Allergic rhinitis (AR) is a common inflammatory nasal condition that affects 10–15% of children and 26% of adults in the UK1. It impacts school attendance and performance in examinations and at work, as well affecting quality of life by disrupting sleep. It is also a risk factor for the development of asthma.
Some people are more prone to allergic rhinitis than others. Risk factors include:
- A family history of allergies;
- Young age — allergies are more common in children;
- Already having an allergic condition, such as eczema or asthma;
- Being exposed to smoke, pollution and other allergens.
Common allergens
Allergic rhinitis occurs when the body mistakes a normally harmless substance for something harmful — called an allergen — and mounts an immune response, which causes nasal and ocular symptoms.
Allergens fall into two main categories:
- Seasonal allergens, such as pollen, which tend to be present outside of the home;
- Perennial allergens, such as house dust mites and pet dander, which are more common within the home.
Occupational allergens, such as chemicals, dust and flour, can also trigger allergic rhinitis in some individuals.
Symptoms can be intermittent (less than four days per week or for less than four consecutive weeks) or persistent (more than four days per week and for more than four consecutive weeks)2.
The presence of seasonal allergens can vary across the UK. For example, the pollen season starts later and is shorter in the north of the country; and urban areas tend to have lower pollen counts than rural areas.
Pollen seasons and counts are also affected by temperature, rainfall, wind and sunshine. Recent research suggests that, with rising temperatures from climate change, pollen seasons may start earlier, meaning that some allergy sufferers could begin to experience hay fever as early as January or February3.
However, as a general guide, the following figure indicates the presence of allergens throughout the year (see Figure 1).
Allergic response
An allergic reaction involves three stages: sensitisation, when the susceptible person first encounters the allergen; the early-phase allergic response, which happens within minutes of re-exposure to the allergen; and the late-phase response, which occurs over the next 6–12 hours4.
Symptoms
Common symptoms of allergic rhinitis can range from mild to severe and may include nasal and ocular symptoms5. Patients should be asked about the type, frequency, severity and persistence of symptoms and where they experience them.
Managing symptoms
There are several actions that people can take to try to reduce mild-to-moderate symptoms of allergic rhinitis, including nasal irrigation with saline and practising allergen avoidance strategies (see Box 1).
Box 1: Allergen avoidance techniques
Pollen allergy
- Avoid walking in grassy, open spaces, particularly during early morning, early evening and during mowing, when the pollen count is high;
- Avoid drying washing outdoors when the pollen count is high;
- Keep windows shut in cars and buildings when the pollen count is high;
- Shower, wash hair and change clothes following high pollen exposures;
- Wear wraparound sunglasses and consider using nasal barriers, such as petroleum jelly, when the pollen count is high;
- Vacuum regularly using a vacuum cleaner with a good filter and dust with a damp cloth.
Dust mite allergy
- Fit mattresses, pillows, and duvets with house dust mite impermeable covers however these are unlikely to be effective on their own;
- Reduce humidity by increasing ventilation;
- Wash all bedding and furry toys at high temperatures, and dust surfaces with a damp cloth, at least once a week;
- Remove carpets, rugs and soft furnishings in the bedroom if possible — wooden or hard floor surfaces are preferred.
- Vacuum hard floors regularly using a vacuum cleaner with a good filter.
Pet allergy
- Ideally do not allow pets in the home or, if this is not possible, restrict them to defined areas;
- Do not allow pets in bedrooms;
- Remove carpets and rugs from the rooms where pets are kept, if possible;
- Regularly wash pets and any surfaces they are in contact with;
- Vacuum regularly using a vacuum cleaner with a good filter.
Source: NICE CKS; NHS; patient.info
Patients should trial avoidance strategies and consider pharmacological options if symptoms persist or are moderate to severe.
Pharmacological options vary depending on patient preference, age, and the severity and persistence of their symptoms. If nasal or ocular symptoms predominate, topical treatments may be more effective. However, some people may prefer to take an oral product5.
Antihistamines can be taken either to treat or prevent symptoms. They act by binding to histamine H1 receptors, blocking the pro-inflammatory actions of histamine.
Older, first-generation antihistamines are not recommended for allergic rhinitis because they cross the blood-brain barrier and occupy H1 receptors throughout the central nervous system, which can impair alertness, cognition, memory and psychomotor performance, as well as causing sedation6. These older antihistamines can also block muscarinic, α-adrenergic, and serotonin receptors, as well as cardiac potassium ion channels, causing cardiovascular, urinary and gastrointestinal adverse reactions.
Second-generation antihistamines are more selective for H1 receptors and have lower brain permeability, so are less likely to cause adverse effects, such as sedation, and cognitive and psychomotor impairment. They also have a faster onset and longer duration of action7 (see Box 2).
Box 2: Oral antihistamines available over the counter
First-generation antihistamines:
- Chlorpheniramine
- Diphenhydramine
- Promethazine
Second-generation antihistamines:
- Acrivastine
- Cetirizine
- Fexofenadine
- Loratadine
Intranasal corticosteroids are available as drops and sprays and act locally to reduce inflammation.
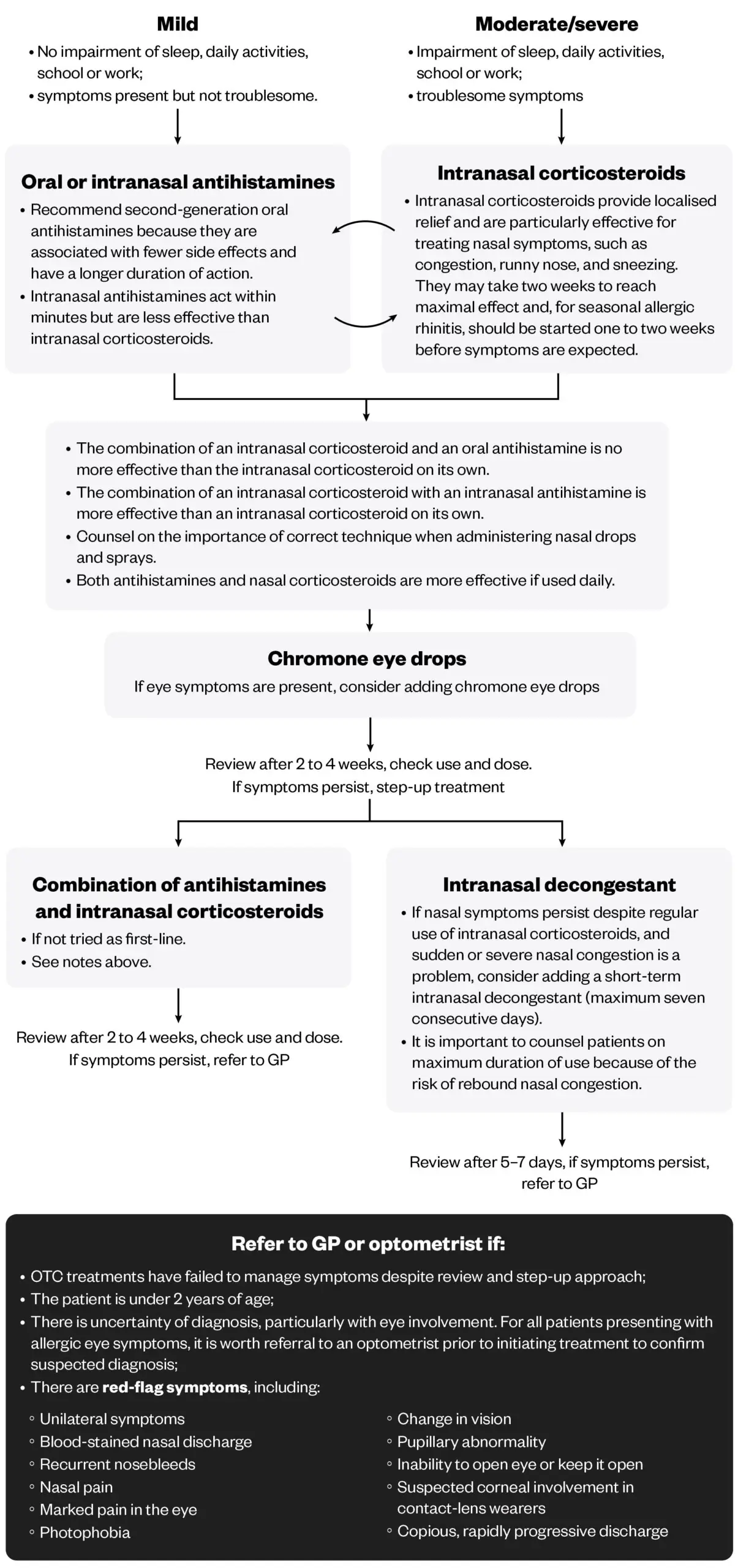
Both oral and intranasal antihistamines and intranasal corticosteroids are recommended as first-line treatments for allergic rhinitis in adults, either alone or in combination (see Figure 4). Intranasal antihistamines are only available via an independent prescriber or a patient group direction, or as part of an intranasal antihistamine/corticosteroid combination product that is classified as a pharmacy medicine5.
If ocular symptoms are present, sodium cromoglicate eye drops can be recommended. These work by stabilising mast cells, preventing the release of histamine and other mediators. Olapatadine eye drops are also available but are prescription-only medicines.
If nasal symptoms persist despite regular use of intranasal corticosteroids, and sudden or severe nasal congestion is a problem, short-term use of decongestants can be considered, which work by constricting the blood vessels in the nasal mucosa. However, there are several contraindications and cautions to these and rebound congestion can occur (see Figure 4).
Choice of treatments
Treatment choices will depend on the frequency and severity of symptoms and patient preference, as well as other patient specific factors, such as age, pregnancy and breastfeeding (see Figure 5), other medical conditions and existing medication (see Figure 6).
Editorial advisers: Sarah Denman, highly advanced clinical pharmacist — immunology and allergy, Leeds Teaching Hospital NHS Trust; Anna Matthews, independent prescriber and superintendent pharmacist at Nanty Pharmacy

For more information from Opella, visit: Allevia® Hayfever and Allergy Relief
- 1.Scadding GK, Kariyawasam HH, Scadding G, et al. <scp>BSACI</scp> guideline for the diagnosis and management of allergic and non‐allergic rhinitis (Revised Edition 2017; First edition 2007). Clin Experimental Allergy. 2017;47(7):856-889. doi:10.1111/cea.12953
- 2.Klimek L, Bachert C, Pfaar O, et al. ARIA guideline 2019: treatment of allergic rhinitis in the German health system. ALS. 2019;3(01):22-50. doi:10.5414/alx02120e
- 3.Lam HCY, Anees-Hill S, Satchwell J, et al. Association between ambient temperature and common allergenic pollen and fungal spores: A 52-year analysis in central England, United Kingdom. Science of The Total Environment. 2024;906:167607. doi:10.1016/j.scitotenv.2023.167607
- 4.Galli SJ, Tsai M, Piliponsky AM. The development of allergic inflammation. Nature. 2008;454(7203):445-454. doi:10.1038/nature07204
- 5.Allergic rhinitis: Scenario: Management. NICE Clinical Knowledge Summaries. January 2024. Accessed November 21, 2024. https://cks.nice.org.uk/topics/allergic-rhinitis/management/management/
- 6.Linton S, Hossenbaccus L, Ellis AK. Evidence-based use of antihistamines for treatment of allergic conditions. Annals of Allergy, Asthma & Immunology. 2023;131(4):412-420. doi:10.1016/j.anai.2023.07.019
- 7.Fein MN, Fischer DA, O’Keefe AW, Sussman GL. CSACI position statement: Newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for the treatment of allergic rhinitis and urticaria. Allergy Asthma Clin Immunol. 2019;15(1). doi:10.1186/s13223-019-0375-9
1 comment
You must be logged in to post a comment.





Great interactive presentation and all the important information can be found here. Thank you!