Background: Antibiotic resistance is a public health crisis that, if left unchecked, will significantly impact health and global health systems in the coming years. The provision of point-of-care (POC) diagnostic tests could reduce inappropriate use of antibiotics, particularly for the management of respiratory tract infections in the community setting. A POC test for C-reactive protein (CRP) has been successfully trialled in general practice and in a community pharmacy setting — both of these studies had positive outcomes and support the rollout of the service. A group A streptococcus (strep A) POC test has also been studied in a community pharmacy setting with positive outcomes.
Aim: To design and assess a pharmacy-led POC testing service to improve appropriate antibiotic prescribing in cough, cold and flu patients.
Method: A community pharmacy cough, cold and flu self-care service was designed and developed by pharmacists and included POC testing for CRP and strep A. The impact of this service was assessed over a three-month-period from 1 January 2019 to 31 March 2019 in five community pharmacies in Northern Ireland.
Results: 446 patients (of which 21 were ineligible) with symptoms of cough, cold or flu took part in the study. 89% (n=378) stated that they would have visited their GP if the service had not been available. A CRP test was performed for 286 patients (67%). Patients with a CRP value of greater than 80mg/L were referred to a GP for antibiotic treatment. Based on Centor scores of 3 or higher, 13% (n=56) of patients were offered a strep A test, of which 25% (n=14) tested positive and were offered an antibiotic based on a patient group directive. Patients, pharmacists and GPs involved in the study were highly supportive of further rollout of the service; however, pharmacists were concerned about the additional time required to provide the service and requested more training. The estimated savings for Health and Social Care in Northern Ireland were around £3,000 for the study population.
Discussion and conclusion: Community pharmacies are the ideal place to manage minor conditions and can help reduce the workload of GPs. This study provides evidence of a service that reduced GP workload, but also supported more appropriate antibiotic prescribing. Patients, pharmacists and GP staff gave positive feedback for the POC testing service and would like to see the service rolled out to other pharmacies.
Keywords: Antibiotics, C-reactive protein, CRP, point-of-care, POC, community pharmacy, respiratory tract infection, self-care
Original submitted: 1 October 2020; Revised submitted: 4 January 2021; Accepted for publication: 21 January 2021.
Key points
- Point-of-care (POC) testing could facilitate the use of targeted and better-selected antibiotics, potentially improving antibiotic prescribing;
- Two POC tests were provided in a cough, cold and flu community pharmacy service, with the aim of improving antibiotic prescribing for general and common respiratory conditions;
- The service was safe in that patients with potentially serious disease were identified; 44 patients were referred to the GP for immediate assessment;
- Both patients and GPs, from their respective phone follow-up and questionnaires, registered high acceptance of the service, and initial concerns from GPs that patients may feel they were being sidelined into an inferior service compared with a GP visit were not borne out over the study period;
- The service was cost-effective in the management of a self-limiting condition compared with the GP consultation and, therefore, justified investment from a commissioning perspective;
- It was, however, not possible to draw a definitive conclusion on the impact of POC testing on antibiotic prescribing from the current study alone.
Introduction
Antibiotic resistance presents a huge challenge for the NHS and public health if the issue of inappropriate antibiotic use is not addressed[1][2]. Globally, around 700,000 deaths each year are caused by antimicrobial resistance to antibiotics, with estimates that this could rise to 10 million deaths per year by 2050 if nothing is done[2,3]. There is currently significant impetus to address this issue[3,4].
Since antibiotics underpin much of current medical practice, practice will have to change if the problem of resistance is not tackled. Patients will die of illnesses that are currently common conditions and there will be poorer clinical outcomes from infectious diseases (e.g. pneumonia and meningitis)[5]; cancer chemotherapy will carry higher risk, as such treatments can compromise immune systems and antibiotic resistance threatens the efficacy of prophylactic treatments[5]. Similar risks would apply to all forms of transplants and surgical procedures, such as cardiac bypass, hip replacement and caesarean sections[3]. Such medical interventions, which are routine practice today, would be impeded in a post-antibiotic era[4].
In the UK, GPs still use an empirical prescribing approach, where the GP assesses a patient’s physical symptoms and prescribes according to their professional judgment[6]. This approach can lead to unnecessary or inappropriate prescriptions for antibiotics[4]. A 2016 report found that in the United States, out of 154 million primary care visits for which an antibiotic was prescribed, around 47 million — about one third — were unnecessary[7]. The same report estimated that this figure rose to more than 50% for antibiotics used for respiratory infections[7].
Respiratory infections are common and account for most primary care consultations globally[8]. Since as many as 95% of these infections are viral, and there is little evidence that use of antibiotics reduces the number of symptom days for bacterial infections compared with no treatment, there is little clinical justification for use of antibiotics[9]. There is good reason to stop prescribing antibiotics for upper respiratory tract infections in normally healthy adults and a similar case can be made for lower respiratory tract infections[10–12].
Point-of-care (POC) testing could facilitate the use of targeted and better-selected antibiotics in the GP surgery or pharmacy, and thus potentially improve antibiotic prescribing[13,14].
A 2016 study by Hughes et al. evaluated C-reactive protein (CRP) testing in general practice[15]. CRP testing can aid in the differentiation of viral and bacterial infections, as CRP levels are found to be markedly higher in patients suffering with a bacterial infection[16]. Of the 71 patients in the study who received a test for an acute respiratory tract infection, 74.6% (n=53) did not receive an antibiotic, suggesting improved prescribing[15]. CRP testing has been assessed in a community pharmacy setting and, although numbers enrolled into the study were small (n=52), an impact on antibiotic prescribing was identified, along with high patient satisfaction with the service and the potential to reduce GP appointments for respiratory tract infections[17].
POC testing for group A streptococcal (strep A) pharyngitis has been assessed in 35 community pharmacies in England[18]. As part of a sore throat test-and-treat service, 367 patients were initially screened using the Centor scoring system and 41% (n=149) were offered a strep A POC test as a result of their score. Patients testing positive were offered antibiotic treatment. This service suggested improvements in antibiotic prescribing, but there were significant limitations to these suggestions as no specific data on reduction in antibiotic use was reported[18].
The current study is novel in that it offers two POC tests in one community pharmacy service, with the aim of improving antibiotic prescribing for general and common respiratory conditions. To date, studies have only used single POC tests (CRP or Centor/strep A) for specific respiratory conditions and have not been successful in demonstrating improved use of antibiotics[15,17,18]. The government and the NHS have identified community pharmacy as an important, accessible and convenient location for the management of minor conditions[19]. However, this will only happen when there is confidence that these services are as safe and effective as those provided in general practice[10].
Aims and objectives
The aim of this study was to design a community pharmacy service that combined two POC tests to support appropriate prescribing of antibiotics and to measure the impact of the service.
The study objectives were to:
- Assure cost-effective patient treatment outcomes for respiratory tract infections;
- Design a pharmacy service to incorporate CRP and Centor/strep A testing;
- Allow autonomous integrated practice by community pharmacists;
- Support medicines optimisation;
- Demonstrate a reduction in inappropriate antibiotic use.
Methodology
The cough, cold and flu self-care service was designed by a group of community pharmacists, with input from GPs following a literature search. The search identified several studies involving relevant POC tests that were used to improve antibiotic prescribing, which informed the design of the service[15,17,18]. A pilot of the initial service protocol was run in one of the participating pharmacies; 66 patients were enrolled from 18 November 2018 to 31 December 2018 to test the protocol and, where necessary, refine the service. The refined service ran from 1 January 2019 to 31 March 2019 in five pharmacies in Northern Ireland. The pharmacies are owned by Northern Pharmacies Ltd; three were small rural dispensing pharmacies, one was a health centre pharmacy and one was a high street pharmacy.
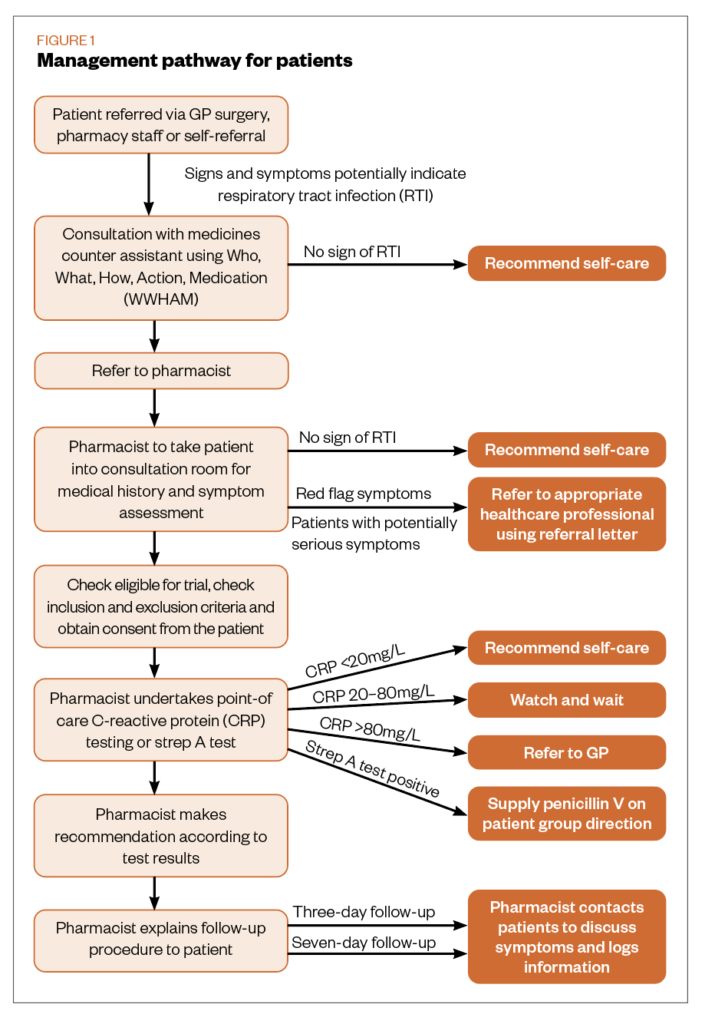
Local GP surgeries were approached, and their support sought for the service. Surgery staff including GPs, practice pharmacists and practice managers were briefed on the service and asked to recommend its use to their patients. Patient management during the service is outlined in Figure 1. In GP surgeries, reception staff assessed whether patients were suitable for the service and, when appropriate, referred them. Appropriate referral criteria included symptoms of cough, cold or flu, individuals aged 12–75 years, and the absence of COPD or asthma. If the patient displayed red flag symptoms during their consultation with the pharmacist, they were referred to an appropriate healthcare professional. Red flag symptoms included: coughing up blood; shortness of breath; wheezing sound; respiratory distress; difficulty swallowing; drooling or muffled voice; and a temperature greater than 39 degrees Celsius.
Equipment
Each pharmacy was provided with testing devices and staff were trained in the use of equipment at a dedicated one-day training event and additional in-pharmacy training support visits. All pharmacy staff were made fully aware of the aims and objectives of the service, and each pharmacy was provided with a service file outlining the service, use of testing equipment and background to antimicrobial stewardship.
In addition, each pharmacy was provided with a folder containing promotional material on antibiotic stewardship to be displayed during the service. This material was also offered to the GP surgery for display. The material used as part of this service was complemented by Public Health Agency leaflets.
Point-of-care testing
Centor test/strep A testing
Centor scores were calculated using the following criteria: fever, absence of cough, tender anterior cervical lymph nodes, tonsillar exudate[20]. Each of the Centor score criteria scored 1 point (max score 4)[20]. A score of <3 is associated with 3–17% likelihood of isolating strep A[21]. A score of 3 or greater is associated with 32–56% likelihood[21]. The modified Centor criteria used in this service added the patient’s age to the criteria[22]. Patients aged 3–14 years received an extra score of 1 point, while patients who were aged 45 years and over had 1 point subtracted from their score[22]. In this service, patients with a sore throat and a Centor score of 3 or greater were offered a strep A test. The service used the OSOM Strep A Test (Sekisui Diagnostics UK Ltd).
Patients with a positive strep A test result were offered antibiotics — either penicillin V or clarithromycin, if allergic — from a patient group direction (PGD). All other patients were offered symptom relief and advice.
C-reactive protein testing
If patients had a productive cough, a CRP test was offered. Patients who presented with only a cough were not assessed for a Centor score as it was not relevant[20].
Staff received training on how to perform the CRP test, using the device available for their pharmacy. The Finecare II system (Wondfo) was used in two pharmacies; this provided quantitative results. A semi-quantitative test was used in the three smaller pharmacies. This was done to reduce costs, as it was not cost-effective to provide the Finecare II system for each of the five pharmacies. The semi-quantitative test used was the ACTIM CRP rapid test (Medix Biochemica). Patients with CRP levels that were ≤20mg/L were deemed to be suffering from a viral respiratory tract infection and offered symptom relief. A watch-and-wait approach was used for patients with a test result of 21–80 mg/L; these patients were offered symptom relief and referred to an appropriate healthcare professional if the follow-up on day three suggested worsening symptoms. Patients with a test result >80mg/L were referred to the GP for further assessment. As this service used semi-quantitative tests, a >80mg/L level was used as the threshold for GP referral, which is lower than the 100mg/L identified in National Institute for Health and Care Excellence (NICE) guidance[23]. It should be noted that NICE withdrew this guideline during the COVID-19 pandemic and the rapid guidelines on managing suspected or confirmed pneumonia in adults in the community and antibiotics for pneumonia in adults in hospital are currently being used.
Temperature
Patient temperature was taken with a Braun ThermoScan ExacTemp IRT6020 thermometer, using the required technique and appropriate training.
Costs and quality control
All costs associated with the development, running and assessment of this service were provided by Northern Pharmacies Ltd and Northern Pharmacies Trust. Quality control support for testing equipment was provided by Sigma. There were also several inbuilt quality controls for the semi-quantitative CRP test and the strep A test kits.
Data collection
Patient data
Data were collected during the patient pharmacy visit on a dedicated form and provided a full record of the patient intervention, recording all details of: assessment; clinical data (temperature, Centor score, strep A test result, CRP test result); and information relating to management (if any advice was provided and any medicines were supplied). A record was made if a patient was referred back to the GP and the reason for this referral. All patients were followed up by phone by a member of the pharmacy staff on day three following the initial assessment to assess how the patient’s symptoms were progressing. It was also noted if they had attended any other healthcare services (GP, out-of-hours or emergency department) for their symptoms. If required, the patient could be referred to their GP (e.g. for worsening symptoms). Patients were followed up on day three as the pilot indicated that most patients did not require a follow-up at day seven; however, following the telephone follow-up on day three, the patients could request to receive a further follow-up call on day seven, if necessary.
Patient satisfaction
People who used the service were asked to provide contact details and were then followed up between April and June 2019 to provide information on how satisfied they were with it. Around half of the patients (n=222) were followed up as part of the patient satisfaction survey, as this was determined sufficient to establish qualitative themes.
Pharmacist assessment
Pharmacists and pharmacy staff completed an assessment form to determine their views of the service and the challenges they experienced in delivering it. In addition, pharmacists and pharmacy support staff were invited to an assessment workshop, where small focus groups provided more detailed feedback.
GP practice assessment
GPs and practice staff completed an assessment form to determine their views on how well the service worked from their perspective and if they had any suggestions for improvement.
The 2-page questionnaire contained 15 questions with ‘Yes’, ‘No’, ‘N/A’ and ‘Unknown’ answer options. The questions covered knowledge of the service, confidence in the service, benefit to the practice, any adverse events and if they would use the service again. There was an option for free-text responses.
Prescribing data
The study aimed to reduce prescriptions for amoxicillin and penicillin V during the study period (1 January 2019 to 31 March 2019). Information on antibiotic prescribing data was obtained for two local medical practices for the service period and that of the previous year (1 January 2018 to 31 March 2018) to determine if there was any change in prescribing data.
Results
Patient demographics
In total, 446 (56.7% [n=253] female, 33.8% [n=151] male, 9.4% [n=42] missing/not provided) patients used the self-care service across the five pharmacies and consented to be included in the evaluation process. Of these, 21 patients were found to be ineligible, mainly owing to being outside of the age inclusion criteria, and so were excluded from the study. An additional 90 patients were lost to follow-up as they did not respond to the phone request. Table 1 shows the breakdown of the number of patients who attended each of the participating pharmacies. Craigavon is a health centre pharmacy with two GP practices on site, which accounts for the higher attendance. Holywood is a high street pharmacy and the others are small rural pharmacies.
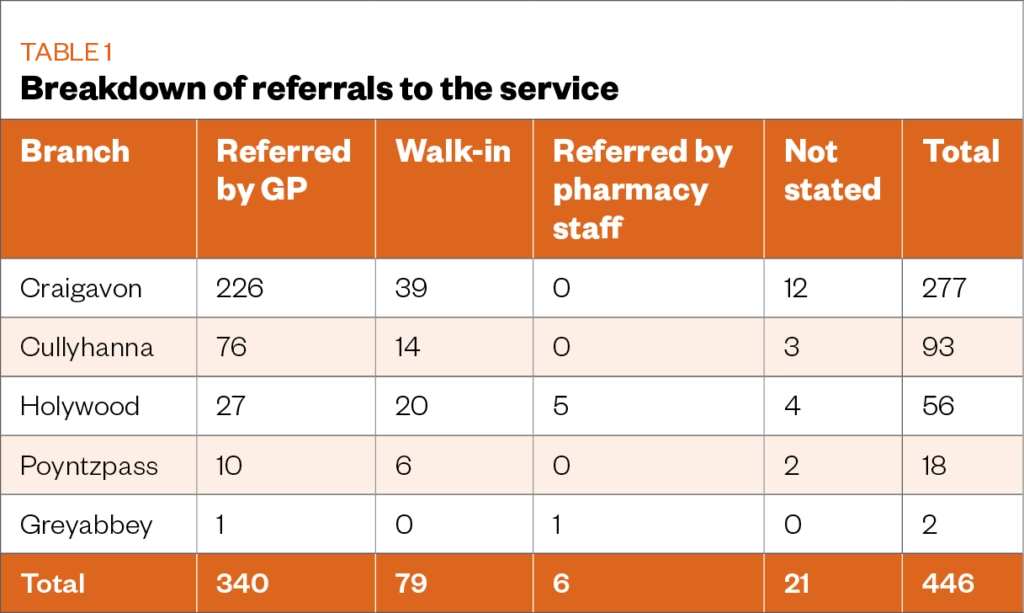
76% (n=340) of the service users were referred via their GP surgery. This was highest (81%; n=226) at Craigavon, where relationships between the pharmacy and GP surgeries in this health centre are particularly strong. Patient feedback suggested that 17% of patients who presented to the service had heard about it through word of mouth or in the local press.
A Centor score was calculated for who presented to the pharmacy with a sore throat, of which 92 were tested for strep A (see Table 2). Of these patients, 56 qualified for testing on Centor score alone.
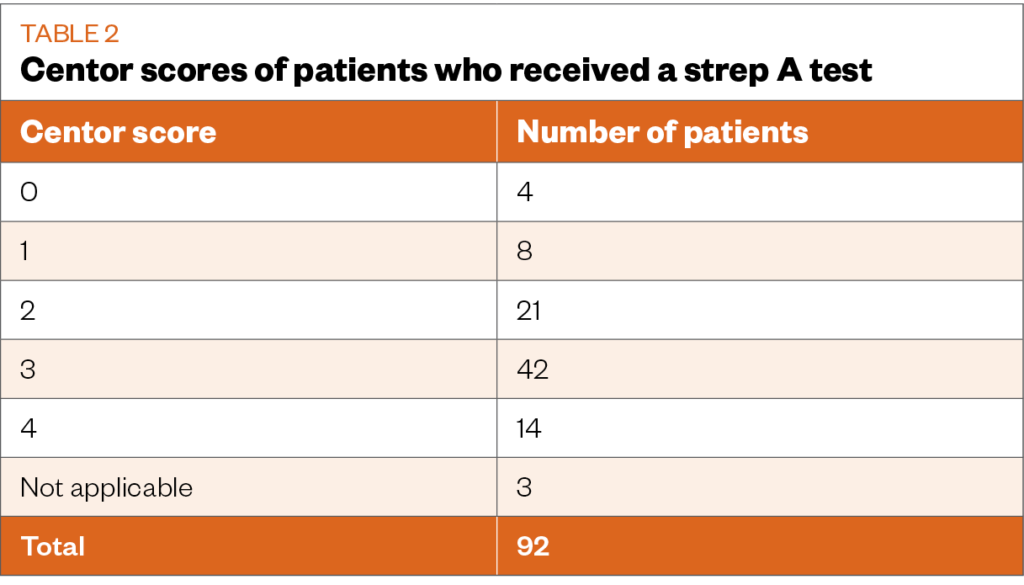
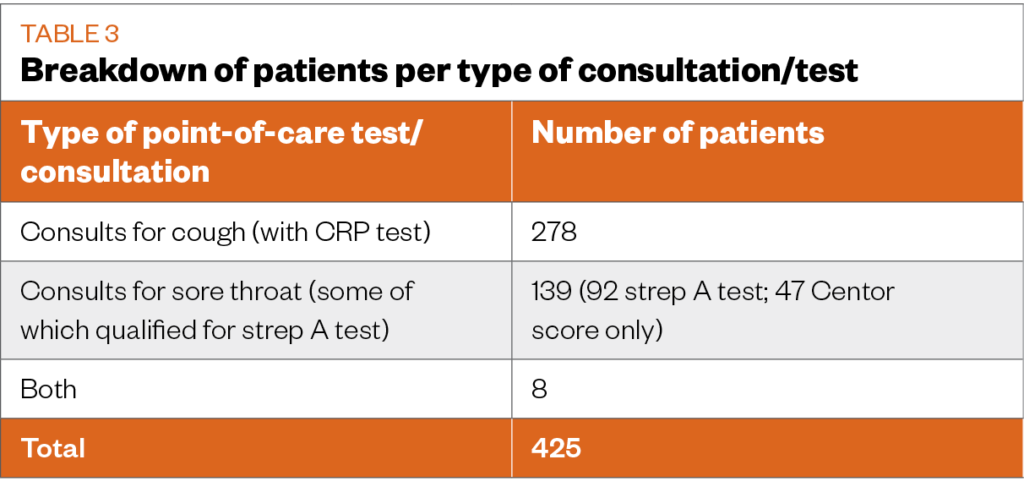
There were 56 patients who scored 3 or more and were offered a strep A test. Of these, 56 (8.2%, n=14) patients received a positive result and were offered antibiotics. In addition, 14% (n=8) of the 56 patients received a CRP test, seven had a result of <20 mg/L and one had a result that was >40mg/L to <80mg/L. All patients in this group were offered symptom relief and advice. At pharmacist discretion — in some cases owing to patient pressure — 36 patients who had a Centor score of less than 3 were given a strep A test; none of these patients returned a positive result. A breakdown of what tests and consultations took place in different patients can be seen in Table 3.
CRP testing
A CRP test was performed for 67.5% (n=286) of the patients, with the majority 81.5% (n=233) carried out using the Finecare II test system. Two patients had a CRP result >80mg/L and these patients were referred to the GP with a recommendation of amoxicillin treatment.
Self-care advice/treatment
In all cases not referred to the GP or treated by the PGD (n=305), patients were provided with advice on the self-care of their condition. This included standard advice on keeping well with a mild viral infection and symptom relief with standard over-the-counter medicines: paracetamol (n=65), ibuprofen (n=22), pseudoephedrine (n=21), cough mixtures (n=13) and throat lozenges (n=15). These medicines were not part of the service and were sold to patients. 23 patients were advised to increase fluid intake, 2 patients were advised to rest and smoking cessation was recommended to 5 patients.
Patient follow-up
Where patients were not referred to their GP following their pharmacy visit, patient feedback during follow-up and the follow-up assessment with GPs indicated that 50 patients independently booked GP appointments with their own GP or an out-of-hours GP. Of these, 98% (n=49) received antibiotics as a result of these consultations. Two patients were admitted to hospital as their condition worsened.
Patient satisfaction
A total of 222 patients took part in the patient satisfaction survey. 94.1% (n=209) of patients stated that they were ‘very likely’ or ‘likely’ to recommend the service. When asked about satisfaction with the service, 96.8% (n=215) stated they were ‘very satisfied’ or ‘satisfied’. Similar levels of satisfaction were found with the advice and/or treatment they received, with 91.9% (n=204) ‘very satisfied’ or ‘satisfied’, and 89% (n=198) indicated that had the service not been available, they would have visited their GP.
Pharmacist questionnaire
Questionnaires were sent to 14 pharmacists and completed by 10 pharmacists, who all felt they had been adequately informed about the new service. Two pharmacists felt that additional training would have been useful, specifically more training on the use of testing equipment. All pharmacists who responded felt confident carrying out the service. One of the main challenges identified was having the time to provide the service within normal pharmacy hours. 80% of respondents (n=11) felt that the service benefited the pharmacy, with the majority citing that they felt the reputation of the pharmacy had benefited. However, some adverse effects were noted by some respondents — staff resource to provide the service (n=4) and increased patient waiting times for other pharmacy services, including dispensing (n=6).
Pharmacy staff focus groups
Focus groups took place in May 2019 to seek staff views on the service, which were attended by 11 pharmacy staff members (7 pharmacists and 4 pharmacy technicians). There were three focus groups comprising five individuals. Each group meeting took place at the same venue and covered the same themes. A report was produced for the three focus groups and themes were identified from the pharmacist questionnaires. These themes covered: training, time to undertake the service, job satisfaction, professional satisfaction and patient care. Staff were positive about the service and in favour of rolling it out more widely. Concerns were identified relating to the amount of training provided, communication with GPs, staffing levels and staff indemnity.
GP questionnaire
Out of 30 questionnaires, 73% (n=22) were received from GPs in practices that engaged with the service. All felt they were adequately informed about the service. GPs identified initial resistance from patients being referred to the service and some patients suggested they were being “fobbed off” and not allowed to see the GP. The GPs indicated that initial resistance soon disappeared as patients experienced the service. One GP noted several patients with a CRP value of <5mg/L returning to the practice seeking antibiotics, but were refused. A total of 50% of GPs (n=11) responding felt the new service altered the practice’s antibiotic prescribing habits in reducing use, and 68.2% of GPs (n=15) did not feel that the service impacted their relationship with their patients. The questionnaire had an option for free-text responses; some of these responses are highlighted in the Box .
Box: Feedback from GPs
“Found it to be very beneficial for all concerned. I would support if permanent — or at least in the winter months.”
“Good service — please make it permanent.”
“Very reliable service. Reduces GP workload. Reduces abx [antibiotic] prescribing.”
Antibiotic prescribing
Antibiotic prescribing information for amoxicillin and penicillin V was received from two local GP practices. Table 4 compares the prescribing of these antibiotics for the period 1 January 2018 to 31 March 2018 and 1 January 2019 to 31 March 2019.
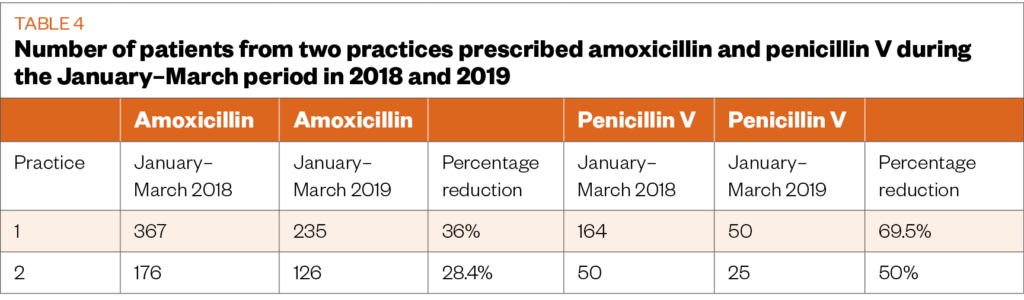
A reduction in the number of prescriptions for both amoxicillin and penicillin V was observed between the two time periods across the two practices.
Service costings
The costs of the tests were £2.25/strep A test, £4.20/quantitative Finecare II CRP test and £5.30/semiquantitative Actim CRP test, with the consumables estimated to cost around £0.15 per patient. Most pharmacies have a consultation room for other services that is regularly used and so the cost of providing this, and for utilities, has not been taken into consideration.
The average time taken per consultation was around 15 minutes for this service. When calculating the costing of the pharmacist’s time, the local locum rate would only be around £4.70 per 15-minute session; however, this figure would not be appropriate for performing a clinical service such as this. The 2019 Personal Social Services Research Unit (PSSRU) figures define the unit cost of a pharmacist’s time as £16.53 for a 15-minute consultation for the management of minor ailments[24,25].
Using these figures, it was estimated that the cost of the service itself would be around £18.93/strep A consultation and test (calculated as: £2.25/strep A test + pharmacist time + consumables = total) or £21.43/CRP consultation and test (calculated as: average cost of CRP tests [£4.75] + pharmacist time + consumables = total).
Using the same PSSRU figures, it is estimated that the average GP appointment lasts 9.2 minutes and costs £39.00[25]. This suggests there would be savings from the provision of the pharmacy-led POC service when compared with a GP appointment for the same complaint, despite a pharmacist requiring more contact time (see Table 5).
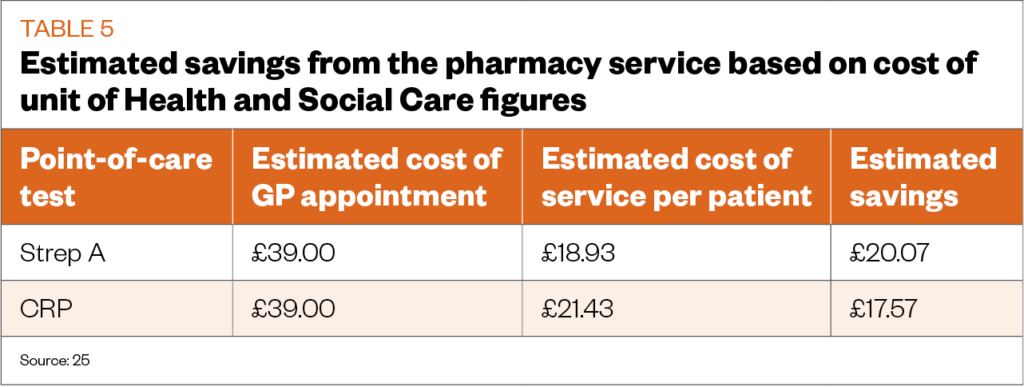
If the average saving, depending on the presenting symptom or test performed, is £18.82 and there were 425 patients involved in the study, there is potential to have saved an estimated £8,000.
However, there would be additional costs. Set-up fees of £1,200 — to include equipment and design — and training costs of up to £3,000 reduces savings to around £3,800. Training costs included the full cost of the training event, and the design and printing of a manual to support the service.
Discussion
This new service brought together two POC tests to provide an accessible service for patients with minor upper and lower respiratory conditions. Individually, these tests have been used successfully for a similar purpose in other studies, but this is the first time that the tests have been combined to address a wider range of common respiratory conditions in one service. The service involved more patients than the previous studies and achieved the same level of acceptability with pharmacists providing the service, the public using the service and GPs[15,17,18].
The service was safe in that patients with potentially serious disease were identified and referred to a GP for immediate assessment. In total, 44 patients were referred in this way. There was no evidence from patient and GP feedback, or from pharmacist follow-up, that any adverse incidents occurred as a result of this service. The two patients who were hospitalised were treated in hospital for a non-infectious exacerbation of COPD and both returned home the next day.
GPs confirmed that, in their view, there was a shift in patients who would normally be seen in general practice to this service, and they viewed the service as improving antibiotic stewardship. GPs reported sending patients seeking antibiotics to the service because test results would improve their empirical prescribing. In total, 25% (n=106) of patients were referred back to the GP either after initial consultation (n=66) or at day 3 follow-up (n=40). While the rate of GP referral from the service may seem high, pharmacists reported in both the questionnaire and the focus groups that triage by the GP reception staff was poor; very ill patients were referred into the service, as were patients who were outside the age range. This highlights a need for better training and support for GP reception staff, or a more effective triage mechanism at the GP surgery to ensure appropriate referral into the service. Of people accessing the service, 89% (n=378) would have otherwise contacted the GP, or had already done so before being directed by GP surgery staff to the service (76%; n=340).
Compared to visiting the GP, the service was cost effective, potentially providing significant cost efficiencies for the health service. Potential savings were in the region of £3,000 for this patient group. However, no additional resource was provided to participating pharmacies and this may have resulted in additional pressures on staff. To roll out the service more widely, these additional costs would need to be invested, which would reduce the identified costs savings. However, the objective of improved antibiotic usage would override the need for these savings.
The service was provided from the pharmacies during normal opening hours without appointment. Feedback from the pharmacy questionnaire and focus groups reported no disruption to other services. Both patients and GPs, from their respective phone follow-up and questionnaires, registered high acceptance of the service and initial concerns from GPs that patients might feel they were being sidelined into an inferior service compared with a GP visit were not borne out over the study period. Where pharmacists providing the service were strongly supportive of it as a positive development for community pharmacy, they did also express concern about the time required to provide the service and its possible impact on the delivery of other services, particularly dispensing.
However, from the pharmacy focus groups that identified these concerns, there was no evidence presented to suggest other services suffered. The time to deliver this service was 15 minutes, on average, which — with appropriate use of other technical and support staff — can be done, but requires additional resources. This would inevitably reduce the cost effectiveness calculated in this pilot. Concerns relating to the amount of training that was received before delivering the service were raised in the pharmacy questionnaire and the focus groups, and would need to be addressed before further rollout of this service.
Clearly, as community pharmacy becomes focused on service delivery and moves away from a medicines supply role, it will be necessary to reconfigure the pharmacy team to accommodate these changes. It has been recognised that, as new services are rolled out across the network, the way current pharmacy services are delivered — particularly dispensing — will need to change[26].
Pharmacists viewed the service as improving their professional standing; this was found in both the pharmacist questionnaire and the focus group. The autonomy of the pharmacist to complete patient management and, where necessary, supply an antibiotic under a PGD without the need for referral back to the GP, was a strong positive theme from the pharmacist focus groups. When designing the service, a commercial PGD was used for penicillin V in the treatment of strep A throat infections. A PGD for amoxicillin was not available for management of lower respiratory tract infection, and there was considerable resistance from local health authorities in the development and provision of one for this study, owing to concern that a PGD could potentially lead to supply of more antibiotics.
This study found that pharmacists, having completed the patient assessment and the required tests, were much less likely to supply antibiotics compared with GPs, who largely employ empirical prescribing. A total of 50 patients, who were not referred back to the GP and not provided with antibiotics by pharmacy staff, then sought GP appointments; of these, 49 were supplied with antibiotics. This reflects the strong “cultural” use of antibiotics, which impacts on their appropriate clinical use[4].
Anecdotal feedback from both the GP questionnaire and the patient follow-up phone calls indicated that when POC test results suggesting a viral infection were communicated to the GP, the supply of an antibiotic was refused. This was not quantified in the current study as it was not part of the project’s evaluation framework, but should be part of the evaluation of any further studies.
Two GP practices involved in the service recorded a reduction in prescribing of both amoxicillin and penicillin V during the POC testing service, compared with the same period for the previous year. However, there are limitations to this finding; the winter of 2019–2020 was unseasonably mild and there was a general reduction in all antibiotic prescribing between the two periods across all GP practices in Northern Ireland. The information was provided by the Medicines Optimisation Innovation Centre (MOIC), which had access to Northern Ireland’s prescribing data. It is, therefore, not possible to draw a definitive conclusion on the impact of POC testing on antibiotic prescribing in the current study[27].
Overall, opinions from patients, pharmacy and GP practice staff seemed to be in favour of the POC testing service, and each group would like to see the service rolled out across Northern Ireland. The feedback received as part of this pilot service will be invaluable in assisting any future rollout of the service as a commissioned service; for example, as part of Pharmacy First.
The emergence of the SARS-CoV-2 virus in late 2019 and the resulting global pandemic will have an impact on any rollout of the service described in this article. The success of the vaccine rollout programme and the control of future infections will ultimately impact on the feasibility of pharmacies to offer and run the service, as strict protocols may still be required to minimise the risk of COVID-19 infection to pharmacy staff.
Conclusion
While this study was unable to provide robust evidence of a reduction in antibiotic use, the reduction seen is encouraging. There is certainly the potential to achieve the objective of optimal use of antibiotics identified in government reports on antibiotic stewardship. The authors are keen that this potential is identified in further studies.
The service was well received by the patients who used it, the pharmacists and pharmacy staff who provided it, and the GP surgeries who referred patients into it. The average duration of an appointment was 15 minutes, which — when factored into a busy pharmacy’s schedule — has the potential to put pressure on staff and resources. Before any future rollout of the service across the pharmacy network, it must be considered how the POC testing service could be provided to all patients wishing to use the service, without impacting the other services the pharmacy provides. The service was cost-effective in the management of a self-limiting condition compared with a GP consultation and, therefore, justified investment from a commissioning perspective.
Acknowledgements and conflicts of interests disclosure
The authors wish to express their appreciation to the Medicines Optimisation and Innovation Centre, Antrim Area Hospital, Antrim, Northern Ireland, for their assessment of data and the independent production of a service report.
The authors have no relevant affiliations or financial involvement with any organisation or entity with a financial interest in or financial conflict with the subject matter or materials discussed in this manuscript.
No writing assistance was used in the production of this manuscript.
References
- 1Davis S. Chief Medical Officer annual report 2011. Volume Two. Infections and the rise of antimicrobial resistance. Public Health England. 2011.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/138331/CMO_Annual_Report_Volume_2_2011.pdf (accessed Jan 2021).
- 2Tackling drug-resistant infections globally: final report and recommendations. THE REVIEW ON ANTIMICROBIAL RESISTANCE. 2016.https://amr-review.org/sites/default/files/160518_Final%20paper_with%20cover.pdf (accessed Jan 2021).
- 3Hall W, McDonnell A, O’Neill J. Super-bugs: An arms race against bacteria. London: : Harvard University Press 2018.
- 4Tacconelli E, Pezzani MD. Public health burden of antimicrobial resistance in Europe. The Lancet Infectious Diseases 2019;:4–6. doi:10.1016/s1473-3099(18)30648-0
- 5Teillant A, Gandra S, Barter D, et al. Potential burden of antibiotic resistance on surgery and cancer chemotherapy antibiotic prophylaxis in the USA: a literature review and modelling study. The Lancet Infectious Diseases 2015;:1429–37. doi:10.1016/s1473-3099(15)00270-4
- 6Krishnakumar J, Tsopra R. What rationale do GPs use to choose a particular antibiotic for a specific clinical situation? BMC Fam Pract Published Online First: December 2019. doi:10.1186/s12875-019-1068-7
- 7Antibiotic Use in Outpatient Settings. Health Experts Create National Targets to Reduce Unnecessary Antibiotic Prescriptions. The Pew Charitable Trusts. 2016.https://www.pewtrusts.org/~/media/assets/2016/05/antibioticuseinoutpatientsettings.pdf (accessed Jan 2021).
- 8Finley C, Chan D, Garrison S, et al. What are the most common conditions in primary care? Systematic review. Can Fam Physician 2018;64:832–40.https://www.ncbi.nlm.nih.gov/pubmed/30429181
- 9Ashworth M, Charlton J, Ballard K, et al. Variations in antibiotic prescribing and consultation rates for acute respiratory infection in UK general practices 1995-2000. Br J Gen Pract 2005;55:603–8.https://www.ncbi.nlm.nih.gov/pubmed/16105368
- 10Exploring the consumer perspective on antimicrobial resistance. Wellcome Trust. 2015.https://wellcome.ac.uk/sites/default/files/exploring-consumer-perspective-on-antimicrobial-resistance-jun15.pdf (accessed Jan 2021).
- 11Respiratory tract infections (self-limiting): prescribing antibiotics. Clinical Guideline 69 [CG69]. National Institute for Health and Care Excellence . 2008.https://www.nice.org.uk/guidance/cg69 (accessed Jan 2021).
- 12Managing common infections: guidance for primary care. Public Health England. 2020.https://www.gov.uk/government/publications/managing-common-infections-guidance-for-primary-care (accessed Jan 2021).
- 13Cals JWL, Ament AJHA, Hood K, et al. C-reactive protein point of care testing and physician communication skills training for lower respiratory tract infections in general practice: economic evaluation of a cluster randomized trial. Journal of Evaluation in Clinical Practice 2010;:1059–69. doi:10.1111/j.1365-2753.2010.01472.x
- 14Hunter R. Cost-Effectiveness of Point-of-Care C-Reactive Protein Tests for Respiratory Tract Infection in Primary Care in England. Adv Ther 2015;:69–85. doi:10.1007/s12325-015-0180-x
- 15Evaluating a point-of-care C-reactive protein test to support antibiotic prescribing decisions in a general practice. Clinical Pharmacist Published Online First: 2016. doi:10.1211/cp.2016.20201688
- 16Haran JP, Beaudoin FL, Suner S, et al. C-reactive protein as predictor of bacterial infection among patients with an influenza-like illness. The American Journal of Emergency Medicine 2013;:137–44. doi:10.1016/j.ajem.2012.06.026
- 17Point-of-care C-reactive protein testing in community pharmacy to deliver appropriate interventions in respiratory tract infections. Clinical Pharmacist Published Online First: 2018. doi:10.1211/cp.2018.20204635
- 18Thornley T, Marshall G, Howard P, et al. A feasibility service evaluation of screening and treatment of group A streptococcal pharyngitis in community pharmacies. J Antimicrob Chemother 2016;:3293–9. doi:10.1093/jac/dkw264
- 19Pharmacy: A Way Forward for Public Health. Public Health England. 2017.https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/643520/Pharmacy_a_way_forward_for_public_health.pdf (accessed Jan 2021).
- 20Centor R, Samlowski R. Avoiding sore throat morbidity and mortality: when is it not ‘just a sore throat?’. Am Fam Physician 2011;83:26, 28.https://www.ncbi.nlm.nih.gov/pubmed/21888123
- 21Sore throat (acute): antimicrobial prescribing. NICE Guidance [NG84]. National Institute for Health and Care Excellence. 2018.https://www.nice.org.uk/guidance/ng84/resources/sore-throat-acute-antimicrobial-prescribing-pdf-1837694694085 (accessed Jan 2021).
- 22Willis BH, Coomar D, Baragilly M. Comparison of Centor and McIsaac scores in primary care: a meta-analysis over multiple thresholds. Br J Gen Pract 2020;:e245–54. doi:10.3399/bjgp20x708833
- 23Pneumonia in adults: Diagnosis and management. Clinical Guidance 191[CG191]. National Institute for Health and Care Excellence. 2019.www.nice.org.uk/guidance/cg191 (accessed Jan 2021).
- 24PSNC Briefing 022/18: Building a business case for a Minor Ailment Service. Pharmaceutical Services Negotiating Committee. 2018.https://psnc.org.uk/wp-content/uploads/2018/04/PSNC-Briefing-022.18-%E2%80%93-Building-a-business-case-for-a-Minor-Ailment-Service.pdf (accessed Jan 2021).
- 25Personal Social Sciences Unit. Unit Costs of Health and Social Care 2019. . University of Kent. 2019.https://www.pssru.ac.uk/project-pages/unit-costs/unit-costs-2019/ (accessed Jan 2021).
- 26Rutter P. Role of community pharmacists in patients' self-care and self-medication. IPRP 2015;:57. doi:10.2147/iprp.s70403
- 27Liu Y, Liu J, Chen F, et al. Impact of meteorological factors on lower respiratory tract infections in children. J Int Med Res 2015;:30–41. doi:10.1177/0300060515586007


