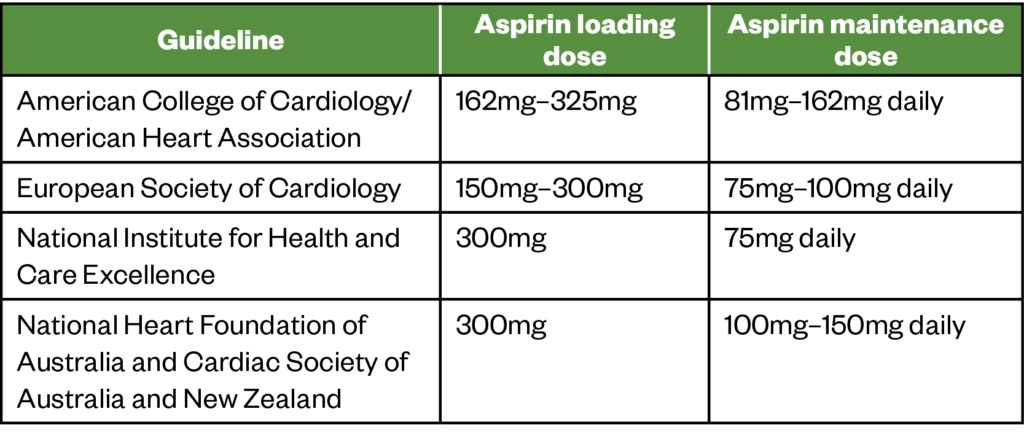
Once general supportive measures are provided, platelet inhibition should be initiated. A single loading dose of aspirin is normally recommended as soon as possible to all patients upon presentation of NSTE-ACS (unless contraindications exist)[1,3,5,6]. Following this, a maintenance dose of aspirin should be continued indefinitely. Four randomised controlled trials have demonstrated the benefit of aspirin in patients with UA by reducing the incidence of MI or death[32]. Loading and maintenance dose recommendations differ between guidelines, as outlined in Table 1 below.
Pharmacotherapy management of confirmed NSTE-ACS in the pre-treatment and peri-procedural phase
While percutaneous coronary intervention (PCI) is the mainstream intervention in patients with STEMI, the mainstream intervention/procedure for patients with NSTE-ACS is invasive coronary angiography with coronary revascularisation (PCI or coronary artery bypass graft [CABG]), as appropriate[1,3,5,6]. Invasive coronary angiography allows clinicians to:
- Confirm the diagnosis of ACS related to obstructive epicardial CAD (or to rule out a coronary origin of chest pain) and, as a consequence, to guide antithrombotic treatment and avoid unnecessary exposure to antithrombotic agents;
- Identify culprit lesion(s);
- Establish the indication for coronary revascularisation and assess the suitability of coronary anatomy for PCI and CABG;
- Stratify the patient’s short- and long-term risk[3].
In patients considered at low risk of ischaemic events, a conservative management strategy is recommended, which consists of a non-invasive stress test (e.g. exercise tolerance test) before deciding on an invasive strategy[3,5].
The pharmacological management of patients in the acute phase is divided into treatment during the pre-treatment phase and the peri-procedural phase.
Antiplatelet use during pre-treatment
The use of P2Y12 inhibitors (e.g. clopidogrel, prasugrel or ticagrelor) soon after the diagnosis of NSTE-ACS, irrespective of management strategy, is referred to as pre-treatment, defined as P2Y12 inhibitor administration before coronary angiography, and when coronary anatomy is unknown[33]. To date, this practice is not yet supported by large-scale randomised controlled trials[3,5]. Fortunately, the recommended standard treatment with potent P2Y12 receptor inhibitors (e.g. ticagrelor or prasugrel) exhibits a fast onset of action, thereby allowing a loading dose to be administered after diagnostic coronary angiography and directly before PCI[3]. The use of P2Y12 inhibitors is discussed in subsequent sections of this article.
Anticoagulants
Anticoagulation therapy should be offered in addition to antiplatelet therapy in the peri-interventional phase[1,3,5,6]. There is evidence that anticoagulation is effective in reducing ischaemic events in NSTE-ACS and, when combined with antiplatelets, it has been shown to be more effective than either treatment alone[34].
The preferred anticoagulant differs between the guidelines. Fondaparinux is recommended by NICE in the pre-treatment phase (i.e. before coronary angiography) for NSTE-ACS patients who do not have a high bleeding risk and who are not undergoing immediate angiography[5].
The recommendation made by NICE for fondaparinux as a pre-treatment anticoagulant was based largely on evidence from the OASIS-5 trial[5,35]. The OASIS-5 trial treated patients with fondaparinux during the conservative treatment phase, who may subsequently undergo cardiac catheterisation[35]. The trial showed reduced major bleeding and mortality, and non-inferiority in the reduction of ischaemic events compared with enoxaparin/unfractionated heparin (UFH)[35].
For patients undergoing PCI, the peri-interventional anticoagulant recommendations are: enoxaparin by the US guideline, or UFH by the European and NICE guidelines[1,3,5]. The ANZ guideline does not favour either UFH or enoxaparin over the other[6]. ESC recommends that fondaparinux is given with a single bolus of UFH for cases of medical treatment or logistical constraints for transferring the patient to PCI within the required time frame[3]. Bivalirudin is recommended as a second-line treatment, as an alternative to either UFH or enoxaparin for individuals at increased risk of bleeding events[1,3,6].
A meta-analysis of trials investigating enoxaparin versus UFH in ACS showed a marginally significant reduction in the combined endpoint of death or MI at 30 days in favour of enoxaparin, but no significant differences in major bleeds at 7 days. However, this meta-analysis did not include a dedicated large-scale randomised study in NSTE-ACS[36].
The recommendation to use UFH over bivalirudin was based largely on the VALIDATE-SWEDEHEART trial, conducted in a contemporary setting of preferred radial access and selective use of GP IIb/IIIa inhibitors[37]. The trial confirmed that bivalirudin compared with heparin was associated with a similar incidence of all-cause death and ischaemic events after PCI[37]. The ACUITY trial, which compared bivalirudin with UFH or low molecular weight heparin (LMWH), found no significant differences for the composite ischaemia endpoint at 30 days or for major bleeds[38]. However, bivalirudin was shown in a meta-analysis to be associated with a significant increased risk of stent thrombosis and MI[39]. For this reason, the use of bivalirudin is reserved as an alternative to UFH plus glycoprotein (GP) IIb/IIIa inhibitors during PCI[1,3,6].
GP IIb/IIIa inhibitors such as tirofiban, eptifibatide or abciximab are limited to peri-procedural use during PCI for NSTE-ACS patients[3,6]. Administered intravenously, GP IIb/IIIa inhibitors have an immediate effect, thereby providing an immediate reduction in the risk of ischemic events during PCI[40]. However, concerns over high bleeding risk and cost have led to a steady decline in their use[40]. European, UK and US guidelines recommend that GP IIb/IIIa inhibitors be limited to bailout use (i.e. for thrombotic procedural complications such as slow flow, no reflow, or angiographic evidence of a large thrombus)[1,3,5]. The majority of trials evaluating GP IIb/IIIa inhibitors in PCI-treated ACS patients predate the era of routine DAPT[41]. Therefore, in the current landscape of use of potent platelet inhibition with ticagrelor or prasugrel, where randomised data on GP IIb/IIIa use are limited, routine use of these agents cannot be recommended. Parenteral anticoagulation should be discontinued after PCI, unless otherwise indicated (e.g. the confirmed presence of LV aneurysm with thrombus formation)[1,3,5,6]. Anticoagulation can be continued in patients not undergoing angiography, for a maximum of eight days or until hospital discharge, whichever occurs first[42].
Beta-blockers
Beta-blocker treatment should be initiated in the acute phase of NSTE-ACS with help with ongoing ischaemic symptoms, unless contraindicated[1,3,5,6]. The evidence for the beneficial effects of beta-blockers in NSTE-ACS is derived from a meta-analysis of 27 studies showing that treatment was associated with a 13% relative risk reduction of mortality in the first week following MI[43].
The continuation of beta-blockers after discharge from hospital as part of a secondary prevention regime is discussed in the next section.
Secondary prevention in non-ST-elevation acute coronary syndrome
Long-term pharmacotherapy in NSTE-ACS patients, also known as secondary prevention treatment, is aimed at modifying risks of further CV events. These pharmacotherapies, coupled with important lifestyle changes, are of paramount importance because of the high risk for recurrent ischaemic events after an NSTE-ACS episode. The pharmacotherapy for secondary prevention in both STEMI and NSTE-ACS are similar; detail relating to this can be found in ‘Pharmacotherapy of STEMI: a review of international guidelines‘.
P2Y12 inhibitors
Patients with NSTE-ACS should be treated with dual antiplatelet therapy (DAPT)[1,3,5,6]. A P2Y12 inhibitor is recommended, in addition to aspirin, for 12 months unless there are contraindications, such as excessive bleed risk[1,3,5,6]. Available P2Y12 inhibitors include clopidogrel, prasugrel, ticagrelor and cangrelor.
The choice of P2Y12 inhibitor in NSTE-ACS patients is dependent on the risk of future adverse cardiovascular events and the corresponding reperfusion strategy chosen. The European guideline specifies the preference for prasugrel in patients who are undergoing PCI[3]. This recommendation was based on the ISAR-REACT 5 trial, which showed that a prasugrel-based strategy was superior to a ticagrelor-based strategy in the reduction of composite rate of death, MI or stroke (6.9 vs. 9.3%, P=0.006) without any increase in bleeding complications (4.8 vs. 5.4%, P=0.46)[44].
NICE also considered the evidence provided by the ISAR-REACT 5 trial[5]. Prasugrel should not be used before knowing the coronary anatomy in NSTE-ACS patients owing to the higher bleeding risk[45]. As the time to coronary angiograph in the UK is up to 72 hours, this may preclude the use of prasugrel owing to the unknown coronary anatomy. Thus, NICE does not favour prasugrel and recommends ticagrelor and prasugrel equally for this group of patients[5].
The American and ANZ guidelines were released before the ISAR REACT 5 trial and are not as specific, but instead recommended the use of ticagrelor or prasugrel over clopidogrel[1,6]. Ticagrelor and clopidogrel are indicated for all reperfusion strategies (i.e. PCI or angiography-guided revascularisation)[46].
Ticagrelor has a faster and more consistent onset of action compared with clopidogrel, in addition to a quicker offset of action with more rapid recovery of platelet function[47]. Ticagrelor was found to be more effective than clopidogrel in patients with moderate to high-risk NSTE-ACS in the PLATO trial[46].
Prasugrel is a prodrug, and acts by irreversibly binding its active metabolite onto platelet P2Y12 receptors and inhibiting their action. It has a faster onset and a more potent antiplatelet effect than clopidogrel[48]. The TRITON-TIMI 38 trial demonstrated that patients receiving prasugrel had fewer recurrent CV events and less stent thrombosis, but more bleeding complications, compared with clopidogrel[49]. Therefore, prasugrel should be considered in patients who present with stent thrombosis, despite compliance with clopidogrel therapy[50]. Prasugrel is contraindicated in patients with prior stroke/transient ischaemic attack; the TRITON-TIMI 38 trial showed there was an increased risk of major and fatal bleeding in this group[49]. Moreover, the study showed no apparent benefit for the use of prasugrel over clopidogrel in patients aged above 75 years or with low bodyweight (<60kg)[49].
Clopidogrel is used in combination with aspirin at a maintenance dose of 75mg daily in patients with NSTE-ACS. Generally, clopidogrel is used when ticagrelor or prasugrel are not suitable; for example, in those with an indication for oral anticoagulation and in those with prior intracranial bleeding[1,3,5,6]. Clopidogrel is an inactive prodrug that requires oxidation by the hepatic enzyme CYP450 to generate an active metabolite[51]. Around 85% of the prodrug is hydrolysed by esterase enzymes into an inactive form, leaving only 15% of clopidogrel available for transformation to the active metabolite, which inactivates platelet P2Y12 receptors and thus inhibits platelet aggregation[51]. For this reason, pharmacodynamic and pharmacokinetic studies have described substantial inter-individual variability in the antiplatelet response to clopidogrel, resulting in an increased risk of ischaemic and bleeding events in clopidogrel hypo- and hyper-responders, respectively[52,53]. DAPT comprising aspirin and clopidogrel has been shown to reduce recurrent ischaemic events in the NSTE-ACS setting compared with aspirin alone[54].
Prasugrel and ticagrelor are more potent antiplatelets in comparison with clopidogrel and have shown increased risk of major bleeding compared with clopidogrel[48,55]. Therefore, for patients with a high risk of bleeding, clopidogrel may be a more appropriate option. In addition, clopidogrel may be useful for those who require long-term oral anticoagulation as most trials involving the use of dual antiplatelet in conjunction with anticoagulant (i.e. triple therapy) were based on the use of clopidogrel[56,57]. ESC, NICE and ANZ guidelines state that the use of prasugrel or ticagrelor as part of triple therapy should be avoided[3,5,6]. The use of triple therapy in patients requiring long-term oral anticoagulants will not be covered within this article, as it was not featured equally in all four guidelines and the evidence around the optimal duration of triple therapy is still evolving[3,5,6].
Duration of dual antiplatelet therapy
Consisting of a P2Y12 inhibitor and aspirin, DAPT is generally recommended for 12 months in patients with NSTE-ACS[1,3,5,6]. However, in specific clinical scenarios, DAPT duration can be shortened (<12 months) or extended (>12 months), depending on the presenting ischaemic and bleeding risk, the occurrence of adverse events and comorbidities[3,6]. Patients identified as having a higher risk of bleeding (e.g. those with previous bleeding complications, low platelet count, or concurrent use of anticoagulants) should be assessed and considered for a shorter duration of dual antiplatelet therapy (i.e. <12 months). The US guideline outlined a shortened duration of <12 months but does not mention an exact duration[1]. Shortened DAPT duration is not covered in the NICE guideline[5]. ESC and ANZ guidelines recommend that DAPT duration may be shortened to 3–6 months, balancing the ischaemic and bleeding risks[3,6,58–60].
Extended dual antiplatelet therapy
The extended use of DAPT (beyond 12 months) may be considered in patients with moderate-high ischaemic risk without increased risk of major bleeds[3,6]. The definitions of high ischaemic risks and low bleeding risks are outlined in the ESC guidance[3]. The US guideline recommends DAPT therapy for at least 12 months for patients who received PCI, depending on stent type[1]. Extended DAPT is recommended with either clopidogrel, ticagrelor or prasugrel[3,6]. The European guideline has a separate DAPT-focused update, which recommends the use of ticagrelor over clopidogrel/prasugrel for extended DAPT therapy[61]. This recommendation is based on a meta-analysis on the effect of extended DAPT in patients with previous MI, which evaluated all three P2Y12 inhibitors[62]. While the results of the meta-analysis may suggest a consistent class effect among clopidogrel, ticagrelor or prasugrel in the decreased risk of MACE, cardiovascular death and stroke, the PEGASUS study — which only evaluated ticagrelor — contributed ≥60% to pooled endpoint estimates within this meta-analysis and was the only trial included in its totality (and as such the only properly powered study for post-MI patients); ESC therefore recommends the use of ticagrelor as first-line treatment[3,63]. This showed that ticagrelor at doses of 60mg twice daily (in conjunction with aspirin 75–150mg once daily and compared with aspirin monotherapy) reduces the risk of ischaemic events in patients who have already reached the first anniversary of their heart attack. The recommendation for treatment duration for the use of ticagrelor (in addition to aspirin), ranges from a period of up to three years to no upper limit[3,6]. However, ESC does suggest the use of extended DAPT with clopidogrel and prasugrel as well, where patients are not eligible for ticagrelor use.
The authors of the PEGASUS-TIMI 54 trial found that for 1,000 patients initiated on ticagrelor 60mg twice daily for 3 years, 13 primary end-point events would be prevented, including 5 ischemic strokes[63]. This benefit would come at a cost of nine TIMI major bleeds, but no hemorrhagic strokes or fatal bleeds[63]. The benefits and risks of extended DAPT must therefore be considered carefully on a case-by-case basis.
Another treatment strategy for extended therapy is the use of dual antithrombotic therapy (DAT), consisting of factor-Xa inhibition with a very low dose of rivaroxaban (2.5mg twice daily) plus aspirin. This regimen was recommended as an option for maintenance treatment beyond 12 months post ACS PCI by ESC[3]. More details can be found under ‘Secondary prevention‘.
A proton-pump inhibitor (PPI) is recommended to be taken in combination with DAPT in patients with higher risk of gastrointestinal bleeds. It is important to note the interaction between certain PPIs (e.g. omeprazole and esomeprazole) which undergo CYP450 metabolism and hence reduce plasma levels of clopidogrel[64]. The FDA, MHRA and EMA currently advise avoiding omeprazole and esomeprazole in patients taking clopidogrel[65–67].
Lipid modification therapy
Statins inhibit the rate-limiting step in cholesterol synthesis and may also reduce vascular inflammation, improve endothelial function and decrease thrombus formation, in addition to lowering LDL[68]. All four guidelines recommend initiation of high-intensity statin therapy as early as possible following admission in all NSTE-ACS patients (in the absence of contraindications)[1,3,5,6]. The evidence for the use of a high-intensity statin was supported by a meta-analysis of eight studies involving 13,208 patients with ACS, which found that the initiation of statin therapy before or after PCI led to 35 fewer MACE at 12 months per 1,000 treated[69]. High-dose statins versus no- or low-dose statins reduced the combined endpoint of death, recurrent MI and stroke (OR 0.52, 95% CI 0.37-0.73). There was non-significant reduction in MI (OR 0.81, 95% CI 0.65-1.01; P=0.06).
The preferred statin is atorvastatin at 80mg daily, unless patient preference, interacting drugs or high risk of adverse effects warrant a dose reduction[1,5]. This was based on the PROVE IT-TIMI 22 and MIRACL trials, which showed a lowering of low-density lipoprotein cholesterol (LDL-C) levels by ≥50%[70,71]. ESC and ANZ guidelines do not specify the preferred high-intensity statin but do have a ‘treat to target’ approach[3,6]. The treatment target are as follows:
- To lower LDL-C to <1.4 mmol/L and to reduce it by at least 50% if the baseline LDL-C level is 1.8–3.5 mmol/L[3];
- A target LDL-C of 1.8 mmol/L[6].
The addition of ezetimibe is recommended if the LDL-C is not sufficiently lowered on statin therapy alone[3,5,6]. The IMPROVE-IT trial demonstrated a modest benefit for ezetimibe used in combination with a statin[72].
Proprotein convertase subtilisin kexin 9 (PCSK9) inhibitors (e.g. evolocumab and alirocumab) are recommended by NICE and ESC in patient cohorts where cholesterol is insufficiently managed on statin and ezetimibe therapy[3,5]. PCSK9 inhibitors have been shown to be effective at reducing cholesterol and LDL-C to <1.3mmol/L[73].
Beta-blockers
The current recommendation from ESC, NICE, ANZ and ACC guidelines is that beta-blockers should be used, in the absence of contraindications, in patients with reduced left ventricular systolic dysfunction (LVSD) (i.e. LVEF ≤40%) or heart failure (HF)[1,3,5,6]. The US guideline recommends using a beta-blocker with evidence of mortality reduction in patients with HF, such as sustained-release metoprolol succinate, carvedilol or bisoprolol[2]. Sustained-release metoprolol succinate is not licensed in the UK market. Beta-blockers have been associated with a significant reduction in mortality and/or cardiovascular events in this cohort of patients[74,75].
The evidence for the use of beta-blockers in patients without reduced LVSD or HF is limited[76]. The benefit of long-term (>1 year) beta-blocker therapy in patients with prior MI is also a subject of debate in recent years[76,77]. Recommendations regarding beta-blocker use in this group of patients therefore differs between guidelines. The US guideline recommends that it is ‘reasonable’ to continue beta-blocker therapy in patients with normal LV function with NSTE-ACS; while ANZ and NICE recommends discontinuation of beta-blockers after 12 months’ therapy in this group of patients[1,5,6]. ESC does not provide specific recommendations around this topic[3].
The need for, and duration of, beta-blocker therapy following MI to maintain a protective effect on cardiac events in the absence of LVSD are unknown and are currently being investigated in several randomised controlled trials[78].
Angiotensin-converting enzyme inhibitors
Angiotensin-converting enzyme (ACE) inhibitors are recommended by all guidelines in patients with reduced ventricular systolic dysfunction, heart failure, hypertension or diabetes[1,3,5,6]. Agents with proven efficacy should be used, such as enalapril and ramipril[79].
In patients without impaired LV function, the use of ACE inhibitors was not shown to reduce all-cause mortality, cardiovascular mortality, non-fatal MI, stroke and heart failure by some trials[80]. A meta-analysis, including 24 trials and 61,961 patients, documented that, in patients with coronary syndrome without heart failure, ACE inhibitors reduced cardiovascular events and death when compared with placebo but not when compared with active controls[81]. Therefore, the use of ACE inhibitors in patients with coronary syndromes without heart failure or high cardiovascular risk is not generally recommended by ESC, unless required to meet blood pressure targets[3]. ANZ, ACC and NICE recommend that ACE inhibitors should be initiated and continued indefinitely in all patients presenting with MI[1,5,6]. ACE inhibitors are thought to have a role in the prevention of cardiac remodelling, which refers to changes in size, shape, structure and function of the heart, often occurring after injury to the heart muscles[82].
In patients who cannot tolerate ACE inhibitors, an angiotensin receptor blocker (e.g. losartan) should be used[1,3,5,6].
Aldosterone antagonist
In patients displaying signs and/or symptoms of heart failure and reduced left ventricular ejection fraction post NSTE-ACS, an aldosterone antagonist should be initiated 3–14 days post-MI in patients with no existing contraindications[1,3,5]. The preferred aldosterone antagonist is eplerenone and is recommended in patients with LV dysfunction (LVEF ≤40%), congestive heart failure or diabetes[83]. Eplerenone therapy has been shown to reduce morbidity and mortality in these patients after ACS[83].
Anticoagulants
Dual antithrombotic therapy consisting of aspirin and a low-dose anticoagulant is recommended as a treatment option for maintenance treatment beyond 12 months post ACS PCI[3,5,84]. The only low-dose anticoagulant currently approved for use for this indication is rivaroxaban 2.5mg twice daily[85]. In a secondary prevention setting, the COMPASS trial found that rivaroxaban 2.5mg twice a day plus aspirin 100mg daily reduced the risk of the combined ischaemic endpoint, overall mortality and cardiovascular mortality alone; while it increased risks of major bleeding complications without a significant increase in the risk of fatal, intracranial or critical organ bleeding event[85]. Greater absolute risk reductions were seen in high-risk patients and, therefore, this treatment most benefits those with high thrombotic risk[3,84].
Conclusion
The management of NSTE-ACS is a rapidly evolving field of practice and this review has highlighted several differences across the four guidelines in relation to a number of pharmacotherapy areas. This is largely because of the variation in the publication year of the guidelines: from 2014 for the US guideline, to 2016 for the ANZ guideline, and 2020 for the UK and European guidelines[1,3,5,6]. The developments in the management of NSTE-ACS in recent years have resulted in the variations in recommendations across the different guidelines.
Evidence remains lacking regarding the use of P2Y12 inhibitor before coronary angiography (i.e. in the pre-treatment phase)[33]. The evidence in this area of practice remains limited, and has been identified by the European guideline as an area for future research[3].
The next key difference between the guidelines was related to the choice of anticoagulant during the peri-interventional phase of NSTE-ACS.
Lastly, key differences exist in the guidelines involving the recommendations around pharmacotherapy for secondary prevention in two therapy areas: long-term antiplatelet therapy, and beta-blocker therapy. The evidence around the optimal duration of DAPT in this cohort of patients is still limited and has been identified as a gap in practice by ESC[3]. The benefits of the long-term use of beta-blockers in patients with normal LV function and no other indications for beta-blockers remain unknown. NICE and ANZ recommend limiting the use of beta-blockers in this cohort of patients to 12 months[5,6]. While beneficial effects of beta-blockers beyond 12 months are limited, discontinuation may be associated with some risks[5]. Further research is therefore recommended to establish the outcome of patients with NSTE-ACS who are using long-term beta-blockers, compared with those who have discontinued beta-blockers[3,5].
- 1Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes: Executive Summary. Circulation 2014;130:2354–94. doi:10.1161/cir.0000000000000133
- 2Sheridan PJ. Critical review of unstable angina and non-ST elevation myocardial infarction. Postgraduate Medical Journal 2002;78:717–26. doi:10.1136/pmj.78.926.717
- 3Collet J-P, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. European Heart Journal 2020;42:1289–367. doi:10.1093/eurheartj/ehaa575
- 4Rott D, Leibowitz D. STEMI and NSTEMI are two distinct pathophysiological entities. European Heart Journal 2007;28:2685–2685. doi:10.1093/eurheartj/ehm368
- 5NG185: Acute Coronary Syndromes. National Institute of Health and Care Excellence. 2020.https://www.nice.org.uk/guidance/ng185 (accessed Aug 2021).
- 6Chew DP, Scott IA, Cullen L, et al. National Heart Foundation of Australia and Cardiac Society of Australia and New Zealand: Australian clinical guidelines for the management of acute coronary syndromes 2016. Medical Journal of Australia 2016;205:128–33. doi:10.5694/mja16.00368
- 7Kotecha T, Rakhit RD. Acute coronary syndromes. Clin Med 2016;16:s43–8. doi:10.7861/clinmedicine.16-6-s43
- 8Shah ASV, Anand A, Strachan FE, et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: a stepped-wedge, cluster-randomised controlled trial. The Lancet 2018;392:919–28. doi:10.1016/s0140-6736(18)31923-8
- 9McManus DD, Gore J, Yarzebski J, et al. Recent Trends in the Incidence, Treatment, and Outcomes of Patients with STEMI and NSTEMI. The American Journal of Medicine 2011;124:40–7. doi:10.1016/j.amjmed.2010.07.023
- 10Myocardial Ischaemia National Audit Project: 2019 summary report (2017/18 data). NICOR. 2019.https://www.nicor.org.uk/wp-content/uploads/2019/09/MINAP-2019-Summary-Report-final.pdf (accessed Aug 2021).
- 11Puymirat E, Simon T, Cayla G, et al. Acute Myocardial Infarction. Circulation 2017;136:1908–19. doi:10.1161/circulationaha.117.030798
- 12Park H-W, Yoon C-H, Kang S-H, et al. Early- and late-term clinical outcome and their predictors in patients with ST-segment elevation myocardial infarction and non-ST-segment elevation myocardial infarction. International Journal of Cardiology 2013;169:254–61. doi:10.1016/j.ijcard.2013.08.132
- 13Myerson M, Coady S, Taylor H, et al. Declining Severity of Myocardial Infarction From 1987 to 2002. Circulation 2009;119:503–14. doi:10.1161/circulationaha.107.693879
- 14Terkelsen CJ, Lassen JF, Nørgaard BL, et al. Mortality rates in patients with ST-elevation vs. non-ST-elevation acute myocardial infarction: observations from an unselected cohort. European Heart Journal 2004;26:18–26. doi:10.1093/eurheartj/ehi002
- 15Marceau A, Samson J-M, Laflamme N, et al. SHORT AND LONG-TERM MORTALITY AFTER STEMI VERSUS NON-STEMI: A SYSTEMATIC REVIEW AND META-ANALYSIS. Journal of the American College of Cardiology 2013;61:E96. doi:10.1016/s0735-1097(13)60097-2
- 16Piccini JP, White JA, Mehta RH, et al. Sustained Ventricular Tachycardia and Ventricular Fibrillation Complicating Non–ST-Segment–Elevation Acute Coronary Syndromes. Circulation 2012;126:41–9. doi:10.1161/circulationaha.111.071860
- 17Savonitto S. Prognostic Value of the Admission Electrocardiogram in Acute Coronary Syndromes. JAMA 1999;281:707. doi:10.1001/jama.281.8.707
- 18Fox KA, Anderson Jr FA, et al. Time course of events in acute coronary syndromes: implications for clinical practice from the GRACE registry. Nat Rev Cardiol 2008;5:580–9. doi:10.1038/ncpcardio1302
- 19Corcoran D, Grant P, Berry C. Risk stratification in non-ST elevation acute coronary syndromes: Risk scores, biomarkers and clinical judgment. IJC Heart & Vasculature 2015;8:131–7. doi:10.1016/j.ijcha.2015.06.009
- 20Veerasamy M, Edwards R, Ford G, et al. Acute Coronary Syndrome Among Older Patients. Cardiology in Review 2015;23:26–32. doi:10.1097/crd.0000000000000016
- 21Antman EM, Cohen M, Bernink PJLM, et al. The TIMI Risk Score for Unstable Angina/Non–ST Elevation MI. JAMA 2000;284:835. doi:10.1001/jama.284.7.835
- 22Granger CB. Predictors of Hospital Mortality in the Global Registry of Acute Coronary Events. Arch Intern Med 2003;163:2345. doi:10.1001/archinte.163.19.2345
- 23Boersma E, Pieper KS, Steyerberg EW, et al. Predictors of Outcome in Patients With Acute Coronary Syndromes Without Persistent ST-Segment Elevation. Circulation 2000;101:2557–67. doi:10.1161/01.cir.101.22.2557
- 24Mehran R, Pocock SJ, Nikolsky E, et al. A Risk Score to Predict Bleeding in Patients With Acute Coronary Syndromes. Journal of the American College of Cardiology 2010;55:2556–66. doi:10.1016/j.jacc.2009.09.076
- 25Subherwal S, Bach RG, Chen AY, et al. Baseline Risk of Major Bleeding in Non–ST-Segment–Elevation Myocardial Infarction. Circulation 2009;119:1873–82. doi:10.1161/circulationaha.108.828541
- 26Abu-Assi E, Raposeiras-Roubin S, Lear P, et al. Comparing the predictive validity of three contemporary bleeding risk scores in acute coronary syndrome. European Heart Journal: Acute Cardiovascular Care 2012;1:222–31. doi:10.1177/2048872612453924
- 27Liu R, Lyu S, Zhao G, et al. Comparison of the performance of the CRUSADE, ACUITY-HORIZONS, and ACTION bleeding scores in ACS patients undergoing PCI: insights from a cohort of 4939 patients in China. J Geriatr Cardiol 2017;14:93–9. doi:10.11909/j.issn.1671-5411.2017.02.011
- 28Costa F, Tijssen JG, Ariotti S, et al. Incremental Value of the CRUSADE, ACUITY, and HAS‐BLED Risk Scores for the Prediction of Hemorrhagic Events After Coronary Stent Implantation in Patients Undergoing Long or Short Duration of Dual Antiplatelet Therapy. JAHA 2015;4. doi:10.1161/jaha.115.002524
- 29Cabello JB, Burls A, Emparanza JI, et al. Oxygen therapy for acute myocardial infarction. Cochrane Database of Systematic Reviews Published Online First: 19 December 2016. doi:10.1002/14651858.cd007160.pub4
- 30Kubica J, Kubica A, Jilma B, et al. Impact of morphine on antiplatelet effects of oral P2Y12 receptor inhibitors. International Journal of Cardiology 2016;215:201–8. doi:10.1016/j.ijcard.2016.04.077
- 31Schjerning Olsen A-M, Fosbøl EL, Lindhardsen J, et al. Duration of Treatment With Nonsteroidal Anti-Inflammatory Drugs and Impact on Risk of Death and Recurrent Myocardial Infarction in Patients With Prior Myocardial Infarction. Circulation 2011;123:2226–35. doi:10.1161/circulationaha.110.004671
- 32Théroux P, Ouimet H, McCans J, et al. Aspirin, Heparin, or Both to Treat Acute Unstable Angina. N Engl J Med 1988;319:1105–11. doi:10.1056/nejm198810273191701
- 33Sibbing D, Kastrati A, Berger PB. Pre-treatment with P2Y12inhibitors in ACS patients: who, when, why, and which agent? Eur Heart J 2015;37:1284–95. doi:10.1093/eurheartj/ehv717
- 34Eikelboom JW, Anand SS, Malmberg K, et al. Unfractionated heparin and low-molecular-weight heparin in acute coronary syndrome without ST elevation: a meta-analysis. The Lancet 2000;355:1936–42. doi:10.1016/s0140-6736(00)02324-2
- 35Mehta SR, Granger CB, Eikelboom JW, et al. Efficacy and Safety of Fondaparinux Versus Enoxaparin in Patients With Acute Coronary Syndromes Undergoing Percutaneous Coronary Intervention. Journal of the American College of Cardiology 2007;50:1742–51. doi:10.1016/j.jacc.2007.07.042
- 36Silvain J, Beygui F, Barthelemy O, et al. Efficacy and safety of enoxaparin versus unfractionated heparin during percutaneous coronary intervention: systematic review and meta-analysis. BMJ 2012;344:e553–e553. doi:10.1136/bmj.e553
- 37Nührenberg TG, Hochholzer W, Mashayekhi K, et al. Efficacy and safety of bivalirudin for percutaneous coronary intervention in acute coronary syndromes: a meta-analysis of randomized-controlled trials. Clin Res Cardiol 2018;107:807–15. doi:10.1007/s00392-018-1251-1
- 38Stone GW, McLaurin BT, Cox DA, et al. Bivalirudin for Patients with Acute Coronary Syndromes. N Engl J Med 2006;355:2203–16. doi:10.1056/nejmoa062437
- 39Zhang S, Gao W, Li H, et al. Efficacy and safety of bivalirudin versus heparin in patients undergoing percutaneous coronary intervention: A meta-analysis of randomized controlled trials. International Journal of Cardiology 2016;209:87–95. doi:10.1016/j.ijcard.2016.01.206
- 40Abtan J, Ducrocq G, Steg PhG, et al. Characteristics and outcomes of patients requiring bailout use of glycoprotein IIb/IIIa inhibitors for thrombotic complications of percutaneous coronary intervention: An analysis from the CHAMPION PHOENIX trial. International Journal of Cardiology 2019;278:217–22. doi:10.1016/j.ijcard.2018.11.114
- 41Neumann F-J, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. European Heart Journal 2018;40:87–165. doi:10.1093/eurheartj/ehy394
- 42Comparison of Fondaparinux and Enoxaparin in Acute Coronary Syndromes. N Engl J Med 2006;354:1464–76. doi:10.1056/nejmoa055443
- 43Yusuf S, Wittes J, Friedman L. Overview of results of randomized clinical trials in heart disease. I. Treatments following myocardial infarction. JAMA 1988;260:2088–93.https://www.ncbi.nlm.nih.gov/pubmed/2901501
- 44Schüpke S, Neumann F-J, Menichelli M, et al. Ticagrelor or Prasugrel in Patients with Acute Coronary Syndromes. N Engl J Med 2019;381:1524–34. doi:10.1056/nejmoa1908973
- 45Montalescot G, Bolognese L, Dudek D, et al. Pretreatment with Prasugrel in Non–ST-Segment Elevation Acute Coronary Syndromes. N Engl J Med 2013;369:999–1010. doi:10.1056/nejmoa1308075
- 46Wallentin L, James S, Storey RF, et al. Effect of CYP2C19 and ABCB1 single nucleotide polymorphisms on outcomes of treatment with ticagrelor versus clopidogrel for acute coronary syndromes: a genetic substudy of the PLATO trial. The Lancet 2010;376:1320–8. doi:10.1016/s0140-6736(10)61274-3
- 47Gurbel PA, Bliden KP, Butler K, et al. Randomized Double-Blind Assessment of the ONSET and OFFSET of the Antiplatelet Effects of Ticagrelor Versus Clopidogrel in Patients With Stable Coronary Artery Disease. Circulation 2009;120:2577–85. doi:10.1161/circulationaha.109.912550
- 48Wiviott SD, Braunwald E, McCabe CH, et al. Prasugrel versus Clopidogrel in Patients with Acute Coronary Syndromes. N Engl J Med 2007;357:2001–15. doi:10.1056/nejmoa0706482
- 49De Servi S, Goedicke J, Schirmer A, et al. Clinical outcomes for prasugrel versus clopidogrel in patients with unstable angina or non-ST-elevation myocardial infarction: an analysis from the TRITON-TIMI 38 trial. European Heart Journal: Acute Cardiovascular Care 2014;3:363–72. doi:10.1177/2048872614534078
- 50Wiviott SD, Braunwald E, McCabe CH, et al. Intensive oral antiplatelet therapy for reduction of ischaemic events including stent thrombosis in patients with acute coronary syndromes treated with percutaneous coronary intervention and stenting in the TRITON-TIMI 38 trial: a subanalysis of a randomised trial. The Lancet 2008;371:1353–63. doi:10.1016/s0140-6736(08)60422-5
- 51Savi P, Labouret C, Delesque N, et al. P2Y12, a New Platelet ADP Receptor, Target of Clopidogrel. Biochemical and Biophysical Research Communications 2001;283:379–83. doi:10.1006/bbrc.2001.4816
- 52Matetzky S, Shenkman B, Guetta V, et al. Clopidogrel Resistance Is Associated With Increased Risk of Recurrent Atherothrombotic Events in Patients With Acute Myocardial Infarction. Circulation 2004;109:3171–5. doi:10.1161/01.cir.0000130846.46168.03
- 53Simon T, Verstuyft C, Mary-Krause M, et al. Genetic Determinants of Response to Clopidogrel and Cardiovascular Events. N Engl J Med 2009;360:363–75. doi:10.1056/nejmoa0808227
- 54Effects of Clopidogrel in Addition to Aspirin in Patients with Acute Coronary Syndromes without ST-Segment Elevation. N Engl J Med 2001;345:494–502. doi:10.1056/nejmoa010746
- 55James SK, Roe MT, Cannon CP, et al. Ticagrelor versus clopidogrel in patients with acute coronary syndromes intended for non-invasive management: substudy from prospective randomised PLATelet inhibition and patient Outcomes (PLATO) trial. BMJ 2011;342:d3527–d3527. doi:10.1136/bmj.d3527
- 56Dewilde WJ, Oirbans T, Verheugt FW, et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: an open-label, randomised, controlled trial. The Lancet 2013;381:1107–15. doi:10.1016/s0140-6736(12)62177-1
- 57Gibson CM, Mehran R, Bode C, et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N Engl J Med 2016;375:2423–34. doi:10.1056/nejmoa1611594
- 58Navarese EP, Andreotti F, Schulze V, et al. Optimal duration of dual antiplatelet therapy after percutaneous coronary intervention with drug eluting stents: meta-analysis of randomised controlled trials. BMJ 2015;350:h1618–h1618. doi:10.1136/bmj.h1618
- 59Costa F, van Klaveren D, James S, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. The Lancet 2017;389:1025–34. doi:10.1016/s0140-6736(17)30397-5
- 60Palmerini T, Della Riva D, Benedetto U, et al. Three, six, or twelve months of dual antiplatelet therapy after DES implantation in patients with or without acute coronary syndromes: an individual patient data pairwise and network meta-analysis of six randomized trials and 11 473 patients. Eur Heart J 2017;:ehw627. doi:10.1093/eurheartj/ehw627
- 61Valgimigli M, Bueno H, Byrne RA, et al. 2017 ESC focused update on dual antiplatelet therapy in coronary artery disease developed in collaboration with EACTS. European Heart Journal 2017;39:213–60. doi:10.1093/eurheartj/ehx419
- 62Udell JA, Bonaca MP, Collet J-P, et al. Long-term dual antiplatelet therapy for secondary prevention of cardiovascular events in the subgroup of patients with previous myocardial infarction: a collaborative meta-analysis of randomized trials. Eur Heart J 2015;:ehv443. doi:10.1093/eurheartj/ehv443
- 63Bonaca MP, Bhatt DL, Steg PG, et al. Ischaemic risk and efficacy of ticagrelor in relation to time from P2Y12inhibitor withdrawal in patients with prior myocardial infarction: insights from PEGASUS-TIMI 54. Eur Heart J 2015;37:1133–42. doi:10.1093/eurheartj/ehv531
- 64Yasuda H, Yamada M, Sawada S, et al. Upper Gastrointestinal Bleeding in Patients Receiving Dual Antiplatelet Therapy after Coronary Stenting. Intern Med 2009;48:1725–30. doi:10.2169/internalmedicine.48.2031
- 65FDA reminder to avoid concomitant use of Plavix (clopidogrel) and omeprazole. Food and Drugs Administration. 2010.https://www.accessdata.fda.gov/drugsatfda_docs/label/2011/020839s055lbl.pdf (accessed Jul 2021).
- 66Clopidogrel and proton pump inhibitors: interaction-updated advice. Drug Safety Update 2010; 3:4. Medicines and Healthcare products Regulatory Agency. 2010.https://www.gov.uk/drug-safety-update/clopidogrel-and-proton-pump-inhibitors-interaction-updated-advice (accessed Jul 2021).
- 67Public statement: Interaction between clopidogrel and proton pump inhibitors. European Medicines Agency. 2009.https://www.ema.europa.eu/en/news/public-statement-possible-interaction-between-clopidogrel-proton-pump-inhibitors#:~:text=The%20European%20Medicines%20Agency%20is,myocardial%20infarction%20(heart%20attack) (accessed Jul 2021).
- 68Sposito AC, Chapman MJ. Statin Therapy in Acute Coronary Syndromes. ATVB 2002;22:1524–34. doi:10.1161/01.atv.0000032033.39301.6a
- 69Navarese EP, Kowalewski M, Andreotti F, et al. Meta-Analysis of Time-Related Benefits of Statin Therapy in Patients With Acute Coronary Syndrome Undergoing Percutaneous Coronary Intervention. The American Journal of Cardiology 2014;113:1753–64. doi:10.1016/j.amjcard.2014.02.034
- 70Schwartz GG. Effects of Atorvastatin on Early Recurrent Ischemic Events in Acute Coronary Syndromes<SUBTITLE>The MIRACL Study: A Randomized Controlled Trial</SUBTITLE>. JAMA 2001;285:1711. doi:10.1001/jama.285.13.1711
- 71Ray KK, Cannon CP, McCabe CH, et al. Early and Late Benefits of High-Dose Atorvastatin in Patients With Acute Coronary Syndromes. Journal of the American College of Cardiology 2005;46:1405–10. doi:10.1016/j.jacc.2005.03.077
- 72Cannon CP, Blazing MA, Giugliano RP, et al. Ezetimibe Added to Statin Therapy after Acute Coronary Syndromes. N Engl J Med 2015;372:2387–97. doi:10.1056/nejmoa1410489
- 73Ray KK, Colhoun HM, Szarek M, et al. Effects of alirocumab on cardiovascular and metabolic outcomes after acute coronary syndrome in patients with or without diabetes: a prespecified analysis of the ODYSSEY OUTCOMES randomised controlled trial. The Lancet Diabetes & Endocrinology 2019;7:618–28. doi:10.1016/s2213-8587(19)30158-5
- 74Andersson C, Shilane D, Go AS, et al. Beta-Blocker Therapy and Cardiac Events Among Patients With Newly Diagnosed Coronary Heart Disease. Journal of the American College of Cardiology 2014;64:247–52. doi:10.1016/j.jacc.2014.04.042
- 75Hwang D, Lee JM, Kim HK, et al. Prognostic Impact of β-Blocker Dose After Acute Myocardial Infarction. Circ J 2019;83:410–7. doi:10.1253/circj.cj-18-0662
- 76Dahl Aarvik M, Sandven I, Dondo TB, et al. Effect of oral β-blocker treatment on mortality in contemporary post-myocardial infarction patients: a systematic review and meta-analysis. European Heart Journal – Cardiovascular Pharmacotherapy 2018;5:12–20. doi:10.1093/ehjcvp/pvy034
- 77Hong J, Barry AR. Long-Term Beta-Blocker Therapy after Myocardial Infarction in the Reperfusion Era: A Systematic Review. Pharmacotherapy 2018;38:546–54. doi:10.1002/phar.2110
- 78Zeitouni M, Kerneis M, Lattuca B, et al. Do Patients need Lifelong β-Blockers after an Uncomplicated Myocardial Infarction? Am J Cardiovasc Drugs 2019;19:431–8. doi:10.1007/s40256-019-00338-4
- 79Baker W, Coleman C, Kluger J, et al. Systematic review: comparative effectiveness of angiotensin-converting enzyme inhibitors or angiotensin II-receptor blockers for ischemic heart disease. Ann Intern Med 2009;151:861–71. doi:10.7326/0003-4819-151-12-200912150-00162
- 80Effects of an Angiotensin-Converting–Enzyme Inhibitor, Ramipril, on Cardiovascular Events in High-Risk Patients. N Engl J Med 2000;342:145–53. doi:10.1056/nejm200001203420301
- 81Bangalore S, Fakheri R, Wandel S, et al. Renin angiotensin system inhibitors for patients with stable coronary artery disease without heart failure: systematic review and meta-analysis of randomized trials. BMJ 2017;:j4. doi:10.1136/bmj.j4
- 82Pfeffer MA, Braunwald E. Ventricular remodeling after myocardial infarction. Experimental observations and clinical implications. Circulation 1990;81:1161–72. doi:10.1161/01.cir.81.4.1161
- 83Zannad F, McMurray JJV, Krum H, et al. Eplerenone in Patients with Systolic Heart Failure and Mild Symptoms. N Engl J Med 2011;364:11–21. doi:10.1056/nejmoa1009492
- 84NICE TA607: Rivaroxaban for preventing atherothrombotic events in people with coronary or peripheral artery disease. National Institute for Health and Care Excellence. 2019.https://www.nice.org.uk/guidance/ta607 (accessed Jul 2021).
- 85Connolly SJ, Eikelboom JW, Bosch J, et al. Rivaroxaban with or without aspirin in patients with stable coronary artery disease: an international, randomised, double-blind, placebo-controlled trial. The Lancet 2018;391:205–18. doi:10.1016/s0140-6736(17)32458-3


