Shutterstock.com
After reading this learning article, you should be able to:
- Understand what croup is and the underlying causes;
- Identify the signs and symptoms of croup, including ’red flag’ symptoms, and know when to refer;
- Understand the treatment options and be able to appropriately counsel worried parents.
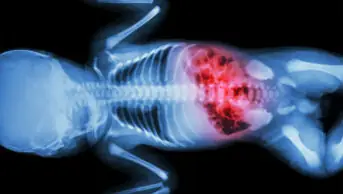
Croup, also known as laryngotracheobronchitis, is a common respiratory disease involving cough, stridor (i.e. creaking, whistling or grating sounds caused by irregular airflow), hoarseness and varying degrees of breathing difficulty. It is a sign of airway obstruction caused by generalised inflammation1–3.
Croup typically occurs in children aged between 6 months and 3 years, peaking at the age of 2 years; it is uncommon after the age of 6 years2,3. It tends to affect males more than females (1.4:1) and there is no evidence to suggest variations in ethnicity prevalence2,4.
Caused by several respiratory tract viruses, croup is most commonly caused by para-influenza virus types 1 and 3 with epidemics occurring every other year2,5. Cases may occur in the UK all year round, but hospital admission rates peak in late autumn (September to December)2,5.
Croup is usually mild and resolves within 48 hours, although some episodes may last for up to one week2. Pharmacists should be able to confidently recognise the symptoms and educate parents on management, including encouraging good oral fluid intake and administering antipyretics5.
Signs and symptoms
Initial signs are similar to a common cold with a low-grade fever and runny nose. Croup symptoms usually develop a few days later, including:
- Barking seal-like cough;
- Hoarse voice;
- Difficulty breathing;
- High pitched, rasping sound when breathing in2,3,6,7.
Symptoms may vary from mild to impending respiratory failure (see Table 1) and tend to be worse at night, with increased agitation2,4. It is usually a short and self-limiting condition, although parents should be aware it may recur after apparently resolving during the day5. Around 80% of children presenting with an acute onset of stridor and a cough have croup1,8.
Mild croup can generally be managed at home; however, hospital admission should be considered in certain circumstances, for example:
- Chronic lung disease;
- Haemodynamically significant congenital heart disease;
- Neuromuscular disorders;
- Immunodeficiency;
- Age under three months;
- Inadequate fluid intake (50–75% of usual volume, or no wet nappy for 12 hours);
- Factors that might affect a carer’s ability to look after a child with croup, (e.g. adverse social circumstances)2.
Box 1 shows when children should be referred urgently to a hospital emergency department.
Box 1: Red flags for urgent referral to hospital emergency department
- Struggling to breathe, grunting and stomach sucking under ribcage;
- Blue/grey/pale skin, lips and tongue;
- Lethargy and difficult to wake;
- Quiet and still;
- Limp and floppy;
- Restless, upset and difficult to calm;
- Swallowing difficulties and drooling.
Risk factors
Although croup can generally be managed at home, referral to a GP or hospital admission may be required as a precaution in children with risk factors for developing severe disease (see Box 2)3,5,8.
Box 2: Risk factors for severe croup
- Patients aged <6 months;
- Prematurity;
- Previous intubation;
- Previous croup;
- Underlying comorbidities, including:
- Neuromuscular disorders;
- Chronic lung disease;
- Trisomy 21 with significant hypotonia.
- Airway abnormalities, including:
- Subglottic stenosis;
- Haemangioma;
- Laryngomalacia or tracheomalacia3,5,8.
Diagnosis
A thorough history and physical examination is required to aid diagnosis. Physical examination typically shows a low-grade fever and no wheezing.
Croup is a largely a clinical diagnosis and involves assessing presence and the severity of symptoms using the Westley Croup Score (see Tables 1 and 2)3 and evaluating respiratory status and rate, retractions, stridor, heart rate, use of accessory muscles and mental status7. The most reliable indicators for assessing severity are the presence of stridor and the extent of retractions7. Pulse oximetry can also help gauge the severity of the disease, because low oxygen levels may be noted in more severe cases7,8. In most acutely ill children, oxygen saturation should be maintained above 92%; some clinicians may aim for a target of 94–98%9.
Patients with red-flag symptoms or symptoms that began abruptly and cause parental concern may present at hospital emergency department7. In a large population-based study, using data from April 1999 to March 2015, there were 27,355 visits for croup, admission occurred in 8.0% of the cases and 5.4% had a repeat visit within 7 days following discharge10.
Laboratory and imaging evaluations are not necessary but can be useful in ruling out other illnesses in children with atypical or severe presentations7. Although chest X-ray cannot diagnose croup, it can rule out other pulmonary conditions when the diagnosis is unclear3,7. Details of the history and physical examination can guide differential diagnosis11. Nearly all children who present with abrupt stridor have croup, but the differential diagnosis is broad8.
Table 3 shows potential differential diagnoses and their associated clinical features2,3,8.
Management
The severity of the child’s condition will guide management of their condition (see Table 1)12. Mild croup can generally by managed at home — see Box 3 for advice pharmacists and pharmacy teams should provide2,5,6,12.
Box 3: How to look after a child with croup at home
DO advise the parent/caregiver to:
- Sit the child upright and try not to let them lie down;
- Comfort them if they’re distressed and try to keep them calm (crying can make the symptoms worse);
- Give them plenty of fluids. For infants who are breastfed, advise continued breastfeeding;
- Check on them regularly, including at night;
- If there are no allergies or contraindications, advise to give paracetamol or ibuprofen, to help ease high temperature or any discomfort.
DO NOT advise the parent/caregiver to:
- Put the child in a steamy room or get them to inhale steam. There is evidence to suggest that putting children into a steamy room can disperse fungus as well as reports of scald injuries. Therefore, this is not advised as a treatment for croup.
Dexamethasone
All children with croup (mild, moderate or severe) should receive a single dose of oral dexamethasone (0.15mg/kg)9,13. Improvement generally begins within 2–3 hours after a single oral dose of dexamethasone and benefit persists for 24–48 hours13. If dexamethasone is not available, oral prednisolone 1mg/kg can be used instead9.
Usually, only a single dose of dexamethasone is needed. A second dose may be needed if the child continues to have problems breathing and is distressed14. Pharmacy teams should advise parents to give the second dose 12 hours after the first dose if the child is awake14.
There is some variation in local guidelines and the evidence suggests that a dose of 0.15mg/kg, and 0.6mg/kg lead to the same reduction in croup scores, admission rates and length of stay in hospital15.
A systematic review of 24 studies investigating the effects and safety of glucocorticoids in the treatment of croup in children, eight reported serious adverse events following the administration of glucocorticoids (namely secondary bacterial infections, e.g. pneumonia, otitis media, bacterial tracheitis) and 16 reported no serious adverse events16.
Common side effects include changes in behaviour, electrolyte imbalances, gastrointestinal discomfort and nausea9.
In general, no contraindications apply in conditions where the use of glucocorticoids may be life-saving17. It is unlikely that children will have any side effects after only one or two doses of dexamethasone for croup14.
Dexamethasone is available as an oral liquid and as 500 micrograms and 2mg tablets. Tablets should be swallowed with a glass of water, squash or juice. Children and their families should be advised not to chew the tablets. The tablets can be crushed if needed and mixed with a small amount of soft food, such as yoghurt, honey or mashed potato14.
If children are unable to tolerate an oral steroid, inhaled budesonide (2mg nebulised as a single dose) or intramuscular dexamethasone (0.6mg/kg as a single dose) are possible alternatives2.
Adrenaline (epinephrine)
For moderate to severe cases, nebulised adrenaline has been found to improve symptom scores at 30 minutes, but the benefits may wear off after 2 hours17. Reports of administering adrenaline in children with severe croup have demonstrated a lower number of cases requiring intubation or tracheotomy13.
The recommended dose of nebulised adrenaline is 400microgram/kg (maximum dose 5mg)9. The dose can be repeated after 30 minutes9.
Side effects are not expected after a single dose of nebulised adrenaline, but can include arrhythmias, confusion, dizziness, dry mouth, hyperglycaemia, hypokalaemia, metabolic acidosis and palpitations9.
Despite early treatment of croup with steroids, some children may not respond and can deteriorate. Nebulised adrenaline often causes a dramatic short-term improvement in symptoms; however, some patients may experience a rebound effect with rapid deterioration18. Continuous monitoring in a medical setting is crucial for children requiring nebulised adrenaline to manage any potential rebound symptoms effectively18.
Children may need supplementary oxygen and additional doses of nebulised adrenaline. Respiratory failure is very rare, with intubation required in 1–3% of all croup cases [8,19]. In children with croup who do not respond to treatment with adrenaline, other causes of acute stridor should be considered8,19.
Other considerations for medication use
Croup is most commonly a viral disease. Antibiotics are reserved for cases when primary or secondary bacterial infection is suspected17.
Pharmacy teams should inform parents/caregivers not to use cough medicines or decongestants, as these medications do not help ease the symptoms of croup20. Often, these treatments can result in drowsy side effects, which can be unsafe when a child has breathing difficulties20.
Complications
Complications from croup are rare but can include respiratory distress and otitis media20. Dehydration may occur if the child is unable to drink fluids. Parents should be advised to watch for signs of complications, such as increased breathing difficulty, high fever or a change in the child’s level of alertness. In rare cases, severe airway obstruction may occur, necessitating urgent medical intervention8,18. Early recognition and treatment of complications can prevent severe outcomes.
Discharge from hospital
Children with mild croup can typically be discharged home after a single dose of dexamethasone. Those with moderate croup should be observed for at least four hours after receiving dexamethasone and then re-assessed to ensure symptom stability1. Clear instructions should be given to parents on what symptoms to monitor and when to seek further medical attention.
For children with moderate to severe croup, parents should receive thorough education on home care strategies, including keeping the child comfortable, monitoring for worsening symptoms and maintaining hydration. Detailed written instructions should be provided and documented in the medical notes1. Follow-up care should be arranged to reassess the child’s recovery and address any ongoing concerns, which will likely be determined on a case-by-case basis.
Prevention advice
Prevention of croup primarily involves reducing the risk of upper respiratory infections. Parents should be advised to:
- Ensure the child practices good hand hygiene, including regular hand washing with soap and water;
- Keep the child away from individuals who are sick, particularly those with respiratory infections;
- Ensure the child is up to date with vaccinations, including the influenza vaccine, as viral infections can trigger croup;
- Avoid exposure to tobacco smoke, as this can exacerbate respiratory conditions20–24.
When communicating with worried parents, pharmacy teams should:
- Use clear, simple language to explain the child’s condition and treatment plan, avoiding medical jargon;
- Provide reassurance by explaining the common course of croup and the effectiveness of treatments such as dexamethasone;
- Encourage parents to ask questions and express their concerns, ensuring they feel heard and understood;
- Offer practical advice on what to do if symptoms worsen, and provide written instructions to reinforce verbal information;
- Demonstrate empathy and understanding, acknowledging their fears and providing support throughout the child’s illness13,25–28.
- 1.Acute Stridor. RCEM Learning. Published 2021. Accessed August 2024. https://www.rcemlearning.co.uk/reference/croup/#1568728736131-14e3d23f-f2a6
- 2.Croup. National Institute for Health and Care Excellence. Published 2022. Accessed August 2024. https://cks.nice.org.uk/topics/croup
- 3.Croup. BMJ Best practice. Published 2024. Accessed August 2024. https://bestpractice.bmj.com/topics/en-gb/681
- 4.Bjornson CL, Johnson DW. Croup in children. CMAJ. 2013;185(15):1317-1323. doi:10.1503/cmaj.121645
- 5.Wright M, Bush A. Assessment and management of viral croup in children. Prescriber. 2016;27(8):32-37. doi:10.1002/psb.1490
- 6.Croup. NHS. Published 2023. Accessed August 2024. https://www.nhs.uk/conditions/croup/
- 7.Zoorob R, Sidani M, Murray J. Croup: an overview. Am Fam Physician. 2011;83(9):1067-1073. https://www.ncbi.nlm.nih.gov/pubmed/21534520
- 8.Smith D, McDermott A, Sullivan J. Croup: Diagnosis and Management. Am Fam Physician. 2018;97(9):575-580. https://www.ncbi.nlm.nih.gov/pubmed/29763253
- 9.BNF for Children. BNF for Children. Accessed August 2024. https://bnfc.nice.org.uk/
- 10.Rosychuk RJ, Klassen TP, Metes D, Voaklander DC, Senthilselvan A, Rowe BH. Croup presentations to emergency departments in Alberta, Canada: A large population‐based study. Pediatric Pulmonology. 2009;45(1):83-91. doi:10.1002/ppul.21162
- 11.Petrocheilou A, Tanou K, Kalampouka E, Malakasioti G, Giannios C, Kaditis AG. Viral croup: Diagnosis and a treatment algorithm. Pediatr Pulmonol. 2014;49(5):421-429. doi:10.1002/ppul.22993
- 12.Moore M, Little P. Humidified air inhalation for treating croup: a systematic review and meta-analysis. Family Practice. 2007;24(4):295-301. doi:10.1093/fampra/cmm022
- 13.Ortiz-Alvarez O. Acute management of croup in the emergency department. Paediatrics & Child Health. 2017;22(3):166-169. doi:10.1093/pch/pxx019
- 14.Dexamethasone for croup. Medicines For Children. Accessed August 2024. https://www.medicinesforchildren.org.uk/medicines/dexamethasone-for-croup/
- 15.Dexamethasone 10mg/5ml Oral Solution – Summary of Product Characteristics. Electronic Medicines Compendium. Published 2023. Accessed August 2024. https://www.medicines.org.uk/emc/product/5289/smpc
- 16.Russell KF, Liang Y, O’Gorman K, Johnson DW, Klassen TP. Glucocorticoids for croup. Cochrane Database of Systematic Reviews. Published online January 19, 2011. doi:10.1002/14651858.cd001955.pub3
- 17.Çetinkaya F, Tüfekçi BS, Kutluk G. A comparison of nebulized budesonide, and intramuscular, and oral dexamethasone for treatment of croup. International Journal of Pediatric Otorhinolaryngology. 2004;68(4):453-456. doi:10.1016/j.ijporl.2003.11.017
- 18.Sakthivel M, Elkashif S, Al Ansari K, Powell CVE. Rebound stridor in children with croup after nebulised adrenaline: does it really exist? Breathe. 2019;15(1):e1.1-e7. doi:10.1183/20734735.0011-2019
- 19.Sizar O, Carr B. statpearls. Published online July 24, 2023. http://www.ncbi.nlm.nih.gov/books/NBK431070/
- 20.Peate I. Croup—a common childhood upper respiratory tract disease. British Journal of Healthcare Assistants. 2022;16(4):178-183. doi:10.12968/bjha.2022.16.4.178
- 21.Handwashing: Clean Hands Save Lives. Centers for Disease Control and Prevention. Accessed August 2024. https://www.cdc.gov/handwashing/index.html
- 22.Managing Infectious Diseases in Schools. American Academy of Pediatrics. Published 2023. Accessed August 2024. https://www.aap.org/en/patient-care/school-health/managing-infectious-diseases-in-schools/#:~:text=On%20this%20page%3A-,Prevention%20Strategies,to%20keep%20their%20bodies%20healthy
- 23.Vaccines and Immunization. World Health Organization. Accessed August 2024. https://www.who.int/health-topics/vaccines-and-immunization
- 24.Passive smoking. NHS. Published 2022. Accessed August 2024. https://www.nhs.uk/live-well/quit-smoking/passive-smoking-protect-your-family-and-friends/
- 25.Health Literacy Toolkit. 2nd Edition, 2023. NHS. Published 2023. Accessed August 2024. https://library.nhs.uk/wp-content/uploads/sites/4/2023/06/Health-Literacy-Toolkit.pdf
- 26.Patient Communication. American Medical Association. Accessed August 2024. https://www.ama-assn.org/topics/patient-communication
- 27.The SHARE Approach. Agency for Healthcare Research and Quality. Accessed August 2024. https://www.ahrq.gov/health-literacy/professional-training/shared-decision/index.html#:~:text=AHRQ’s%20SHARE%20Approach%20is%20a,matters%20most%20to%20the%20patient
- 28.Moudatsou M, Stavropoulou A, Philalithis A, Koukouli S. The Role of Empathy in Health and Social Care Professionals. Healthcare. 2020;8(1):26. doi:10.3390/healthcare8010026