PA Images/Alamy Stock Photo
In the UK, substance use disorders remain a significant public health challenge. In 2021, the Scottish government identified it as a national priority1. According to the Office for National Statistics, almost 3 million people aged 16 to 59 years in the UK have used illicit substances in the year to March 20242. The charity Scottish Families affected by Alcohol and Drugs (SFAD) has also estimated that for every person who uses substances, 11 more people are impacted3.
For individuals impacted by substance use, pharmacies are often an accessible and trusted point of care. Pharmacy teams, with their expertise in medication management, are ideally positioned to support people living with substance use disorders and make a lasting impact on their health and well-being. Pharmacies buck the inverse care law (the principle that people who are most in need of health care are the least likely to receive it) and are more commonly found in areas of deprivation within the UK, where the most harms occur4.
In this article, we outline seven important considerations aimed at improving pharmacy services for individuals affected by substance use across the UK. By implementing evidence-based practices and adapting to new evidence and trends in substances — alongside joint working with health and social care partners at a strategic level — pharmacy teams can provide professional care in supportive, non-stigmatising, trauma-aware environments. Pharmacy services can enhance their ability to greatly reduce harm, support recovery and improve outcomes for individuals.
1. Harm reduction
Harm reduction is the foundation of substance use treatment. While there is ongoing debate around the move from focusing solely on abstinence, harm reduction strategies are aimed to minimise the negative health effects associated with substance use, while respecting an individual’s right to choice5. Pharmacies are well placed in communities to facilitate these approaches through commissioned services, such as injecting equipment provision, supervised consumption of opioid agonist treatment (OAT) and education on safer substance use practices6–8.
Example: The provision of OAT through pharmacies, where the opioid agonist medications, methadone or buprenorphine are dispensed under supervision or administered (in the case of long-acting injectable formulations), have been shown to significantly reduce the risk of non-fatal overdose and deaths, transmission of infectious diseases and anti-social behaviour associated with substance use9,10. Many pharmacies, as part of their injecting equipment provision, offer education on safer injection techniques, blood-borne virus screening, vaccination and treatment, as well as advice on preventing overdose8.
Key message: Commissioners and pharmacy bodies should actively advocate for expanded harm-reduction services within all community pharmacies, including injecting equipment provision, holding of and distribution of naloxone and, where clinically required, supervised consumption. This will reduce the risks associated with substance use and encourage safer practices among individuals.
2. Improving access to opioid agonist treatment
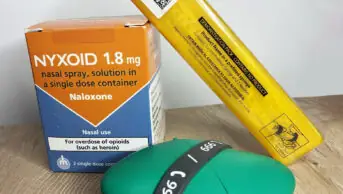
OAT is an effective, evidence-based treatment for individuals with opioid use disorder. Pharmacies can play a vital role in improving access to OAT by offering a flexible and community-based approach to care. This can include dispensing and/or administering medications such as methadone, buprenorphine or naloxone, as well as providing support and guidance for individuals prescribed OAT.
Example: Increasing access to naloxone for emergency reversal of opioid overdose is crucial. In parts of the UK, pharmacies hold naloxone for emergency use and may supply take-home naloxone, which has been shown to save lives by enabling rapid intervention in overdose situations11. By integrating naloxone holding and supply as a core part of substance use service provision, pharmacies can contribute to reducing deaths from opioid overdoses11.
For information about establishing a naloxone supply in hospitals, see ‘How to implement a naloxone supply approach in hospitals’12.
Key message: Pharmacists should ensure they are familiar with local and national guidance, such as that produced by the Office for Health Improvement and Disparities (OHID)6 or the Scottish Medication Assisted Treatment (MAT) Standards7, which are aimed to provide holistic support to people on their recovery journeys and create flexible service models that allows for positive risk-taking around dispensing frequencies and monitoring.
Access to OAT can allow people with substance use disorders to engage in employment, training and volunteering to support them to feel more valued by society and promote recovery13.
3. Creating a stigma-free and psychologically safe environment
Individuals struggling with substance use disorders often face stigma and discrimination14. This can prevent them from seeking help or engaging with services. The extent of the stigma experienced may include pharmacies and pharmacy staff15. Pharmacies must create a non-stigmatising environment to ensure that people feel comfortable in accessing care16,17. Training pharmacy staff is crucial to helping them understand the challenges faced by people with substance use disorders and showing empathy around the drivers of their substance use.
For more information, see ‘How to improve pharmacy services by integrated trauma-informed care’18.
Example: Developing a shared approach where people feel like partners in their recovery journey can enhance treatment engagement and retention in services7. This means offering services with respect, privacy and dignity, whether it is in a private consultation space or when dispensing medications. Providing clear, compassionate communication about treatment options, side effects and expectations can help people make informed and engaged decisions about their care8.
Key message: Pharmacy teams must undergo training in trauma-informed care and non-stigmatising language to create an inclusive and supportive environment18,19. This can help people visiting the pharmacy feel more comfortable discussing their health concerns and seeking help when needed20,21.
4. Strengthening collaboration with multidisciplinary health and social care teams
The treatment of substance use disorders requires a multidisciplinary approach across the whole of healthcare and social care. Pharmacy teams can play a pivotal role within this, across health, social care and the third sector. Strong partnerships between pharmacies and substance use services ensure that people receive the holistic care they need to support their recovery7,8,22 . Pharmacy teams can develop this by initiating contact with GP practice teams, community mental health teams and substance use services to discuss any concerns or ways to improve their care or reduce risks. Pharmacy leaders and pharmacy teams should use all opportunities to advocate for pharmacy teams to be included in multidisciplinary team meetings and case conferences.
Example: The integration of psychosocial support alongside MAT in the Scottish MAT standards7. Offering counselling and therapy services in partnership with local organisations can significantly improve outcomes by addressing the underlying psychological issues that often accompany substance use disorders, such as trauma or co-occurring mental health conditions22.
The introduction of an electronic reporting system (e.g. NEO360) allows community pharmacies to communicate concerns/issues directly to prescribers and key workers in a timeous and auditable manner. This communication allows addiction services to react and follow up on the messages received from the community pharmacy, as well as help patients in urgent need of increased support and assistance.
Key message: Pharmacies should establish close working relationships with local substance use services, mental health services, third-sector partners and wider social-support services, such as housing and welfare benefits, to provide holistic care that addresses both the physical and psychological aspects of substance use.
5. Promoting education and awareness
Pharmacists can provide education on the population who use substances, the risks associated with substances and the importance of seeking professional and peer help. This role goes beyond the individual using substances and can include friends and family members, as well as the wider community. Public-health campaigns and outreach activities — such as offering information on the risks of substance use, supporting national campaigns to reduce stigma or substance use prevention — can provide individuals with knowledge and reduce the stigma surrounding substance use disorders17.
Example: The Royal Pharmaceutical Society’s ‘Improving care of people with mental health conditions in Scotland’ is an example of how national bodies can work with members of parliament to promote the role of pharmacy to maintain and improve the mental and physical health of people who use pharmacies23.
Key message: Pharmacies should take an active role in education by providing information on the risks of substance use, available treatment options and how to seek help. Pharmacies can do this by displaying educational materials (e.g. posters, leaflets), training staff to engage in brief interventions and signposting. Local services can be invited to use space in the pharmacy to help raise awareness of their services. These actions can help reduce stigma and encourage individuals to access necessary services.
6. Respecting the right to confidentiality and privacy
Confidentiality is the foundation of pharmacy standards, especially when working with individuals impacted by substance use. Many people with substance use disorders are reluctant to seek help, owing to concerns about their privacy and the stigma they may face24. Pharmacies must be careful to strike the right balance when sharing information on an individual to maintain the trusting relationship with individuals accessing care.
Example: When a person first presents with a prescription for an opioid agonist treatment, be clear with them when you will share information. For example, you may check with the prescriber if they do not collect their medication or if there are concerns about changes in their behaviour. There are some aspects of data collection that pharmacies are required to undertake legally — for example, controlled drug records and maintaining patient records25,26. They are also required legally to pass on any concerns where someone may be at risk of harm — for example, in cases of child or adult protection. Explain to the patient that, whenever possible and appropriate, this will be done with their agreement; however, in some cases pharmacists may do so, even if they do not agree.
Key message: Pharmacies should have robust confidentiality policies and data-sharing agreements in place to ensure appropriate sharing of information and privacy, particularly when discussing sensitive issues such as substance use. Clear communication about how personal information will be handled can reassure people that their care will remain private6,27.
7. Building trust through consistent care and support
People impacted by substance use disorders often experience periods of relapse. Recovery is rarely a smooth process. For many, this can lead to feelings of shame around failure, frustration at a lack of willpower and a reluctance to return to treatment. Pharmacies can build trust by offering consistent, non-punitive care, understanding the complexities of addiction and supporting individuals through their recovery journey28.
Example: People may test boundaries when building relationships by enquiring about issues of lower significance. For example, during advice for a minor ailment related to their substance use, they may say that they had a slip-up and used a small amount of illicit drugs. Depending on the response or reaction to this, they may then ask for advice on an infected injecting site or ask for injecting equipment. Pharmacy staff can support individuals by responding in a supportive non-judgemental way, reassuring them that this is very common and many people occasionally use substances on their road to recovery. The most important thing is for the patient to be open with you so that you can help support them to get the best care and treatment.
Key message: Pharmacists can support people being retained in treatment by maintaining regular, supportive interactions. Provide reassurance that relapses are part of the recovery process and most people have them. Relapses can be viewed as part of the learning experience in developing alternate coping mechanisms. Encourage them to remain engaged in their treatment plan.
Summary
Pharmacy services have a key role in supporting individuals impacted by substance use disorders in the UK8,28. By supporting harm reduction strategies, providing accessible medication-assisted treatment in communities close to where people live, delivering non-judgmental and stigma-free environments and working closely with other healthcare professionals, pharmacies can contribute to improved health outcomes for people living with substance use disorder23. Most importantly, a person-centred, trauma-informed approach based on empathy, respect and understanding will be crucial to achieving lasting, positive change in the lives of these individuals11,21,28.
- 1.Drugs policy – update: statement by the First Minister . Scottish Government. January 2021. Accessed December 2025. https://www.gov.scot/publications/update-drugs-policy
- 2.Drug misuse in England and Wales: year ending March 2024. Office for National Statistics. 2024. Accessed December 2025. https://www.ons.gov.uk/peoplepopulationandcommunity/crimeandjustice/articles/drugmisuseinenglandandwales/yearendingmarch2024
- 3.Bradley R. Families harmed by alcohol and drugs waiting 8 years for support. Scottish Families Affected by Alcohol and Drugs. 2021. Accessed December 2025. https://www.sfad.org.uk/families-harmed-by-alcohol-and-drugs-waiting-8-years-for-support
- 4.Todd A, Thomson K, Kasim A, Bambra C. Cutting care clusters: the creation of an inverse pharmacy care law? An area-level analysis exploring the clustering of community pharmacies in England. BMJ Open. 2018;8(7):e022109. doi:10.1136/bmjopen-2018-022109
- 5.Logan DE, Marlatt GA. Harm reduction therapy: a practice‐friendly review of research. J Clin Psychol. 2010;66(2):201-214. doi:10.1002/jclp.20669
- 6.Community pharmacy: delivering substance misuse services. Office for Health Improvement & Disparities. 2024. Accessed December 2025. https://www.gov.uk/government/publications/community-pharmacy-delivering-substance-misuse-services/community-pharmacy-delivering-substance-misuse-services
- 7.Medication Assisted Treatment (MAT) standards: access, choice, support. Scottish Government. 2021. Accessed December 2025. https://www.gov.scot/publications/medication-assisted-treatment-mat-standards-scotland-access-choice-support/pages/2/
- 8.The pharmacy team’s role in reducing harm and preventing drug deaths. Royal Pharmaceutical Society. 2021. Accessed December 2025. https://www.rpharms.com/recognition/all-our-campaigns/policy-a-z/drug-deaths-and-the-role-of-the-pharmacy-team
- 9.Guidance Part 1: introducing opioid substitution treatment (OST). Public Health England. July 2021. Accessed December 2025. https://www.gov.uk/government/publications/opioid-substitution-treatment-guide-for-keyworkers/part-1-introducing-opioid-substitution-treatment-ost
- 10.Santo T Jr, Clark B, Hickman M, et al. Association of Opioid Agonist Treatment With All-Cause Mortality and Specific Causes of Death Among People With Opioid Dependence. JAMA Psychiatry. 2021;78(9):979. doi:10.1001/jamapsychiatry.2021.0976
- 11.Take-home naloxone: could community pharmacies be the answer to tackling drug deaths? Pharmaceutical Journal. Published online 2025. doi:10.1211/pj.2025.1.358268
- 12.How to implement a naloxone supply approach in hospitals. Pharmaceutical Journal. Published online 2025. doi:10.1211/pj.2025.1.385494
- 13.Martin E, Maher H, McKeon G, Patterson S, Blake J, Chen KY. Long-acting injectable buprenorphine for opioid use disorder: A systematic review of impact of use on social determinants of health. Journal of Substance Abuse Treatment. 2022;139:108776. doi:10.1016/j.jsat.2022.108776
- 14.Tackling the stigma of addiction. Scottish Government. 2021. Accessed December 2025. https://www.gov.scot/news/tackling-the-stigma-of-addiction
- 15.Weir N, Dunlop E, MacKenzie A, et al. Professionalism, professional identity and community pharmacy culture: The context of substance dependency through the lens of student and early career pharmacists. Addiction. Published online September 25, 2025. doi:10.1111/add.70180
- 16.Mackenzie A. Positive Pharmacy Experiences. Healthcare Improvements Scotland. Accessed December 2025. https://www.healthcareimprovementscotland.scot/publications/reflective-insights-on-positive-pharmacy-experiences-december-2024
- 17.Understanding Mental Health Stigma and Discrimination. See Me Scotland. 2021. Accessed December 2025. https://www.seemescotland.org/stigma-discrimination/understanding-mental-health-stigma-and-discrimination
- 18.How to improve pharmacy services by integrating trauma-informed care. Pharmaceutical Journal. Published online 2025. doi:10.1211/pj.2025.1.380861
- 19.A glossary of contested terms in substance use. Scottish Drugs Forum. 2020. Accessed December 2025. https://www.drugsandalcohol.ie/33136/1/Moving-Beyond-People-First-Language.pdf
- 20.SAMHSA’s concept of trauma and guidance for a trauma-informed approach. Substance Abuse and Mental Health Services Administration. 2014. Accessed December 2025. https://library.samhsa.gov/sites/default/files/sma14-4884.pdf
- 21.Matheson C, Hunter C, Schofield J, et al. Making community pharmacies psychologically informed environments (PIE): a feasibility study to improve engagement with people using drug services in Scotland. Prim Health Care Res Dev. 2023;24. doi:10.1017/s1463423623000087
- 22.Working definition of trauma-informed practice. Office for Health Improvement & Disparities. 2022. Accessed December 2025. https://www.gov.uk/government/publications/working-definition-of-trauma-informed-practice/working-definition-of-trauma-informed-practice
- 23.Improving care of people with mental health conditions: how pharmacists can help. Royal Pharmaceutical Society. 2020. Accessed December 2025. https://www.rpharms.com/Portals/0/RPS%20document%20library/Open%20access/Policy/Scottish%20Mental%20Health%20Policy%202020.pdf
- 24.Schomerus G, Schindler S, Rechenberg T, et al. Stigma as a barrier to addressing childhood trauma in conversation with trauma survivors: A study in the general population. Kamperman AM, ed. PLoS ONE. 2021;16(10):e0258782. doi:10.1371/journal.pone.0258782
- 25.Data handling, record keeping and disposal. Community Pharmacy England. January 2021. Accessed December 2025. https://cpe.org.uk/digital-and-technology/data-security/data-handling-record-keeping-and-disposal/
- 26.Controlled Drugs records in pharmacy. Specialist Pharmacy Service. June 2023. Accessed December 2025. https://www.sps.nhs.uk/articles/controlled-drugs-records-in-pharmacy/
- 27.Drug misuse and dependence: UK guidelines on clinical management. Public Health England. 2019. Accessed December 2025. https://www.gov.uk/government/publications/drug-misuse-and-dependence-uk-guidelines-on-clinical-management
- 28.Improvement Support for MAT Standards Implementation: Assessing the impact and implications of the MAT standards on community pharmacy services. Healthcare Improvement Scotland. 2024. Accessed December 2025. https://www.healthcareimprovementscotland.scot/publications/medication-assisted-treatment-mat-standards-pharmacy-impact-report-april-2024