Shutterstock.com
The National Institute of Health and Care Excellence (NICE) has not recommended the gene therapy treatment exagamglogene autotemcel (Casgevy; Vertex Pharmaceuticals) for the treatment of sickle cell disease (SCD) in patients aged 12 years and over with recurrent vaso-occlusive crises (VOCs).
Draft guidance, published on 14 March 2024, said the NICE committee considered the cost-effectiveness estimate for Casgevy to be higher than what NICE normally considers to be an acceptable use of NHS resources.
The draft NICE guidance said more information was required to “address the uncertainties in the clinical and economic evidence” owing to “several issues with the economic modelling” and requested the manufacturers for “additional data” beyond the current proposal.
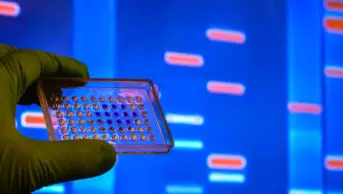
Casgevy was licensed by the Medicines and Healthcare products Regulatory Agency (MHRA) in November 2023 for treatment of SCD and transfusion-dependent β-thalassemia. Casgevy is the first medicine to be licensed in the UK that uses CRISPR, the innovative gene-editing tool.
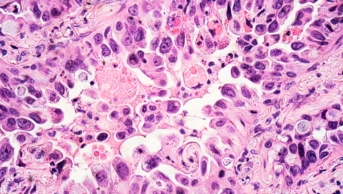
Treatment involves collecting the person’s blood stem cells that are then edited in a lab to produce high levels of foetal haemoglobin in red blood cells. These are then returned to the body in a single infusion.
Helen Knight, director of medicines evaluation at NICE, commented: “The appraisal committee considered that exa-cel could represent a potential cure for some people with SCD, freeing people from the burden of VOCs as well as addressing NICE’s aim of reducing health inequalities associated with the condition.
“As such, and acknowledging the limitations with the evidence, NICE is willing to accept higher than the usual maximum for assessing cost-effectiveness.
“NICE and Vertex are ready to work together to address the issues highlighted in this draft guidance and in particular explore how the uncertainty in the evidence could be addressed through an updated managed access proposal. This would allow people to have treatment with exa-cel while more evidence is collected,” she added.
SCD is an inherited red blood cell disorder affecting around 14,000 people in the UK. It is most common in people with African, Caribbean, Middle Eastern or South Asian heritage.
There are limited treatment options for SCD, with Casgevy being one of only two treatments approved in the UK in the past 20 years.
Crizanlizumab (Adakveo; Novartis) was recommended by NICE for preventing recurrent sickle cell crisis in October 2021, but the marketing authorisation was withdrawn by the MHRA on 10 January 2024 after the drug’s clinical benefit was not confirmed in a phase III study.
Casgevy is the second treatment for SCD to be rejected by NICE in the past month, following rejection of voxelotor (Oxbryta; Pfizer) in February 2024 owing to lack of evidence in clinical trials to support its cost-effectiveness.
John James, chief executive of the Sickle Cell Society, which supports and represents people affected by SCD, said: “This is yet another shocking let down by NICE when it comes to approving new treatments for SCD.
“It highlights NICE’s limited grasp of the profound impact the condition has on people’s quality of life. It also demonstrates shortcomings in the tools they use to effectively evaluate new gene therapy treatments,” he added.
“For the UK’s fastest-growing genetic blood condition, progress in accessing safe and effective treatments remains frustratingly slow for those affected by sickle cell.
“We’ll keep working with the sickle cell community, our medical experts and our partners Anthony Nolan Trust to gather the real-world evidence that NICE is currently failing to recognise,” he added.
The final NICE guidance is expected to be published on 17 July 2024.