Abstract
Aim
To evaluate the results of a survey of male prisoners attending a pharmacist-led dermatology clinic.
Design
Confidential questionnaire survey.
Subjects and Setting
Male prisoners attending a pharmacist-led dermatology clinic at HMP Moorland and HMP Lindholme, both in Doncaster.
Results
85% of 106 respondents stated that their condition was either “better” or “much better” after treatment by the pharmacist. 98% were happy to reconsult the pharmacist. 96% stated that they were “satisfied” or “very satisfied” with the advice received. 97% stated that they gained a better understanding of their condition after visiting the clinic. 62% of additional comments provided by 47 respondents were positive about the pharmacist.
Conclusion
Prisoners treated by the pharmacist were generally satisfied with the treatment and advice that they received at the clinics.
The true prevalence of skin diseases is unknown although estimates suggest that between a third and a quarter of the population are affected at some time in their lives.1 A community-based survey some 30 years ago estimated the prevalence of skin diseases requiring medical care at 22.5 per cent2 and it has been estimated that dermatological conditions account for between 15 and 20 per cent of a typical GP’s workload.3 The incidence in skin disorders seen in community pharmacies is unknown although probably of a similar order of magnitude. One study in Maltese community pharmacies suggested a prevalence of four to five skin-related cases per day.4 Skin diseases, although rarely life-threatening, have a hugely negative psychological effect3 and there is evidence that, for conditions such as acne, the impact on quality of life is as great as other chronic conditions such as epilepsy and diabetes.5 In primary care as much as three quarters of all dermatological consultations are for a small number of conditions, namely, acne, eczema, psoriasis and leg ulcers.3 Since three of these conditions can be treated to some extent with preparations available over the counter, it was decided to explore potential role of a pharmacist in the initial management of patients with skin problems.
The present work describes the results of a confidential survey conducting among prisoners attending pharmacist dermatology clinics6 at HMP Moorland and HMP Lindholme, which are all-male prisons in Doncaster. The objectives were to assess prisoners’ views on how they perceived their condition after treatment from the pharmacist, to determine whether or not prisoners were likely to revisit the pharmacist with the same or another skin problem in the future and to assess the level of satisfaction with the advice received by the pharmacist.
Methods
A total of 181 prisoners were seen at the clinics. A six-item questionnaire was developed which evolved from an earlier questionnaire described elsewhere.7 The new questionnaire was piloted with a sample of 10 prisoners and no problems were revealed. All prisoners who received treatment were invited to complete a questionnaire at a follow-up appointment. The timescale of the follow-up appointment varied with the condition being treated. For instance, prisoners with an acute flare of eczema treated with a topical steroid were reviewed wherever possible after seven days. In contrast, prisoners with acne were reviewed after eight weeks. The data were collected over a six-month period. All prisoners were assured of the anonymity and confidentiality of the information that they provided. One hundred and eighty-one prisoners were asked to complete the questionnaire in the waiting area of the health care centre after their appointment and to seal the completed form in the envelope provided and hand it back to the pharmacist before leaving. A total of 106 prisoners (59 per cent) who were seen agreed to complete a questionnaire.
Results
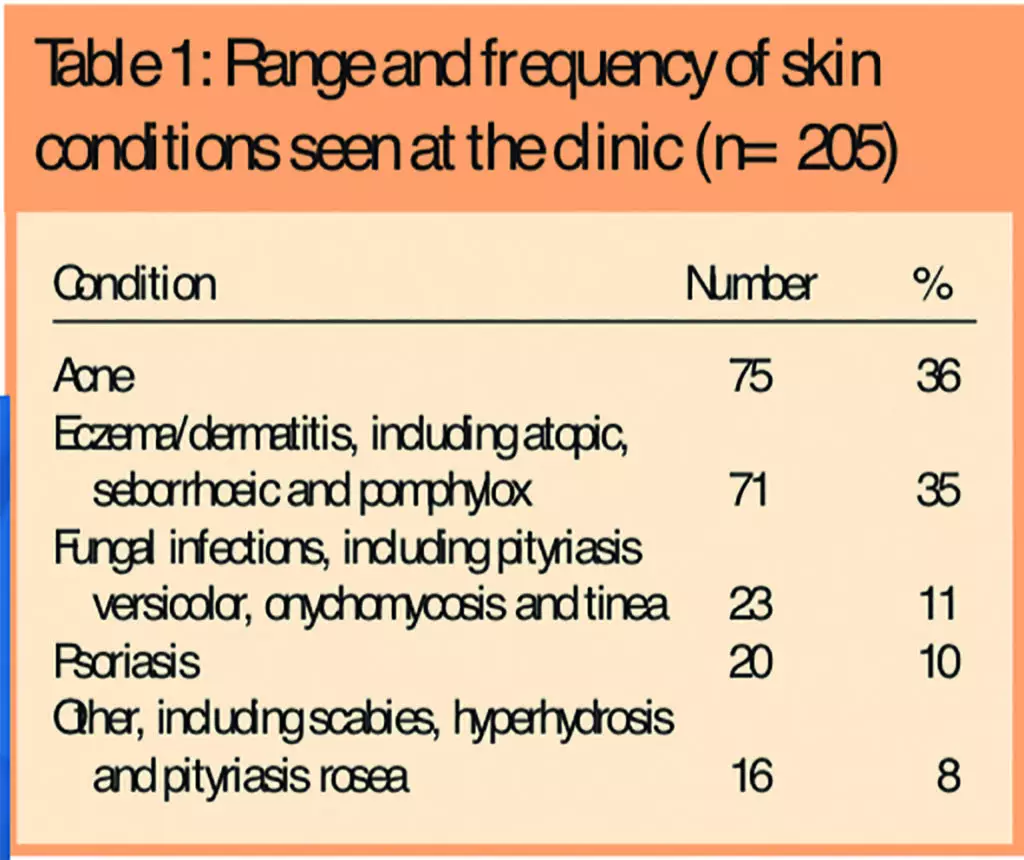
The range and frequency of conditions seen at the clinics are shown in Table 1.
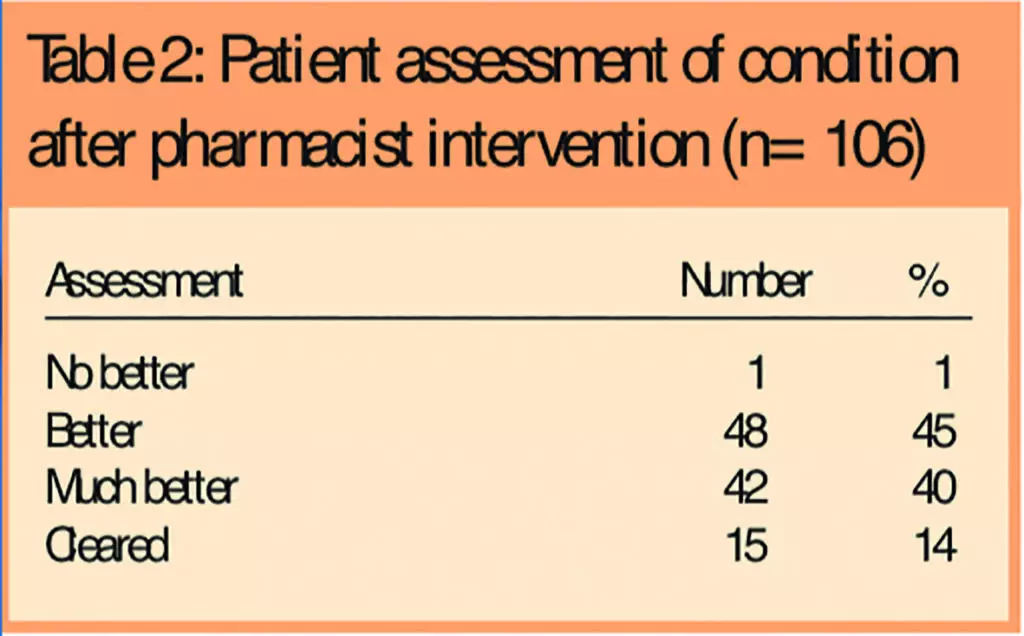
Prisoners were asked to rate their condition after treatment from the pharmacist and the results are given in Table 2, which shows that 85 per cent of respondents (90/106) reported that their condition was “better” or “much better” after treatment.
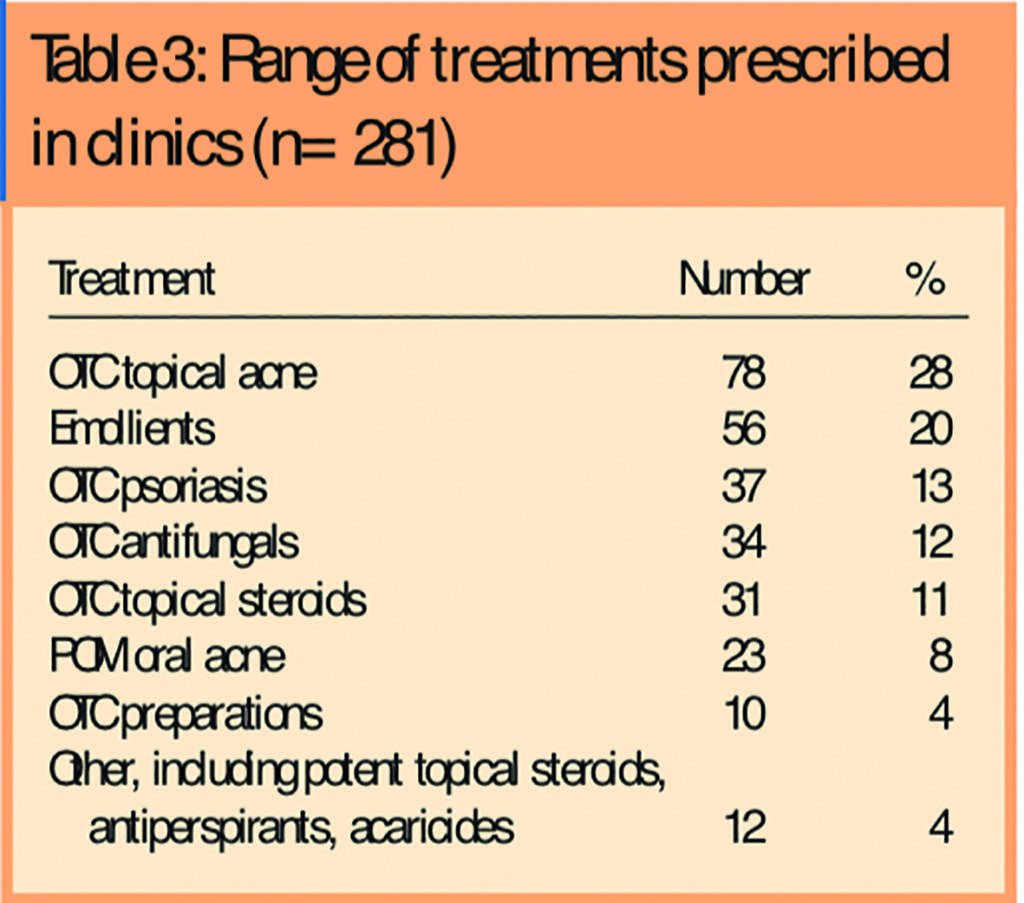
A number of different treatments were used and these have been broadly categorised as outlined in Table 3, which shows that most treatments issued are already available over the counter. When asked if they would return to see the pharmacist with the same problem, 98 per cent of respondents (104/106) said they would. Furthermore, when asked if they would return to see the pharmacist with a different skin problem, 97 per cent (103/106) said they would.
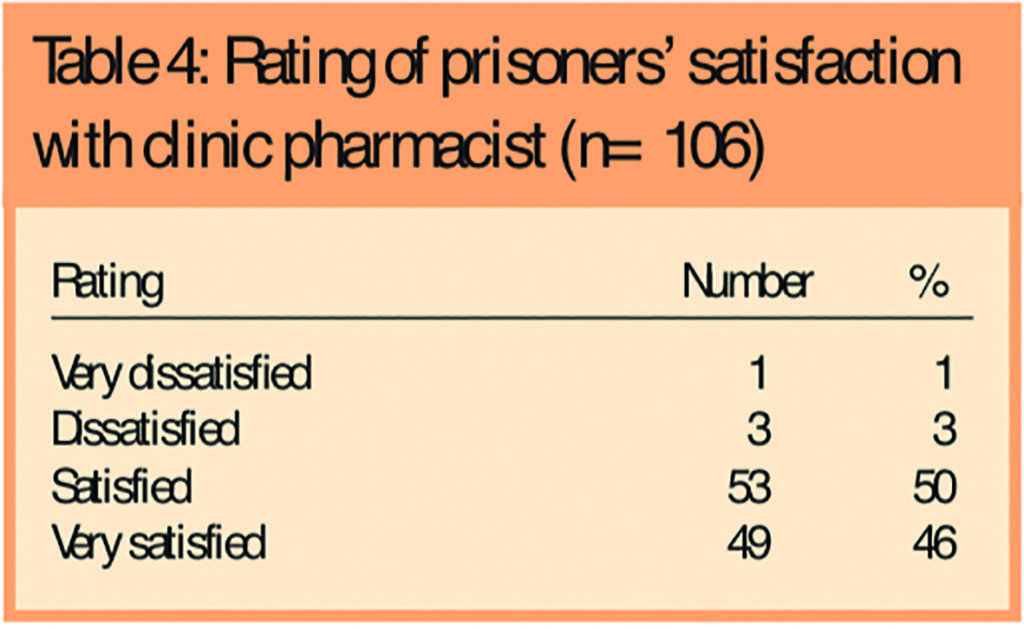
Respondents were then asked to rate their level of satisfaction with the advice they received from the pharmacist on a scale of 1–4, where 1 represented “very dissatisfied” and 4 represented “very satisfied”. The results are shown in Table 4, from which it can be seen that 96 per cent (99/106) were satisfied with the advice that they received.
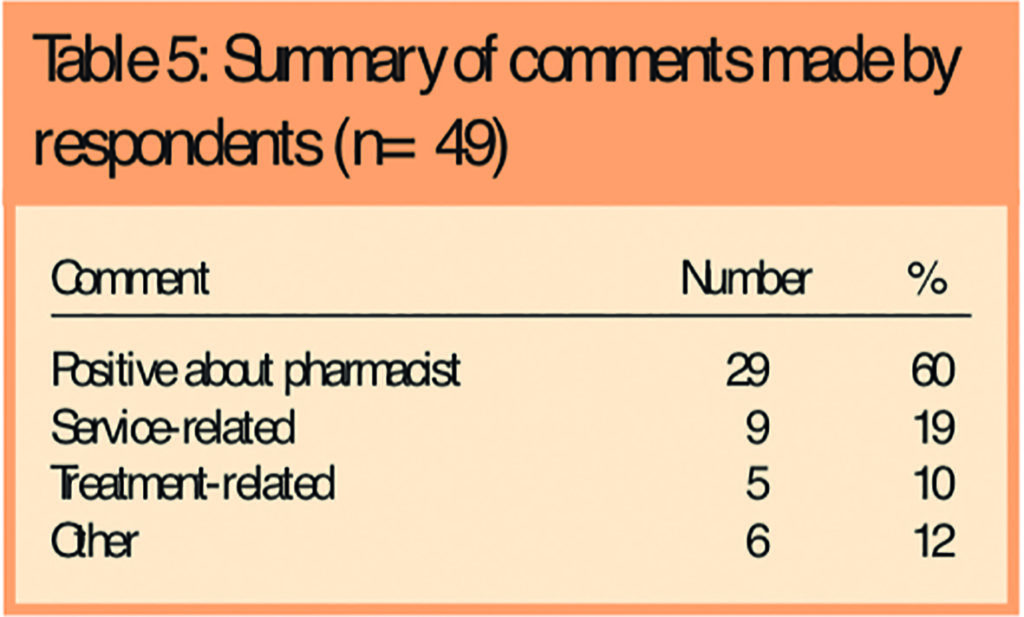
A final question asked whether or not prisoners had gained a better understanding of their condition and 97 per cent (103/106) said they had. Prisoners were then invited to add any comments. Forty-four per cent of respondents (47/106) made comments or remarks. The comments were categorised as shown in Table 5, which shows that 62 per cent (29/47) were positive about the pharmacist.
Discussion
The results from this small study show that the prisoners sampled were satisfied with the services and advice provided by the pharmacist.
All prisoners who were seen had self-referred and had not necessarily been seen by a medical practitioner before coming to the clinic. Consequently, there was no independent verification of their diagnosis by a medical practitioner. Nevertheless, the results in Table 2 show that most prisoners rated their condition as either “better” or “much better”. This lends support to the notion that the pharmacist was probably able accurately to diagnose the problem or at least provide suitable treatment in the majority of cases. Moreover, as shown in Table 3, most of the topical therapies used are already available for pharmacists to sell over the counter.
The positive response to the questions on whether or not prisoners would return to see the pharmacist with the same or other another skin condition suggest a high degree of satisfaction with the pharmacist. The response to the final question shows the potential benefits for the role of pharmacists in educating patients about their skin condition and its treatment. Analysis of the comments provided by prisoners gave some insight into their thoughts about the pharmacist and the services provided and four examples are given in the Panel.
Panel: Some prisoners’ comments on the dermatology clinic
- I found this clinic helpful and informative and would use it again in future
- Since seeing the dermatology [sic] he hastrete [sic] me well and dos [sic] a good job and understands
- I was given very useful information and it has helped me understand my skin condition better and I know how to control it also if it comes back
- I had been to the Dr outside prison and they did not help me as much as the prison clinics which I am very grateful
As the study is unique there is little with which to compare the results. Some evidence on the frequency of dermatological problems in American prisons has been reviewed by Brauner.8 However, as these results were based on two studies between 1976 and 1983 and comparison of the incidence of skin conditions with the those in the present study may not be relevant because of differences between the two penal systems. Furthermore, little is known about the health-seeking advice of males with skin problems in the community. Nevertheless, there is some evidence demonstrating that prisoners consult as much as six times more frequently than a demographically equivalent community population,9 although this study did not address the range of presenting conditions.
Although the results of this small study are generally favourable, the study suffers from a number of limitations. Since many skin conditions are chronic there will inevitably be some improvement in the condition irrespective of the treatments used. Therefore, it is difficult to be sure whether or not a prisoner’s condition would have improved irrespective of the intervention of the pharmacist. The timescale for the review appointments tried to reduce, but could not completely eliminate, this natural variation. Secondly, as prisoners were invited to complete the questionnaire and hand it (albeit in a sealed envelope) to the pharmacist they had just consulted, they might have been concerned about the anonymity of the questionnaire, which might have influenced their replies. In an effort to reduce this potential confounding factor, prisoners were informed that the questionnaires would be sent away for independent analysis and that the pharmacist would not see their individual responses.
Literacy problems are often cited as being common in prisons but only two prisoners invited to complete a questionnaire stated that they were unable to do so because of illiteracy. Indeed, many of the comments recorded (see Panel for examples) illustrate a low level of literacy among prisoners. However, at the piloting stage, there were no reported problems with understanding the questions.
The questionnaire did not use any recognised assessment tools (such as an acne grading scale) to assess prisoners’ response to treatment because of the problem of correlating the change in symptom severity with the subjective impression of the patient. In practice such correlations can be difficult since the clinical severity of a condition does not necessarily reflect the psychological impact upon the patient. Consequently, the assessment of the degree of improvement was left to the patients themselves.
Conclusion
The results of the survey demonstrate that prisoners were generally happy to consult a pharmacist about their skin problems. They also gained a better understanding of their condition and how to manage it after visiting the clinics and made positive comments about the pharmacist.
The study has also revealed that most prisoners could be successfully treated with products that are already available to pharmacists. Consequently, it would be useful if pharmacists with a special interest in dermatology could establish primary care-based clinics to assess and treat patients with skin problems.
As noted in Table 1, 81 per cent of all consultations were for only three commonly occurring conditions and most pharmacists would already have the necessary training and experience to manage such patients. The study has also revealed how patients gained a greater understanding of their condition. Therefore another potentially valuable role for pharmacists would be as educators, informing patients not only about their skin problem but also about how to use topical therapies.
Finally, with many primary care organisations operating minor ailments schemes through community pharmacies, if such schemes were expanded to include chronic conditions such as acne and psoriasis, then this would allow pharmacists to take a more active role in the management of these common skin conditions.
About the author
Rod Tucker, PhD, MRPharmS was chief pharmacist at HMP Moorland.
He is now at Pharmacy Department, HMP Hull, Hedon Road, Hull HU5 9LS (e-mail rod.tucker@hmps.gsi.gov.uk)
References
- NHS Modernisation Agency. Action on dermatology. London: Department of Health; 2003.
- Rea, JN, Newhouse, ML, Halil, T. Skin diseases in Lambeth. A community study of prevalence and use of medical care. British Journal of Preventative and Social Medicine 1976;30:107–14.
- All Party Parliamentary Group on Skin.Report on the enquiry into the impact of skin diseases on people’s lives. London: All Party Parliamentary Group on Skin; 2003.
- Azzopardi LM, Serracino IA, Zarb Adami M, Salek S. Pharmacists’ intervention improves management of skin conditions. Pharmacy World and Science. 2000;22:175.
- Mallon E, Newton JN, Klassen A, Stewart-Brown SL, Ryan TJ, Finlay AY. The quality of life in acne: a comparison with general medical conditions using generic questionnaires. British Journal of Dermatology 1999;140:672–6.
- Tucker RP. Pharmacist-led dermatology clinics can improve prisoners’ quality of life. Pharmaceutical Journal 2004;272: 577–9.
- Tucker RP. Exploring prisoners’ views of a pharmacy-led dermatology clinic. Pharmacy in Practice. 2004;4:113–14.
- Brauner GJ, Goodheart HP, Dermatologic care behind bars. Journal of the American Academy of Dermatology 1988; 18:1066–73.
- Marshall T, Simpson S, Stevens A. Use of health services by prison inmates: comparisons with the community. Journal of Epidemiology and Community Health 2001;55:364–5.


